Abstract
Background and aims
Perinatal arterial ischemic stroke (PAIS) often has lifelong neurodevelopmental consequences. We aimed to review early predictors (<4 months of age) of long-term outcome.
Methods
We carried out a systematic literature search (PubMed and Embase), and included articles describing term-born infants with PAIS that underwent a diagnostic procedure within four months of age, and had any reported outcome parameter ≥12 months of age. Two independent reviewers included studies and performed risk of bias analysis.
Results
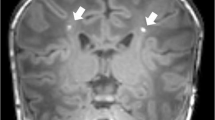
We included 41 articles reporting on 1395 infants, whereof 1255 (90%) infants underwent follow-up at a median of 4 years. A meta-analysis was performed for the development of cerebral palsy (n = 23 studies); the best predictor was the qualitative or quantitative assessment of the corticospinal tracts on MRI, followed by standardized motor assessments. For long-term cognitive functioning, bedside techniques including (a)EEG and NIRS might be valuable. Injury to the optic radiation on DTI correctly predicted visual field defects. No predictors could be identified for behavior, language, and post-neonatal epilepsy.
Conclusion
Corticospinal tract assessment on MRI and standardized motor assessments are best to predict cerebral palsy after PAIS. Future research should be focused on improving outcome prediction for non-motor outcomes.
Impact
-
We present a systematic review of early predictors for various long-term outcome categories after perinatal arterial ischemic stroke (PAIS), including a meta-analysis for the outcome unilateral spastic cerebral palsy.
-
Corticospinal tract assessment on MRI and standardized motor assessments are best to predict cerebral palsy after PAIS, while bedside techniques such as (a)EEG and NIRS might improve cognitive outcome prediction.
-
Future research should be focused on improving outcome prediction for non-motor outcomes.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 14 print issues and online access
$259.00 per year
only $18.50 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
Data availability
Template data collection forms can be found in the protocol on Prospero. Data extracted from included studies and data used for analysis can be made available upon request with the corresponding author.
References
Sorg, A. L. et al. Incidence estimates of perinatal arterial ischemic stroke in preterm- and term-born infants: a national capture-recapture calculation corrected surveillance study. Neonatology 118, 727–733 (2021).
Gale, C. et al. Neonatal brain injuries in England: Population-based incidence derived from routinely recorded clinical data held in the National Neonatal Research Database. Arch. Dis. Child. Fetal Neonatal Ed. 103, F301–F306 (2018).
Ferriero, D. M. et al. Management of stroke in neonates and children: A scientific statement from the American Heart Association/American stroke association. Stroke 50, E51–E96 (2019).
Wagenaar, N. et al. Neurodevelopment after perinatal arterial ischemic stroke. Pediatrics 142, e20174164 (2018).
Benders, M. J. et al. Feasibility and safety of erythropoietin for neuroprotection after perinatal arterial ischemic stroke. J. Pediatr. 164, 481–482 (2014).
Baak, L. M. et al. Feasibility and safety of intranasally administered mesenchymal stromal cells after perinatal arterial ischaemic stroke in the Netherlands (PASSIoN): a first-in-human, open-label intervention study. Lancet Neurol. 21, 528–536 (2022).
Wagenaar, N. et al. Promoting neuroregeneration after perinatal arterial ischemic stroke: neurotrophic factors and mesenchymal stem Brain Activity and Cerebral Oxygenation After Perinatal Arterial Ischemic Stroke Are Associated With Neurodevelopment. Pediatr. Res. 83, 372–384 (2018).
Hoare, B. J. et al. Constraint-induced movement therapy in children with unilateral cerebral palsy. Cochrane Database Syst. Rev. 2019, CD004149 (2019).
Charles, J. & Gordon, A. M. Development of hand-arm bimanual intensive training (HABIT) for improving bimanual coordination in children with hemiplegic cerebral palsy. Dev. Med. Child Neurol. 48, 931–936 (2006).
Kirton, A. et al. Brain stimulation and constraint for perinatal stroke hemiparesis: The PLASTIC CHAMPS Trial. Neurology 86, 1659–1667 (2016).
Kirton, A. et al. Transcranial direct current stimulation for children with perinatal stroke and hemiparesis. Neurology 88, 259–267 (2017).
Ouzzani, M., Hammady, H., Fedorowicz, Z. & Elmagarmid, A. Rayyan-a web and mobile app for systematic reviews. Syst. Rev. 5, 1–10 (2016).
Moola, S. et al. Chapter 7: Systematic reviews of etiology and risk. in Joanna Briggs Institute Reviewer’s Manual. (eds. Aromataris, E. & Munn, Z.) (The Joanna Briggs Institute, 2017).
Guo, J. & Riebler, A. Meta4diag: Bayesian bivariate meta-analysis of diagnostic test studies for routine practice. J. Stat. Softw. 83, 1–27 (2018).
Hamza, T. H., Reitsma, J. B. & Stijnen, T. Meta-analysis of diagnostic studies: A comparison of random intercept, normal-normal, and binomial-normal bivariate summary ROC approaches. Med. Decis. Mak. 28, 639–649 (2008).
Wagenaar, N. et al. Brain activity and cerebral oxygenation after perinatal arterial ischemic stroke are associated with neurodevelopment. Stroke 50, 2668–2676 (2019).
McBride, M. C., Laroia, N. & Guillet, R. Electrographic seizures in neonates correlate with poor neurodevelopmental outcome. Neurology 55, 506–513 (2000).
Tekgul, H. et al. The current etiologic profile and neurodevelopmental outcome of seizures in term newborn infants. Pediatrics 117, 1270–1280 (2006).
Schulzke, S., Weber, P., Luetschg, J. & Fahnenstich, H. Incidence and diagnosis of unilateral arterial cerebral infarction in newborn infants. J. Perinat. Med. 33, 170–175 (2005).
Lee, H. J. et al. Clinical presentations and neurodevelopmental outcomes of perinatal stroke in preterm and term neonates: a case series. J. Korean Med. Sci. 25, 888–894 (2010).
Yi, Y. Y. et al. Clinical outcomes of cerebral infarctions in neonates. Pediatr. Neurol. 45, 368–372 (2011).
Suppiej, A. et al. Pediatric epilepsy following neonatal seizures symptomatic of stroke. Brain Dev. 38, 27–31 (2016).
Nevalainen, P. et al. Bedside neurophysiological tests can identify neonates with stroke leading to cerebral palsy. Clin. Neurophysiol. 130, 759–766 (2019).
Wanigasinghe, J. et al. Epilepsy in hemiplegic cerebral palsy due to perinatal arterial ischaemic stroke. Dev. Med. Child Neurol. 52, 1021–1027 (2010).
Mercuri, E. et al. Early prognostic indicators of outcome in infants with neonatal cerebral infarction: a clinical, electroencephalogram, and magnetic resonance imaging study. Pediatrics 103, 39–46 (1999).
Guzzetta, A. et al. General movements detect early signs of hemiplegia in term infants with neonatal cerebral infarction. Neuropediatrics 34, 61–66 (2003).
Guzzetta, A. et al. Hand movements at 3 months predict later hemiplegia in term infants with neonatal cerebral infarction. Dev. Med. Child Neurol. 52, 767–772 (2010).
Pascal, A. et al. Motor outcome after perinatal stroke and early prediction of unilateral spastic cerebral palsy. Eur. J. Paediatr. Neurol. 29, 54–61 (2020).
Yin, H. et al. A pilot study of the General Movement Optimality Score detects early signs of motor disorder in neonates with arterial ischemic stroke. Early Hum. Dev. 163, 105484 (2021).
Eyre, J. A. et al. Is hemiplegic cerebral palsy equivalent to amblyopia of the corticospinal system? Ann. Neurol. 62, 493–503 (2007).
Ecury-Goossen, G. M. et al. Neurodevelopmental outcome after neonatal perforator stroke. Dev. Med. Child Neurol. 58, 49–56 (2016).
Hajek, C. A. et al. Cognitive outcomes following arterial ischemic stroke in infants and children. J. Child Neurol. 29, 887–894 (2014).
van Buuren, L. M. et al. Cognitive outcome in childhood after unilateral perinatal brain injury. Dev. Med. Child Neurol. 55, 934–940 (2013).
Roze, E. et al. Tractography of the corticospinal tracts in infants with focal perinatal injury: comparison with normal controls and to motor development. Neuroradiology 54, 507–516 (2012).
Westmacott, R., Macgregor, D., Askalan, R. & Deveber, G. Late emergence of cognitive deficits after unilateral neonatal stroke. Stroke 40, 2012–2019 (2009).
Kirton, A., Shroff, M., Visvanathan, T. & deVeber, G. Quantified corticospinal tract diffusion restriction predicts neonatal stroke outcome. Stroke 38, 974–980 (2007).
De Vries, L. S., Van Der Grond, J., Van Haastert, I. C. & Groenendaal, F. Prediction of outcome in new-born infants with arterial ischaemic stroke using diffusion-weighted magnetic resonance imaging. Neuropediatrics 36, 12–20 (2005).
Boardman, J. P. et al. Magnetic resonance image correlates of hemiparesis after neonatal and childhood middle cerebral artery stroke. Pediatrics 115, 321–326 (2005).
Mercuri, E. et al. Neonatal cerebral infarction and neuromotor outcome at school age. Pediatrics 113, 95–100 (2004).
Mercuri, E. et al. Neonatal cerebral infarction and visual function at school age. Arch. Dis. Child. Fetal Neonatal Ed. 88, F487–F491 (2003).
Núñez, C. et al. Neonatal arterial stroke location is associated with outcome at 2 years: A voxel-based lesion-symptom mapping study. Arch. Dis. Child. Fetal Neonatal Ed. 107, F45–F50 (2022).
Wiedemann, A. et al. Impact of stroke volume on motor outcome in neonatal arterial ischemic stroke. Eur. J. Paediatr. Neurol. 25, 97–105 (2020).
Giudice, C., Rogers, E. E., Johnson, B. C., Glass, H. C. & Shapiro, K. A. Neuroanatomical correlates of sensory deficits in children with neonatal arterial ischemic stroke. Dev. Med. Child Neurol. 61, 667–671 (2019).
Koenraads, Y. et al. Prediction of visual field defects in newborn infants with perinatal arterial ischemic stroke using early MRI and DTI-based tractography of the optic radiation. Eur. J. Paediatr. Neurol. 20, 309–318 (2016).
van der Aa, N. E. et al. Neonatal posterior cerebral artery stroke: clinical presentation, MRI findings, and outcome. Dev. Med. Child Neurol. 55, 283–290 (2013).
Husson, B. et al. Motor outcomes after neonatal arterial ischemic stroke related to early MRI data in a prospective study. Pediatrics 126, 912–918 (2010).
Ricci, D. et al. Cognitive outcome at early school age in term-born children with perinatally acquired middle cerebral artery territory infarction. Stroke 39, 403–410 (2008).
Golomb, M. R., Garg, B. P., Saha, C., Azzouz, F. & Williams, L. S. Cerebral palsy after perinatal arterial ischemic stroke. J. Child Neurol. 23, 279–286 (2008).
Mackay, M. T. et al. Pediatric ASPECTS predicts outcomes following acute symptomatic neonatal arterial stroke. Neurology 94, e1259–e1270 (2020).
Wusthoff, C. J. et al. Risk of later seizure after perinatal arterial ischemic stroke: a prospective cohort study. Pediatrics 127, e1550–e1557 (2011).
Srivastava, R. et al. Diffusion imaging of cerebral diaschisis in neonatal arterial ischemic stroke. Pediatr. Neurol. 100, 49–54 (2019).
van der Aa, N. E. et al. Neonatal neuroimaging predicts recruitment of contralesional corticospinal tracts following perinatal brain injury. Dev. Med. Child Neurol. 55, 707–712 (2013).
Van Der Aa, N. E. et al. Does diffusion tensor imaging-based tractography at 3 months of age contribute to the prediction of motor outcome after perinatal arterial ischemic stroke? Stroke 42, 3410–3414 (2011).
van der Aa, N. E. et al. Quantification of white matter injury following neonatal stroke with serial DTI. Pediatr. Res. 73, 756–762 (2013).
Husson, B. et al. MR angiography findings in infants with neonatal arterial ischemic stroke in the middle cerebral artery territory: A prospective study using circle of Willis MR angiography. Eur. J. Radiol. 85, 1329–1335 (2016).
Ryll, U. C. et al. Predictive validity of the Hand Assessment for Infants in infants at risk of unilateral cerebral palsy. Dev. Med. Child Neurol. 63, 436–443 (2020).
Einspieler, C. et al. Cerebral palsy: Early markers of clinical phenotype and functional outcome. J. Clin. Med. 8, 1616 (2019).
Novak, I. et al. Early, accurate diagnosis and early intervention in cerebral palsy: Advances in diagnosis and treatment. JAMA Pediatr. 171, 897–907 (2017).
Haataja, L. et al. Optimality score for the neurologic examination of the infant at 12 and 18 months of age. J. Pediatr. 135, 153–161 (1999).
Tong, S., Baghurst, P., Vimpani, G. & McMichael, A. Socioeconomic Position, Maternal IQ, Home Environment, and Cognitive Development. J. Pediatr. 151, 284–288 (2007).
Mollon, J. et al. Genetic influence on cognitive development between childhood and adulthood. Mol. Psychiatry 26, 656–665 (2021).
Lo, W. et al. Social competence following neonatal and childhood stroke. Int. J. Stroke 9, 1037–1044 (2014).
Gold, J. J. & Trauner, D. A. Hippocampal volume and memory performance in children with perinatal stroke. Pediatr. Neurol. 50, 18–25 (2014).
Oskoui, M. & Shevell, M. I. Profile of pediatric hemiparesis. J. Child Neurol. 20, 471–476 (2005).
Carlsson, M., Hagberg, G. & Olsson, I. Clinical and aetiological aspects of epilepsy in children with cerebral palsy. Dev. Med. Child Neurol. 45, 371–376 (2003).
Morgan, C. et al. The pooled diagnostic accuracy of neuroimaging, general movements, and neurological examination for diagnosing cerebral palsy early in high-risk infants: A case control study. J. Clin. Med. 8, 1879 (2019).
Cérébrale, F. P. ENSEMBLE—European Newborn Study: Early Markers for a Better LifE. https://fondationparalysiecerebrale.org/en/ensemble-project.
Makropoulos, A., Robinson, E. C., Schuh, A. & Wright, R. The Developing Human Connectome Project: a minimal processing pipeline for neonatal cortical surface reconstruction. Neuroimage 173, 88–112 (2019).
Dick, A. S., Raja Beharelle, A., Solodkin, A. & Small, S. L. Interhemispheric functional connectivity following prenatal or perinatal brain injury predicts receptive language outcome. J. Neurosci. 33, 5612–5625 (2013).
Craig, B. T. et al. Crossed cerebellar atrophy in perinatal stroke. Stroke 50, 175–177 (2019).
Hellstrom-Westas, L., Resen, I. & Svenningsen, N. W. Predictive value of early continuous amplitude integrated EEG recordings on outcome after severe birth asphyxia in full term infants. Arch. Dis. Child 72, 34–38 (1995).
Einspieler, C. & Prechtl, H. F. R. Prechtl’s assessment of general movements: A diagnostic tool for the functional assessment of the young nervous system. Ment. Retard. Dev. Disabil. Res. Rev. 11, 61–67 (2005).
Govaert, P. Sonographic stroke templates. Semin. Fetal Neonatal. Med. 14, 284–298 (2009).
Kirton, A., Deveber, G., Pontigon, A.-M., Macgregor, D. & Shroff, M. Presumed perinatal ischemic stroke: vascular classification predicts outcomes. Ann. Neurol. 63, 436–443 (2008).
de Vries, L. S. et al. Infarcts in the vascular distribution of the middle cerebral artery in preterm and fullterm infants. Neuropediatrics 28, 88–96 (1997).
Funding
This work was supported by the European Society for Pediatric Research (ESPR). The funder had no role in the study design, data collection and analysis, preparation of the manuscript or decision to publish. The authors have no further conflicts of interest to declare.
Author information
Authors and Affiliations
Contributions
L.M.B. designed the protocol, performed the article search, and the statistical analyses, and wrote the original draft. L.M.B. and A.A.E.V. selected articles, extracted data and performed risk of bias analysis, with NEA as a third reviewer in case of discrepancies. NEA, F.G., J.D., C.H.A.N., M.J.N.L.B., and N.W. aided in design, conceptualization, and supervision. All authors reviewed and edited the paper and confirm that they had full access to all the data in the study and accept responsibility to submit for publication.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Baak, L.M., van der Aa, N.E., Verhagen, A.A.E. et al. Early predictors of neurodevelopment after perinatal arterial ischemic stroke: a systematic review and meta-analysis. Pediatr Res 94, 20–33 (2023). https://doi.org/10.1038/s41390-022-02433-w
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41390-022-02433-w