Abstract
Pregnant individuals with viral illness may experience significant morbidity and have higher rates of pregnancy and neonatal complications. With the growing number of viral infections and new viral pandemics, it is important to examine the effects of infection during pregnancy on both the gestational parent and the offspring. Febrile illness and inflammation during pregnancy are correlated with risk for autism, attention deficit/hyperactivity disorder, and developmental delay in the offspring in human and animal models. Historical viral epidemics had limited follow-up of the offspring of affected pregnancies. Infants exposed to seasonal influenza and the 2009 H1N1 influenza virus experienced increased risks of congenital malformations and neuropsychiatric conditions. Zika virus exposure in utero can lead to a spectrum of abnormalities, ranging from severe microcephaly to neurodevelopmental delays which may appear later in childhood and in the absence of Zika-related birth defects. Vertical infection with severe acute respiratory syndrome coronavirus-2 has occurred rarely, but there appears to be a risk for developmental delays in the infants with antenatal exposure. Determining how illness from infection during pregnancy and specific viral pathogens can affect pregnancy and neurodevelopmental outcomes of offspring can better prepare the community to care for these children as they grow.
Impact
-
Viral infections have impacted pregnant people and their offspring throughout history.
-
Antenatal exposure to maternal fever and inflammation may increase risk of developmental and neurobehavioral disorders in infants and children.
-
The recent SARS-CoV-2 pandemic stresses the importance of longitudinal studies to follow pregnancies and offspring neurodevelopment.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 14 print issues and online access
$259.00 per year
only $18.50 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Liu, H. et al. Why are pregnant women susceptible to COVID-19? An immunological viewpoint. J. Reprod. Immunol. 139, 103122 (2020).
Mor, G., Aldo, P. & Alvero, A. B. The unique immunological and microbial aspects of pregnancy. Nat. Rev. Immunol. 17, 469–482 (2017).
Jamieson, D. J., Theiler, R. N. & Rasmussen, S. A. Emerging infections and pregnancy. Emerg. Infect. 12, 1638–1643 (2006).
Fortin, O. & Mulkey, S. B. Neurodevelopmental outcomes in congenital and perinatal infections. Curr. Opin. Infect. Dis. 36, 405–413 (2023).
Shuid, A. N. et al. Association between viral infections and risk of autistic disorder: an overview. Int. J. Environ. Res. Public. Health 18, 2817 (2021).
Hosier, H. et al. SARS-CoV-2 infection of the placenta. J. Clin. Invest. 130, 4947–4953 (2020).
Dong, L. et al. Possible vertical transmission of SARS-CoV-2 from an infected mother to her newborn. JAMA 323, 1846–1848 (2020).
Pulinx, B. et al. Vertical transmission of SARS-CoV-2 infection and preterm birth. Eur. J. Clin. Microbiol. Infect. Dis. 39, 2441–2445 (2020).
Zeng, H. et al. Antibodies in infants born to mothers with COVID-19 pneumonia. JAMA 323, 1848–1849 (2020).
Zaigham, M. et al. Clinical-pathological features in placentas of pregnancies with SARS-CoV-2 infection and adverse outcome: case series with and without congenital transmission. BJOG Int. J. Obstet. Gynaecol. 129, 1361–1374 (2022).
Atladóttir, H. Ó. et al. Maternal infection requiring hospitalization during pregnancy and autism spectrum disorders. J. Autism Dev. Disord. 40, 1423–1430 (2010).
Atladóttir, H. Ó., Henriksen, T. B., Schendel, D. E. & Parner, E. T. Autism after infection, febrile episodes, and antibiotic use during pregnancy: an exploratory study. Pediatrics 130, e1447–e1454 (2012).
Bohmwald, K., Andrade, C. A. & Kalergis, A. M. Contribution of pro-inflammatory molecules induced by respiratory virus infections to neurological disorders. Pharmaceuticals 14, 340 (2021).
Zimmer, A., Youngblood, A., Adnane, A., Miller, B. J. & Goldsmith, D. R. Prenatal exposure to viral infection and neuropsychiatric disorders in offspring: a review of the literature and recommendations for the COVID-19 pandemic. Brain. Behav. Immun. 91, 756–770 (2021).
Zerbo, O. et al. Maternal infection during pregnancy and autism spectrum disorders. J. Autism Dev. Disord. 45, 4015–4025 (2015).
Shi, L., Tu, N. & Patterson, P. H. Maternal influenza infection is likely to alter fetal brain development indirectly: the virus is not detected in the fetus. Int. J. Dev. Neurosci. 23, 299–305 (2005).
Patterson, P. H. Immune involvement in schizophrenia and autism: etiology, pathology and animal models. Behav. Brain Res. 204, 313–321 (2009).
Mednick, S. A., Machon, R. A., Huttunen, M. O. & Bonett, D. Adult schizophrenia following prenatal exposure to an influenza epidemic. Arch. Gen. Psychiatry 45, 189–192 (1988).
Brown, A. S. et al. Serologic evidence for prenatal influenza in the etiology of schizophrenia. Abstr. IXth Int. Congr. Schizophr. Res. 60, 34 (2003).
Edwards, M. J., Saunders, R. D. & Shiota, K. Effects of heat on embryos and foetuses. Int. J. Hyperth. 19, 295–324 (2003).
Dreier, J. W., Andersen, A.-M. N. & Berg-Beckhoff, G. Systematic review and meta-analyses: fever in pregnancy and health impacts in the offspring. Pediatrics 133, e674–e688 (2014).
Zerbo, O. et al. Is maternal influenza or fever during pregnancy associated with autism or developmental delays? results from the CHARGE (CHildhood Autism Risks from Genetics and Environment) study. J. Autism Dev. Disord. 43, 25–33 (2013).
Croen, L. A. et al. Infection and fever in pregnancy and autism spectrum disorders: findings from the study to explore early development. Autism Res. 12, 1551–1561 (2019).
Holst, C., Jørgensen, S. E., Wohlfahrt, J., Nybo Andersen, A.-M. & Melbye, M. Fever during pregnancy and motor development in children: a study within the Danish National Birth Cohort. Dev. Med. Child Neurol. 57, 725–732 (2015).
Currenti, S. A. Understanding and determining the etiology of autism. Cell. Mol. Neurobiol. 30, 161–171 (2010).
Hornig, M. et al. Prenatal fever and autism risk. Mol. Psychiatry 23, 759–766 (2018).
Ács, N., Bánhidy, F., Puhó, E. & Czeizel, A. E. Maternal influenza during pregnancy and risk of congenital abnormalities in offspring. Birth Defects Res. A. Clin. Mol. Teratol. 73, 989–996 (2005).
Martin, R. P. & Dombrowski, S. C. Prenatal Exposures: Psychological and Educational Consequences for Children. xiii, 284 (Springer Science + Business Media, New York, NY, US, 2008).
Graham, J. M. Jr., Edwards, M. J. & Edwards, M. J. Teratogen update: gestational effects of maternal hyperthermia due to febrile illnesses and resultant patterns of defects in humans. Teratology 58, 209–221 (1998).
Fang, S.-Y., Wang, S., Huang, N., Yeh, H.-H. & Chen, C.-Y. Prenatal infection and autism spectrum disorders in childhood: a population-based case-control study in Taiwan. Paediatr. Perinat. Epidemiol. 29, 307–316 (2015).
Patterson, P. H. Maternal infection and immune involvement in autism. Trends Mol. Med. 17, 389–394 (2011).
Abdallah, M. W. et al. Amniotic fluid inflammatory cytokines: potential markers of immunologic dysfunction in autism spectrum disorders. World J. Biol. Psychiatry 14, 528–538 (2013).
Goines, P. E. et al. Increased midgestational IFN-γ, IL-4 and IL-5 in women bearing a child with autism: a case-control study. Mol. Autism 2, 13 (2011).
Gustavson, K. et al. Maternal fever during pregnancy and offspring attention deficit hyperactivity disorder. Sci. Rep. 9, 9519 (2019).
Werenberg Dreier, J. et al. Fever and infections in pregnancy and risk of attention deficit/hyperactivity disorder in the offspring. J. Child Psychol. Psychiatry 57, 540–548 (2016).
Dreier, J. W., Berg-Beckhoff, G., Andersen, P. K. & Andersen, A.-M. N. Prenatal exposure to fever and infections and academic performance: a multilevel analysis. Am. J. Epidemiol. 186, 29–37 (2017).
Collier, S. A., Rasmussen, S. A., Feldkamp, M. L. & Honein, M. A. Prevalence of self-reported infection during pregnancy among control mothers in the National Birth Defects Prevention Study. Birth Defects Res. A. Clin. Mol. Teratol. 66, 193–201 (2009).
Cordeiro, C. N., Tsimis, M. & Burd, I. Infections and brain development. Obstet. Gynecol. Surv. 70, 644–655 (2015).
Estes, M. L. & McAllister, A. K. Maternal TH17 cells take a toll on baby’s brain. Science 351, 919–920 (2016).
Deverman, B. E. & Patterson, P. H. Cytokines and CNS development. Neuron 64, 61–78 (2009).
Meyer, U. et al. The time of prenatal immune challenge determines the specificity of inflammation-mediated brain and behavioral pathology. J. Neurosci. 26, 4752–4762 (2006).
Meyer, U., Yee, B. K. & Feldon, J. The neurodevelopmental impact of prenatal infections at different times of pregnancy: the earlier the worse? Neuroscientist 13, 241–256 (2007).
Jones, K. L. et al. Autism with intellectual disability is associated with increased levels of maternal cytokines and chemokines during gestation. Mol. Psychiatry 22, 273–279 (2017).
Dozmorov, M. G. et al. Associations between maternal cytokine levels during gestation and measures of child cognitive abilities and executive functioning. Brain. Behav. Immun. 70, 390–397 (2018).
Gabay, C. & Kushner, I. Acute-phase proteins and other systemic responses to inflammation. N. Engl. J. Med. 340, 448–454 (1999).
Brown, A. S. et al. Elevated maternal C-reactive protein and autism in a national birth cohort. Mol. Psychiatry 19, 259–264 (2014).
Wong, S. F., Chow, K. M. & de Swiet, M. Severe acute respiratory syndrome and pregnancy. BJOG Int. J. Obstet. Gynaecol. 110, 641–642 (2003).
Wong, S. F. et al. Pregnancy and perinatal outcomes of women with severe acute respiratory syndrome. Am. J. Obstet. Gynecol. 191, 292–297 (2004).
Lam, C. M. et al. A case-controlled study comparing clinical course and outcomes of pregnant and non-pregnant women with severe acute respiratory syndrome. BJOG Int. J. Obstet. Gynaecol. 111, 771–774 (2004).
Ng, P. C., Leung, C. W., Chiu, W. K., Wong, S. F. & Hon, E. K. L. SARS in newborns and children. Biol. Neonate 85, 293–298 (2004).
Li, A. M. & Ng, P. C. Severe acute respiratory syndrome (SARS) in neonates and children. Arch. Dis. Child. Fetal Neonatal Ed. 90, F461 (2005).
Di Mascio, D. et al. Outcome of coronavirus spectrum infections (SARS, MERS, COVID-19) during pregnancy: a systematic review and meta-analysis. Am. J. Obstet. Gynecol. MFM 2, 100107 (2020).
Alfaraj, S. H., Al-Tawfiq, J. A. & Memish, Z. A. Middle East Respiratory Syndrome Coronavirus (MERS-CoV) infection during pregnancy: Report of two cases & review of the literature. J. Microbiol. Immunol. Infect. 52, 501–503 (2019).
Silasi, M. et al. Viral infections during pregnancy. Am. J. Reprod. Immunol. 73, 199–213 (2015).
Kwon, J.-Y., Romero, R. & Mor, G. New Insights into the relationship between viral infection and pregnancy complications. Am. J. Reprod. Immunol. 71, 387–390 (2014).
Kourtis, A. P., Read, J. S. & Jamieson, D. J. Pregnancy and infection. N. Engl. J. Med. 370, 2211–2218 (2014).
Neuzil, K. M., Reed, G. W., Mitchel, E. F., Simonsen, L. & Griffin, M. R. Impact of influenza on acute cardiopulmonary hospitalizations in pregnant women. Am. J. Epidemiol. 148, 1094–1102 (1998).
Jamieson, D. J. et al. H1N1 2009 influenza virus infection during pregnancy in the USA. Lancet 374, 451–458 (2009).
Harris, J. W. Influenza occurring in pregnant women: a statistical study of thirteen hundred and fifty cases. J. Am. Med. Assoc. 72, 978–980 (1919).
Nuzum, J. W., Pilot, I., Stangl, F. H. & Bonar, B. E. Pandemic influenza and pneumonia in a large civil hospital. J. Am. Med. Assoc. 71, 1562–1565 (1918).
Freeman, D. W. & Barno, A. Deaths from Asian influenza associated with pregnancy. Am. J. Obstet. Gynecol. 78, 1172–1175 (1959).
Louie, J. K., Acosta, M., Jamieson, D. J., Honein, M. A. & Group, C. P. (H1N1) W. severe 2009 H1N1 influenza in pregnant and postpartum women in California. N. Engl. J. Med. 362, 27–35 (2010).
Mosby, L. G., Rasmussen, S. A. & Jamieson, D. J. 2009 pandemic influenza A (H1N1) in pregnancy: a systematic review of the literature. Am. J. Obstet. Gynecol. 205, 10–18 (2011).
Pierce, M., Kurinczuk, J. J., Spark, P., Brocklehurst, P. & Knight, M. Perinatal outcomes after maternal 2009/H1N1 infection: national cohort study. BMJ 342, d3214 (2011).
Borren, I. et al. Early prenatal exposure to pandemic influenza A (H1N1) infection and child psychomotor development at 6 months—A population-based cohort study. Early Hum. Dev. 122, 1–7 (2018).
Rasmussen, S. A., Jamieson, D. J. & Uyeki, T. M. Effects of influenza on pregnant women and infants. Am. J. Obstet. Gynecol. 207, S3–S8 (2012).
Deykin, E. Y. & Macmahon, B. Viral exposure and autism. Am. J. Epidemiol. 109, 628–638 (1979).
Zerbo, O. et al. Association between influenza infection and vaccination during pregnancy and risk of autism spectrum disorder. JAMA Pediatr. 171, e163609–e163609 (2017).
Dassa, D., Takei, N., Sham, P. C. & Murray, R. M. No association between prenatal exposure to influenza and autism. Acta Psychiatr. Scand. 92, 145–149 (1995).
Mueller, F. S. et al. Influence of poly(I:C) variability on thermoregulation, immune responses and pregnancy outcomes in mouse models of maternal immune activation. Brain. Behav. Immun. 80, 406–418 (2019).
Malkova, N. V., Yu, C. Z., Hsiao, E. Y., Moore, M. J. & Patterson, P. H. Maternal immune activation yields offspring displaying mouse versions of the three core symptoms of autism. Brain. Behav. Immun. 26, 607–616 (2012).
Shi, L., Fatemi, S. H., Sidwell, R. W. & Patterson, P. H. Maternal influenza infection causes marked behavioral and pharmacological changes in the offspring. J. Neurosci. 23, 297 (2003).
Dunaevsky, A. & Bergdolt, L. Brain changes in a maternal Immune activation model of neurodevelopmental brain disorders. Prog. Neurobiol. 175, 1–19 (2019).
Smith, S. E. P., Li, J., Garbett, K., Mirnics, K. & Patterson, P. H. Maternal immune activation alters fetal brain development through interleukin-6. J. Neurosci. 27, 10695 (2007).
Rasmussen, J. M. et al. Maternal Interleukin-6 concentration during pregnancy is associated with variation in frontolimbic white matter and cognitive development in early life. NeuroImage 185, 825–835 (2019).
Ozaki, K. et al. Maternal immune activation induces sustained changes in fetal microglia motility. Sci. Rep. 10, 21378 (2020).
Choi, G. B. et al. The maternal interleukin-17a pathway in mice promotes autism-like phenotypes in offspring. Science 351, 933–939 (2016).
Machado, C. J., Whitaker, A. M., Smith, S. E. P., Patterson, P. H. & Bauman, M. D. Maternal immune activation in nonhuman primates alters social attention in juvenile offspring. Biol. Psychiatry 77, 823–832 (2015).
Fatemi, S. H. et al. Prenatal viral infection leads to pyramidal cell atrophy and macrocephaly in adulthood: implications for genesis of autism and schizophrenia. Cell. Mol. Neurobiol. 22, 25–33 (2002).
Short, S. J. et al. Maternal influenza infection during pregnancy impacts postnatal brain development in the rhesus monkey. Biol. Psychiatry 67, 965–973 (2010).
Corradini, I. et al. Maternal immune activation delays excitatory-to-inhibitory gamma-aminobutyric acid switch in offspring. Biol. Psychiatry 83, 680–691 (2018).
Basil, P. et al. Prenatal maternal immune activation causes epigenetic differences in adolescent mouse brain. Transl. Psychiatry 4, e434–e434 (2014).
Richetto, J. et al. Genome-wide DNA methylation changes in a mouse model of infection-mediated neurodevelopmental disorders. Genet. Epigenetic Risks Autism Spectr. Disord. 81, 265–276 (2017).
Shrestha, S. & Offer, S. M. Epigenetic regulations of GABAergic neurotransmission: relevance for neurological disorders and epigenetic therapy. Med. Epigenetics 4, 1–19 (2016).
Hill, R. A. et al. Maternal SARS-CoV-2 exposure alters infant DNA methylation. Brain Behav. Immun. - Health 27, 100572 (2022).
Fujita, Y., Ishima, T. & Hashimoto, K. Supplementation with D-serine prevents the onset of cognitive deficits in adult offspring after maternal immune activation. Sci. Rep. 6, 37261 (2016).
Zhang, J., Jing, Y., Zhang, H., Bilkey, D. K. & Liu, P. Maternal immune activation altered microglial immunoreactivity in the brain of postnatal day 2 rat offspring. Synapse 73, e22072 (2019).
Scher, M. S. “The first thousand days” define a fetal/neonatal neurology program. Front. Pediatr. 9, 683138 (2021).
Huntley, M. A. et al. Genome-wide analysis of differential gene expression and splicing in excitatory neurons and interneuron subtypes. J. Neurosci. 40, 958–973 (2020).
Katsarou, A., Moshé, S. L. & Galanopoulou, A. S. Interneuronopathies and their role in early life epilepsies and neurodevelopmental disorders. Epilepsia Open 2, 284–306 (2017).
Molnár, Z. et al. New insights into the development of the human cerebral cortex. J. Anat. 235, 432–451 (2019).
Para, R. et al. The distinct immune nature of the fetal inflammatory response syndrome type I and type II. ImmunoHorizons 5, 735–751 (2021).
Jung, E. et al. The fetal inflammatory response syndrome: the origins of a concept, pathophysiology, diagnosis, and obstetrical implications. Semin. Fetal Neonatal Med. 25, 101146 (2020).
Kim, C. J. et al. Acute chorioamnionitis and funisitis: definition, pathologic features, and clinical significance. Am. J. Obstet. Gynecol. 213, S29–S52 (2015).
Lee, J. et al. Characterization of the fetal blood transcriptome and proteome in maternal anti‐fetal rejection: evidence of a distinct and novel type of human fetal systemic inflammatory response. Am. J. Reprod. Immunol. 70, 265–284 (2013).
COVID Data Tracker. Centers for Disease Control and Prevention https://covid.cdc.gov/covid-data-tracker (2020).
Rasmussen, S. A. et al. Pandemic influenza and pregnant women: summary of a meeting of experts. Am. J. Public Health 99, S248–S254 (2009).
Narang, K. et al. SARS-CoV-2 infection and COVID-19 during pregnancy: a multidisciplinary review. Mayo Clin. Proc. 95, 1750–1765 (2020).
Villar, J. et al. Maternal and neonatal morbidity and mortality among pregnant women with and without COVID-19 infection: the INTERCOVID multinational cohort study. JAMA Pediatr. 175, 817–826 (2021).
Kumar, R. et al. SARS-CoV-2 infection during pregnancy and pregnancy-related conditions: concerns, challenges, management and mitigation strategies–a narrative review. J. Infect. Public Health 14, 863–875 (2021).
Zambrano, L. D. et al. Morbidity and mortality weekly report update: characteristics of symptomatic women of reproductive age with laboratory-confirmed SARS-CoV-2 infection by pregnancy status. Cent. Dis. Control MMWR Morb. Mortal. Wkly. Rep. 69, 1641–1647 (2020).
Allotey, J. et al. Clinical manifestations, risk factors, and maternal and perinatal outcomes of coronavirus disease 2019 in pregnancy: living systematic review and meta-analysis. BMJ 370, m3320 (2020).
Ellington, S. et al. Characteristics of women of reproductive age with laboratory-confirmed SARS-CoV-2 infection by pregnancy status—United States, January 22–June 7, 2020. MMWR Morb. Mortal. Wkly. Rep. 69, 769–775 (2020).
Piekos, S. N. et al. The effect of maternal SARS-CoV-2 infection timing on birth outcomes: a retrospective multicentre cohort study. Lancet Digit. Health 4, e95–e104 (2022).
Khalil, A. et al. SARS-CoV-2 infection in pregnancy: a systematic review and meta-analysis of clinical features and pregnancy outcomes. EClinicalMedicine 25, 100446 (2020).
Schwartz, D. A., Mulkey, S. B. & Roberts, D. J. SARS-CoV-2 placentitis, stillbirth, and maternal COVID-19 vaccination: clinical–pathologic correlations. Am. J. Obstet. Gynecol. 228, 261–269 (2023).
Strid, P. et al. Coronavirus disease 2019 (COVID-19) Severity Among Women of Reproductive Age With Symptomatic Laboratory-Confirmed Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) Infection by Pregnancy Status—United States, 1 January 2020–25 December 2021. Clin. Infect. Dis. 75, S317–S325 (2022).
Iuliano, A. D. et al. Trends in disease severity and health care utilization during the early omicron variant period compared with previous SARS-CoV-2 high transmission periods—United States, December 2020-January 2022. Cent. Dis. Control MMWR Morb. Mortal. Wkly. Rep. 71, 146–152 (2022).
Stock, S. J. et al. SARS-CoV-2 infection and COVID-19 vaccination rates in pregnant women in Scotland. Nat. Med. 28, 504–512 (2022).
Adhikari, E. H. et al. COVID-19 cases and disease severity in pregnancy and neonatal positivity associated with delta (B.1.617.2) and omicron (B.1.1.529) variant predominance. JAMA 327, 1500–1502 (2022).
Reyes-Lagos, J. J. et al. A translational perspective of maternal immune activation by SARS-CoV-2 on the potential prenatal origin of neurodevelopmental disorders: the role of the cholinergic anti-inflammatory pathway. Front. Psychol. 12, 614451 (2021).
Dubey, H., Sharma, R. K., Krishnan, S. & Knickmeyer, R. SARS-CoV-2 (COVID-19) as a possible risk factor for neurodevelopmental disorders. Front. Neurosci. 16, 1021721 (2022).
Granja, M. G. et al. SARS-CoV-2 infection in pregnant women: neuroimmune-endocrine changes at the maternal-fetal interface. Neuroimmunomodulation 28, 1–21 (2021).
Engert, V. et al. Severe brain damage in a moderate preterm infant as complication of post-COVID-19 response during pregnancy. Neonatology 118, 505–508 (2021).
Mulkey, S. B. et al. Neurodevelopment in infants with antenatal or early neonatal exposure to SARS-CoV-2. Early Hum. Dev. 175, 105694 (2022).
Edlow, A. G., Castro, V. M., Shook, L. L., Kaimal, A. J. & Perlis, R. H. Neurodevelopmental outcomes at 1 year in infants of mothers who tested positive for SARS-CoV-2 during pregnancy. JAMA Netw. Open 5, e2215787–e2215787 (2022).
Hessami, K. et al. COVID-19 pandemic and infant neurodevelopmental impairment: a systematic review and meta-analysis. JAMA Netw. Open 5, e2238941–e2238941 (2022).
Shuffrey, L. C. et al. Association of birth during the COVID-19 pandemic with neurodevelopmental status at 6 months in infants with and without in utero exposure to maternal SARS-CoV-2 infection. JAMA Pediatr. 176, e215563–e215563 (2022).
Ayed, M. et al. Neurodevelopmental outcomes of infants born to mothers with SARS-CoV-2 infections during pregnancy: a national prospective study in Kuwait. BMC Pediatr. 22, 319 (2022).
Lavallée, A. & Dumitriu, D. Low risk of neurodevelopmental impairment in the COVID-19 generation should not make researchers complacent. JAMA Netw. Open 5, e2238958–e2238958 (2022).
Firestein, M. R., Dumitriu, D., Marsh, R. & Monk, C. Maternal mental health and infant development during the COVID-19 pandemic. JAMA Psychiatry 79, 1040–1045 (2022).
Mulkey, S. B. Lessons learned in caring for newborns from one viral outbreak to the next. Pediatr. Res. 95, 416–417 (2023).
Celik, I. H., Ozkaya Parlakay, A. & Canpolat, F. E. Management of neonates with maternal prenatal coronavirus infection and influencing factors. Pediatr. Res. https://doi.org/10.1038/s41390-023-02855-0 (2023).
Lu, Y.-C. et al. Maternal psychological distress during the COVID-19 pandemic and structural changes of the human fetal brain. Commun. Med. 2, 47 (2022).
Halai, U.-A. et al. Maternal Zika virus disease severity, virus load, prior dengue antibodies, and their relationship to birth outcomes. Clin. Infect. Dis. 65, 877–883 (2017).
Honein, M. A. et al. Birth defects among fetuses and infants of US women with evidence of possible Zika virus infection during pregnancy. JAMA 317, 59–68 (2017).
Muller, W. J. & Mulkey, S. B. Lessons about early neurodevelopment in children exposed to ZIKV in utero. Nat. Med. 25, 1192–1193 (2019).
Moore, C. A. et al. Characterizing the pattern of anomalies in congenital Zika syndrome for pediatric clinicians. JAMA Pediatr. 171, 288–295 (2017).
França, G. V. A. et al. Congenital Zika virus syndrome in Brazil: a case series of the first 1501 livebirths with complete investigation. Lancet 388, 891–897 (2016).
Adebanjo, T. et al. Update: interim guidance for the diagnosis, evaluation, and management of infants with possible congenital Zika virus syndrome—United States, October 2017. Cent. Dis. Control MMWR Morb. Mortal. Wkly. Rep. 66, 1089–1099 (2017).
Mulkey, S. B. et al. Neurodevelopmental abnormalities in children with in utero Zika virus exposure without congenital Zika syndrome. JAMA Pediatr. 174, 269–276 (2020).
Marbán-Castro, E. et al. Zika virus infection in pregnant travellers and impact on childhood neurodevelopment in the first two years of life: A prospective observational study. Travel Med. Infect. Dis. 40, 101985 (2021).
Grant, R. et al. In utero Zika virus exposure and neurodevelopment at 24 months in toddlers normocephalic at birth: a cohort study. BMC Med. 19, 12 (2021).
Rice, M. E. et al. Vital signs: Zika-associated birth defects and neurodevelopmental abnormalities possibly associated with congenital Zika virus infection—U.S. Territories and freely associated states, 2018. Cent. Dis. Control MMWR Morb. Mortal. Wkly. Rep. 67, 858–867 (2018).
Hoen, B. et al. Pregnancy outcomes after ZIKV infection in French territories in the Americas. N. Engl. J. Med. 378, 985–994 (2018).
Nielsen-Saines, K. et al. Delayed childhood neurodevelopment and neurosensory alterations in the second year of life in a prospective cohort of ZIKV-exposed children. Nat. Med. 25, 1213–1217 (2019).
Wild, C. P. Complementing the genome with an “exposome”: the outstanding challenge of environmental exposure measurement in molecular epidemiology. Cancer Epidemiol. Biomark. Prev. 14, 1847–1850 (2005).
Tamiz, A. P., Koroshetz, W. J., Dhruv, N. T. & Jett, D. A. A focus on the neural exposome. Neuron 110, 1286–1289 (2022).
Scher, M. S. The neural exposome influences the preterm fetal-to-neonatal connectome. Pediatr. Res. 95, 9–11 (2023).
Scher, M. S. Fetal neurology: principles and practice with a life-course perspective. in Handbook of Clinical Neurology (eds. de Vries, L. S. & Glass, H. C.) vol. 162 1–29 (Elsevier, 2019).
Funding
Sarah B. Mulkey receives research support from the Eunice Kennedy Shriver National Institute of Child Health & Human Development of the National Institutes of Health (grant number R01HD102445 [PI: S.B.M.] and R01HD107140 [Co-I: S.B.M.]) for studies on Zika virus and SARS-CoV-2, respectively. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Author information
Authors and Affiliations
Contributions
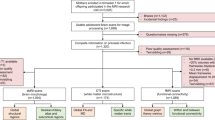
Emma F. Yates—Performed the literature review, received mentorship from Sarah B. Mulkey in writing a review manuscript, wrote initial draft of the manuscript, edited the manuscript with feedback from her mentor, edited the format of the manuscript for Pediatric Research, designed the figure for the manuscript, reviewed and approved the final version of the manuscript. Sarah B. Mulkey—Received study funding in viral exposures in pregnancy and child outcomes, developed the concept for the review manuscript, mentored Emma F. Yates in performing a literature review, provided critical review of the manuscript draft and edited drafts and revised versions, edited the figure, reviewed and approved the final version of the manuscript. Submitted the final version of the manuscript to Pediatric Research.
Corresponding author
Ethics declarations
Competing interests
Sarah B. Mulkey receives grant funding from the National Institutes of Health as described in funding. Sarah B. Mulkey and Emma F. Yates do not have conflicts of interest to disclose.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Yates, E.F., Mulkey, S.B. Viral infections in pregnancy and impact on offspring neurodevelopment: mechanisms and lessons learned. Pediatr Res (2024). https://doi.org/10.1038/s41390-024-03145-z
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41390-024-03145-z