Abstract
Background
The majority of neonatal NIRS literature recommends target ranges for cerebral saturation (rScO2) based on data using adult sensors. Neonatal sensors are now commonly used in the neonatal intensive care unit (NICU). However, there is limited clinical data correlating these two measurements of cerebral oxygenation.
Methods
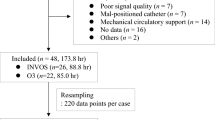
A prospective observational study was conducted in two NICUs between November 2019 and May 2021. An adult sensor was placed on infants undergoing routine cerebral NIRS monitoring with a neonatal sensor. Time-synchronized rScO2 measurements from both sensors, heart rate, and systemic oxygen saturation values were collected over 6 h under varying clinical conditions and compared.
Results
Time-series data from 44 infants demonstrated higher rScO2 measurements with neonatal sensors than with adult sensors; however, the magnitude of the difference varied depending on the absolute value of rScO2 (Adult = 0.63 × Neonatal + 18.2). While there was an approximately 10% difference when adult sensors read 85%, readings were similar when adult sensors read 55%.
Conclusion
rScO2 measured by neonatal sensors is typically higher than measured by adult sensors, but the difference is not fixed and is less at the threshold indicative of cerebral hypoxia. Assuming fixed differences between adult and neonatal sensors may lead to overdiagnosis of cerebral hypoxia.
Impact
-
In comparison to adult sensors, neonatal sensors rScO2 readings are consistently higher, but the magnitude of the difference varies depending on the absolute value of rScO2.
-
Marked variability during high and low rScO2 readings was noted, with approximately 10% difference when adult sensors read 85%, but nearly similar (58.8%) readings when adult sensors read 55%.
-
Estimating fixed differences of approximately 10% between adult and neonatal probes may lead to an inaccurate diagnosis of cerebral hypoxia and result in subsequent unnecessary interventions.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 14 print issues and online access
$259.00 per year
only $18.50 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
Data availability
Datasets generated and analyzed during the current study are available from corresponding author on reasonable request.
References
Van Bel, F., Lemmers, P. M. A. & Naulaers, G. Monitoring neonatal regional cerebral oxygen saturation in clinical practice: value and pitfalls. Neonatology 94, 237–244 (2008).
Alderliesten, T. et al. Brain oxygen saturation assessment in neonates using T2- prepared blood imaging of oxygen saturation and near-infrared spectroscopy. J. Cereb. Blood Flow Metab. 37, 902–913 (2017).
Watzman, H. M. et al. Arterial and venous contributions to near-infrared cerebral oximetry. Anesthesiology 93, 947–953 (2000).
Benni, P. B. et al. Validation of the CAS neonatal NIRS system by monitoring VVECMO patients: preliminary results. Adv. Exp. Med. Biol. 566, 195–201 (2005).
Nagdyman, N. et al. Comparison of different near-infrared spectroscopic cerebral oxygenation indices with central venous and jugular venous oxygenation saturation in children. Paediatr. Anaesth. 18, 160–166 (2008).
Rais-Bahrami, K., Rivera, O. & Short, B. L. Validation of a noninvasive neonatal optical cerebral oximeter in veno-venous ECMO patients with a cephalad catheter. J. Perinatol. 26, 628–635 (2006).
Alderliesten, T. et al. Reference values of regional cerebral oxygen saturation during the first 3 days of life in preterm neonates. Pediatr. Res. 79, 55–64 (2016).
Hyttel-Sorensen, S. et al. Cerebral near-infrared spectroscopy oximetry in extremely preterm infants: phase II randomized clinical trial. BMJ 350, g7635 (2015).
Hansen, M. L. et al. Cerebral near-infrared spectroscopy monitoring versus treatment as usual for extremely preterm infants: a protocol for the SafeBoosC randomized clinical phase III trial. Trials 20, 811 (2019).
Hyttel-Sorensen, S., Kleiser, S., Wolf, M. & Greisen, G. Calibration of a prototype NIRS oximeter against two commercial devices on a blood-lipid phantom. Biomed. Opt. Express 4, 1662–1672 (2013).
Kusaka, T. et al. Quantification of cerebral oxygenation by full-spectrum near-infrared spectroscopy using a two-point method. Comp. Biochem. Physiol. A Mol. Integr. Physiol. 132, 121–132 (2002).
Kleiser, S., Nasseri, N., Andresen, B., Greisen, G. & Wolf, M. Comparison of tissue oximeters on a liquid phantom with adjustable optical properties. Biomed. Opt. Express 7, 2973–2992 (2016).
Dix, L. M. L., van Bel, F., Baerts, W. & Lemmers, P. M. A. Comparing near-infrared spectroscopy devices and their sensors for monitoring regional cerebral oxygen saturation in the neonate. Pediatr. Res. 74, 557–563 (2013).
Van Meurs, K. P. et al. Development of a neuroNICU with a broader focus on all newborns at risk of brain injury: the first 2 years. Am. J. Perinatol. 35, 1196–1205 (2018).
Pellicer, A. et al. The SafeBoosC phase II randomized clinical trial: a treatment guideline for targeted near-infrared-delivered cerebral tissue oxygenation versus standard treatment in extremely preterm infants. Neonatology 104, 171–178 (2013).
Rosner, B., Willet, W. C. & Spiegelman, D. Correction of logistic regression relative risk estimates and confidence intervals for systematic within-person measurement error. Stat. Med. 8, 1051–1069 (1989).
Frost, C. & Thompson, S. G. Correcting for regression dilution bias: comparison of methods for a single predictor variable. J. R. Stat. Soc. A 163, 173–189 (2000).
Buonaccorsi, J. P. In Encyclopedia of Biostatistics (eds Armitage, P. & Colton, T.) 1515–1516 (Chichester, 1998).
Deming, W. E. Statistical Adjustment of Data. Revised Ed. (Dover Publications – Mathematics, 1964).
Hongo, K., Kobayashi, S., Okudera, H., Hokama, M. & Nakagawa, F. Noninvasive cerebral optical spectroscopy: depth-resolved measurements of cerebral haemodynamics using indocyanine green. Neurol. Res. 17, 89–93 (1995).
Cui, W., Wang, N. & Chance, B. Study of photon migration depths with time-resolved spectroscopy. Opt. Lett. 16, 1632–1634 (1991).
Wijbenga, R. G., Lemmers, P. M. & van Bel, F. Cerebral oxygenation during the first days of life in preterm and term neonates: differences between different brain regions. Pediatr. Res. 70, 389–394 (2011).
Chock, V. Y. et al. Cerebral oxygenation and autoregulation in preterm infants (Early NIRS Study). J. Pediatr. 227, 94–100 (2020).
Ancora, G. et al. Early predictors of short term neurodevelopmental outcome in asphyxiated cooled infants. A combined brain amplitude integrated electroencephalography and near infrared spectroscopy study. Brain Dev. 35, 26–31 (2013).
Lemmers, P. M. et al. Cerebral oxygenation and brain activity after perinatal asphyxia: does hypothermia change their prognostic value? Pediatr. Res. 74, 180–185 (2013).
Jain, S. V. et al. Cerebral regional oxygen saturation trends in infants with hypoxic-ischemic encephalopathy. Early Hum. Dev. 113, 55–61 (2017).
Lemmers, P. & van Bel, F. Left-to-right differences of regional cerebral oxygen saturation and oxygen extraction in preterm infants during the first days of life. Pediatr. Res. 65, 226–230 (2009).
Alderliesten, T. et al. Hypotension in preterm neonates: low blood pressure alone does not affect neurodevelopmental outcome. J. Pediatr. 164, 986–991 (2014).
Jani, P. et al. Liberal hemoglobin threshold affects cerebral arterial pulsed Doppler and cardiac output, not cerebral tissue oxygenation: a prospective cohort study in anemic preterm infants. Transfusion 59, 3093–3101 (2019).
Pocivalnik, M. et al. Regional tissue oxygen saturation: comparability and reproducibility of different devices. J. Biomed. Opt. 16, 057004 (2011).
Schneider, A. et al. Comparison of four near-infrared spectroscopy devices shows that they are only suitable for monitoring cerebral oxygenation trends in preterm infants. Acta Paediatr. 103, 934–938 (2014).
Andresen, B., Greisen, G. & Hyttel-Sorensen, S. Comparison of INVOS 5100C and Nonin SenSmart X-100 oximeter performance in preterm infants with spontaneous apnea. Pediatr. Res. 87, 1244–1250 (2020).
Dani, C., Pratesi, S., Fontanelli, G., Barp, J. & Bertini, G. Blood transfusions increase cerebral, splanchnic, and renal oxygenation in anemic preterm infants. Transfusion 50, 1220–1226 (2010).
van Hoften, J. C., Verhagen, E. A., Keating, P., Ter Horst, H. J. & Bos, A. F. Cerebral tissue oxygen saturation and extraction in preterm infants before and after blood transfusion. Arch. Dis. Child. Fetal Neonatal Ed. 95, F352–F358 (2010).
Funding
The study did not receive financial assistance.
Author information
Authors and Affiliations
Contributions
G.F.T.V. made substantial contributions to the study conception and design, interpretation of data, drafting the article and revising it critically for intellectual content, and final approval of version to be approved. A.D. and J.Z. made substantial contributions to the study conception and design, interpretation of data, drafting the article, and final approval of version to be approved. C.Y.N. made substantial contributions to the study conception and design, acquisition of data, interpretation of data, drafting the article and revising it critically for intellectual content, and final approval of version to be approved. E.S.Y., J.K., and M.G. made substantial contributions to the acquisition of data. K.P.V.M. and V.Y.C. made substantial contributions to the study conception and design, analysis and interpretation of data, drafting the article and revising it critically for intellectual content, and final approval of version to be approved.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
The free and informed consent form was required and signed by the legal guardians of the patients.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Variane, G.F.T., Dahlen, A., Noh, C.Y. et al. Cerebral oxygen saturation in neonates: a bedside comparison between neonatal and adult NIRS sensors. Pediatr Res 94, 1810–1816 (2023). https://doi.org/10.1038/s41390-023-02705-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41390-023-02705-z