Abstract
Background
The study of patient-ventilator interactions (PVI) in mechanically ventilated neonates is limited by the lack of unified PVI definitions and tools to perform large scale analyses.
Methods
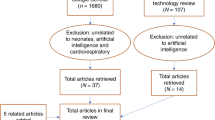
An observational study was conducted in 23 babies randomly selected from 170 neonates who were ventilated with SIPPV-VG, SIMV-VG or PSV-VG mode for at least 12 h. 500 breaths were randomly selected and manually annotated from each recording to train convolutional neural network (CNN) models for PVI classification.
Results
The average asynchrony index (AI) over all recordings was 52.5%. The most frequently occurring PVIs included expiratory work (median: 28.4%, interquartile range: 23.2–40.2%), late cycling (7.6%, 2.8–10.2%), failed triggering (4.6%, 1.2–6.2%) and late triggering (4.4%, 2.8–7.4%). Approximately 25% of breaths with a PVI had two or more PVIs occurring simultaneously. Binary CNN classifiers were developed for PVIs affecting ≥1% of all breaths (n = 7) and they achieved F1 scores of >0.9 on the test set except for early triggering where it was 0.809.
Conclusions
PVIs occur frequently in neonates undergoing conventional mechanical ventilation with a significant proportion of breaths containing multiple PVIs. We have developed computational models for seven different PVIs to facilitate automated detection and further evaluation of their clinical significance in neonates.
Impact
-
The study of patient-ventilator interactions (PVI) in mechanically ventilated neonates is limited by the lack of unified PVI definitions and tools to perform large scale analyses.
-
By adapting a recent taxonomy of PVI definitions in adults, we have manually annotated neonatal ventilator waveforms to determine prevalence and co-occurrence of neonatal PVIs.
-
We have also developed binary deep learning classifiers for common PVIs to facilitate their automatic detection and quantification.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 14 print issues and online access
$259.00 per year
only $18.50 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
Data availability
The computer code of the deep learning models and their analysis can be freely accessed at https://github.com/chongtwd/Detection-and-quantitative-analysis-of-patient-ventilator-interactions-in-ventilated-neonates. The ventilator data used to train and evaluate the models are not publicly available due to ethical concerns but are available from the corresponding author on reasonable request and subject to favorable ethical opinion.
References
Brown, M. K. & DiBlasi, R. M. Mechanical ventilation of the premature neonate. Respir. Care 56, 1298–1311 (2011).
Norman, M., Jonsson, B., Wallström, L. & Sindelar, R. Respiratory support of infants born at 22–24 weeks of gestational age. Semin. Fetal Neonatal Med. 27, 101328 (2022).
Miller, J. D. & Carlo, W. A. Pulmonary complications of mechanical ventilation in neonates. Clin. Perinatol. 35, 273–281 (2008).
Baker, C. D. Chronic respiratory failure in bronchopulmonary dysplasia. Pediatr. Pulmonol. 56, 3490–3498 (2021).
DeMauro, S. B. Neurodevelopmental outcomes of infants with bronchopulmonary dysplasia. Pediatr. Pulmonol. 56, 3509–3517 (2021).
Schmalisch, G. Basic principles of respiratory function monitoring in ventilated newborns: a review. Paediatr. Respir. Rev. 20, 76–82 (2016).
Beck, J. & Sinderby, C. Neurally adjusted ventilatory assist in newborns. Clin. Perinatol. 48, 783–811 (2021).
Hummler, H. & Schulze, A. New and alternative modes of mechanical ventilation in neonates. Semin. Fetal Neonatal Med. 14, 42–48 (2009).
van Kaam, A. H. et al. Modes and strategies for providing conventional mechanical ventilation in neonates. Pediatr. Res. 90, 957–962 (2021).
Mammel, M. C. & Donn, S. M. Real-time pulmonary graphics. Semin. Fetal Neonatal Med. 20, 181–191 (2015).
Crooke, P. S., Head, J. D. & Marini, J. J. A general two-compartment model for mechanical ventilation. Math. Comp. Model. 24, 1–18 (1996).
Bhutani, V. K., Sivieri, E. M., Abbasi, S. & Shaffer, T. H. Evaluation of neonatal pulmonary mechanics and energetics: a two factor least mean square analysis. Pediatr. Pulmonol. 4, 150–158 (1988).
Nilsestuen, J. O. & Hargett, K. D. Using ventilator graphics to identify patient-ventilator asynchrony. Respir. Care 50, 202–234 (2005).
Mirabella, L. et al. Patient-ventilator asynchronies: clinical implications and practical solutions. Respir. Care 65, 1751–1766 (2020).
Blanch, L. et al. Asynchronies during mechanical ventilation are associated with mortality. Intensive Care Med. 41, 633–641 (2015).
Kyo, M. et al. Patient–ventilator asynchrony, impact on clinical outcomes and effectiveness of interventions: a systematic review and meta-analysis. J. Intensive Care 9, 50 (2021).
Mortamet, G. et al. Patient–ventilator asynchrony during conventional mechanical ventilation in children. Ann. Intensive Care 7, 122 (2017).
Blokpoel, R. G. T., Burgerhof, J. G. M., Markhorst, D. G. & Kneyber, M. C. J. Trends in pediatric patient-ventilator asynchrony during invasive mechanical ventilation. Pediatr. Crit. Care Med. 22, 993–997 (2021).
Greenough, A., Morley, C. & Davis, J. Interaction of spontaneous respiration with artificial ventilation in preterm babies. J. Pediatr. 103, 769–773 (1983).
McCallion, N., Lau, R., Dargaville, P. A. & Morley, C. J. Volume guarantee ventilation, interrupted expiration, and expiratory braking. Arch. Dis. Child. 90, 865–870 (2005).
Mally, P. V., Beck, J., Sinderby, C., Caprio, M. & Bailey, S. M. Neural breathing pattern and patient-ventilator interaction during neurally adjusted ventilatory assist and conventional ventilation in newborns. Pediatr. Crit. Care Med. 19, 48–55 (2018).
Bignall, S., Dixon, P., Quinn, C. & Kitney, R. Monitoring interactions between spontaneous respiration and mechanical inflations in preterm neonates. Crit. Care Med. 25, 545–553 (1997).
Adams, J. Y. et al. Development and validation of a multi-algorithm analytic platform to detect off-target mechanical ventilation. Sci. Rep. 7, 14980 (2017).
Blanch, L. et al. Validation of the Better Care® system to detect ineffective efforts during expiration in mechanically ventilated patients: a pilot study. Intensive Care Med. 38, 772–780 (2012).
Rehm, G. et al. Creation of a robust and generalizable machine learning classifier for patient ventilator asynchrony. Methods Inf. Med. 57, 208–219 (2018).
Casagrande, A. et al. An effective pressure–flow characterization of respiratory asynchronies in mechanical ventilation. J. Clin. Monit. Comput. 35, 289–296 (2020).
Gholami, B. et al. Replicating human expertise of mechanical ventilation waveform analysis in detecting patient-ventilator cycling asynchrony using machine learning. Comput. Biol. Med. 97, 137–144 (2018).
Bakkes, T. H. G. F., Montree, R. J. H., Mischi, M., Mojoli, F. & Turco, S. A machine learning method for automatic detection and classification of patient-ventilator asynchrony. In: 42nd Annual International Conference of the IEEE Engineering in Medicine & Biology Society (EMBC). IEEE (2020). Accessed on 7th June, 2022, from https://doi.org/10.1109/embc44109.2020.9175796
Zhang, L. et al. Detection of patient-ventilator asynchrony from mechanical ventilation waveforms using a two-layer long short-term memory neural network. Comp. Biol. Med. 120, 103721 (2020).
Rusconi, F. et al. Reference values for respiratory rate in the first 3 years of life. Pediatrics 94, 350–355 (1994).
Numa, A. H. & Newth, C. J. Anatomic dead space in infants and children. J. Appl. Physiol. 80, 1485–1489 (1996).
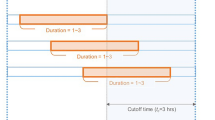
Mireles-Cabodevila, E., Siuba, M. T. & Chatburn, R. L. A taxonomy for patient-ventilator interactions and a method to read ventilator waveforms. Respir. Care 67, 129–148 (2021).
Chong, D., Morley, C. J. & Belteki, G. Computational analysis of neonatal ventilator waveforms and loops. Pediatr. Res. 89, 1432–1441 (2020).
Thille, A. W., Rodriguez, P., Cabello, B., Lellouche, F. & Brochard, L. Patient-ventilator asynchrony during assisted mechanical ventilation. Intensive Care Med. 32, 1515–1522 (2006).
Glorot, X., Bordes, A. & Bengio, Y. Deep sparse rectifier neural networks”, In Int. Conf. Artificial Intelligence and Statistics, 315–323 (2011).
Kingma, D., & Adam, J. B. A Method for Stochastic Optimization. (2014) Retrieved on 3rd August 2022, from https://arxiv.org/abs/1412.6980.
Wikipedia contributors. F-score. In Wikipedia, The Free Encyclopedia. Retrieved on 19th April 2023, from https://en.wikipedia.org/w/index.php?title=F-score&oldid=1148225663
de Waal, C. G., van Leuteren, R. W., de Jongh, F. H., van Kaam, A. H. & Hutten, G. J. Patient-ventilator asynchrony in preterm infants on nasal intermittent positive pressure ventilation. Arch. Dis. Child Fetal Neonatal Ed. 104, F280–F284 (2019).
Acknowledgements
We would like to thank Thomas Krüger, Kreske Brunckhorst and the engineers of Dräger Medical for their advice and the program exporting data from the ventilator. We thank to Lakshana Gunathilagan for performing some of the manual waveform annotation. We thank to Professor Colin Morley and Dr Amanda Ogilvy-Stuart for her advice and comments on the manuscript. G.B. is a consultant to Vyaire Medical (Mettawa, IL, US) and Dräger Medical (Lübeck, Germany).
Funding
This project was indirectly supported by the National Institute of Health and Care Research, UK (NIHR).
Author information
Authors and Affiliations
Contributions
DC contributed to the conceptual design of the study, performed the manual annotation, analyzed the data, developed the classifiers, and contributed to the writing of the manuscript. GB contributed to the conceptual design of the study, helped with interpretation of results, and contributed to the writing of the manuscript. All authors reviewed and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Informed consent
Informed consent was obtained from parents in writing.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Chong, D., Belteki, G. Detection and quantitative analysis of patient-ventilator interactions in ventilated infants by deep learning networks. Pediatr Res (2024). https://doi.org/10.1038/s41390-024-03064-z
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41390-024-03064-z