Abstract
Background
Growing evidence suggests that cardiovascular disease develops over the lifetime, often beginning in childhood. Metal exposures have been associated with cardiovascular disease and important risk factors, including dyslipidemia, but prior studies have largely focused on adult populations and single metal exposures.
Objective
To investigate the individual and joint impacts of multiple metal exposures on lipid levels during childhood.
Methods
This cross-sectional study included 291 4-year-old children from the Rhea Cohort Study in Heraklion, Greece. Seven metals (manganese, cobalt, selenium, molybdenum, cadmium, mercury, and lead) were measured in whole blood using inductively coupled plasma mass spectrometry. Serum lipid levels included total cholesterol, triglycerides, high-density lipoprotein (HDL) cholesterol, and low-density lipoprotein (LDL) cholesterol. To determine the joint and individual impacts of child metal exposures (log2-transformed) on lipid levels, Bayesian kernel machine regression (BKMR) was employed as the primary multi-pollutant approach. Potential effect modification by child sex and childhood environmental tobacco smoke exposure was also evaluated.
Results
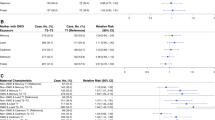
BKMR identified a positive association between the metal mixture and both total and LDL cholesterol. Of the seven metals examined, selenium (median 90.6 [IQR = 83.6, 96.5] µg/L) was assigned the highest posterior inclusion probability for both total and LDL cholesterol. A difference in LDL cholesterol of 8.22 mg/dL (95% CI = 1.85, 14.59) was observed when blood selenium was set to its 75th versus 25th percentile, holding all other metals at their median values. In stratified analyses, the positive association between selenium and LDL cholesterol was only observed among boys or among children exposed to environmental tobacco smoke during childhood.
Impact statement
Growing evidence indicates that cardiovascular events in adulthood are the consequence of the lifelong atherosclerotic process that begins in childhood. Therefore, public health interventions targeting childhood cardiovascular risk factors may have a particularly profound impact on reducing the burden of cardiovascular disease. Although growing evidence supports that both essential and nonessential metals contribute to cardiovascular disease and risk factors, such as dyslipidemia, prior studies have mainly focused on single metal exposures in adult populations. To address this research gap, the current study investigated the joint impacts of multiple metal exposures on lipid concentrations in early childhood.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 6 print issues and online access
$259.00 per year
only $43.17 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
Data availability
The datasets generated and analyzed during the current study are not publicly available due to the privacy of individuals that participated in the study. The data will be available on reasonable request to the Rhea Cohort Study.
References
Cardiovascular diseases (CVDs). https://www.who.int/news-room/fact-sheets/detail/cardiovascular-diseases-(cvds). Accessed 26 Apr 2022.
Mathers CD, Loncar D. Projections of global mortality and burden of disease from 2002 to 2030. PLoS Med. 2006;3:e442.
Yusuf S, Reddy S, Ôunpuu S, Anand S. Global burden of cardiovascular diseases. Circulation. 2001;104:2746–53.
Olson M, Chambers M, Shaibi G. Pediatric markers of adult cardiovascular disease. Curr Pediatr Rev. 2017;13:255–9.
Koskinen J, Juonala M, Dwyer T, Venn A, Thomson R, Bazzano L, et al. Impact of lipid measurements in youth in addition to conventional clinic-based risk factors on predicting preclinical atherosclerosis in adulthood: International Childhood Cardiovascular Cohort Consortium. Circulation. 2018;137:1246–55.
Pool LR, Aguayo L, Brzezinski M, Perak AM, Davis MM, Greenland P, et al. Childhood risk factors and adulthood cardiovascular disease: a systematic review. J Pediatr. 2021;232:118–26.e23.
Expert Panel on Integrated Guidelines for Cardiovascular Health and Risk Reduction in Children and Adolescents; National Heart, Lung, and Blood Institute. Expert panel on integrated guidelines for cardiovascular health and risk reduction in children and adolescents: summary report. Pediatrics 2011;128:S213–56.
Aljahdali AA, Peterson KE, Cantoral A, Ruiz-Narvaez E, Tellez-Rojo MM, Kim HM, et al. Diet Quality scores and cardiometabolic risk factors in mexican children and adolescents: a longitudinal analysis. Nutrients. 2022;14:896.
Pan A, Lin X, Hemler E, Hu FB. Diet and cardiovascular disease: advances and challenges in population-based studies. Cell Metab. 2018;27:489–96.
Nocon M, Hiemann T, Müller-Riemenschneider F, Thalau F, Roll S, Willich SN. Association of physical activity with all-cause and cardiovascular mortality: a systematic review and meta-analysis. Eur J Cardiovasc Prev Rehabil. 2008;15:239–46.
Lear SA, Hu W, Rangarajan S, Gasevic D, Leong D, Iqbal R, et al. The effect of physical activity on mortality and cardiovascular disease in 130 000 people from 17 high-income, middle-income, and low-income countries: the PURE study. Lancet. 2017;390:2643–54.
Münzel T, Hahad O, Sørensen M, Lelieveld J, Duerr GD, Nieuwenhuijsen M, et al. Environmental risk factors and cardiovascular diseases: a comprehensive expert review. Cardiovasc Res. 2022;118:2880–902.
Chowdhury R, Ramond A, O’Keeffe LM, Shahzad S, Kunutsor SK, Muka T, et al. Environmental toxic metal contaminants and risk of cardiovascular disease: systematic review and meta-analysis. BMJ. 2018;362:k3310.
Yang A-M, Lo K, Zheng T-Z, Yang J-L, Bai Y-N, Feng Y-Q, et al. Environmental heavy metals and cardiovascular diseases: status and future direction. Chronic Dis Transl Med. 2020;6:251–9.
Nigra AE, Ruiz-Hernandez A, Redon J, Navas-Acien A, Tellez-Plaza M. Environmental metals and cardiovascular disease in adults: a systematic review beyond lead and cadmium. Curr Environ Health Rep. 2016;3:416–33.
Lamas GA, Bhatnagar A, Jones MR, Mann KK, Nasir K, Tellez-Plaza M, et al. Contaminant metals as cardiovascular risk factors: a scientific statement from the American Heart Association. J Am Heart Assoc. 2023;12:e029852.
Jiang Y, Zheng W. Cardiovascular toxicities upon manganese exposure. Cardiovasc Toxicol. 2005;5:345–54.
O’Neal SL, Zheng W. Manganese toxicity upon overexposure: a decade in review. Curr Environ Health Rep. 2015;2:315–28.
Xiao Y, Yuan Y, Liu Y, Yu Y, Jia N, Zhou L, et al. Circulating multiple metals and incident stroke in Chinese adults. Stroke. 2019;50:1661–8.
Jenkinson MRJ, Meek RMD, Tate R, MacMillan S, Grant MH, Currie S. Cobalt-induced cardiomyopathy—do circulating cobalt levels matter? Bone Jt Res. 2021;10:340–7.
Laclaustra M, Navas-Acien A, Stranges S, Ordovas JM, Guallar E. Serum selenium concentrations and hypertension in the US population. Circ Cardiovasc Qual Outcomes. 2009;2:369–76.
Su L, Jin Y, Unverzagt FW, Liang C, Cheng Y, Hake AM, et al. Longitudinal association between selenium levels and hypertension in a rural elderly Chinese cohort. J Nutr Health Aging. 2016;20:983–8.
Tellez-Plaza M, Guallar E, Navas-Acien A. Environmental metals and cardiovascular disease. BMJ. 2018;362:k3435.
Sanders AP, Flood K, Chiang S, Herring AH, Wolf L, Fry RC. Towards prenatal biomonitoring in north carolina: assessing arsenic, cadmium, mercury, and lead levels in pregnant women. PLoS One. 2012;7:e31354.
Tchounwou PB, Yedjou CG, Patlolla AK, Sutton DJ. Heavy metals toxicity and the environment. EXS. 2012;101:133–64.
Gouaref I, Koceir E-A, Gouaref I, Koceir E-A. Trace elements modulates oxidative stress in type 2 diabetes. 2017 IntechOpen, https://doi.org/10.5772/intechopen.71172.
Balali-Mood M, Naseri K, Tahergorabi Z, Khazdair MR, Sadeghi M. Toxic mechanisms of five heavy metals: mercury, lead, chromium, cadmium, and arsenic. Front Pharmacol. 2021;12. https://www.frontiersin.org/articles/10.3389/fphar.2021.643972. Accessed 26 Nov 2022.
Kang P, Shin HY, Kim KY. Association between dyslipidemia and mercury exposure in adults. Int J Environ Res Public Health. 2021;18:775.
Kim D-W, Ock J, Moon K-W, Park C-H. Association between heavy metal exposure and dyslipidemia among Korean adults: from the Korean National Environmental Health Survey, 2015-2017. Int J Environ Res Public Health. 2022;19:3181.
Zhou Z, Lu Y-H, Pi H-F, Gao P, Li M, Zhang L, et al. Cadmium exposure is associated with the prevalence of dyslipidemia. Cell Physiol Biochem. 2016;40:633–43.
Zhu X, Fan Y, Sheng J, Gu L, Tao Q, Huang R, et al. Association Between blood heavy metal concentrations and dyslipidemia in the elderly. Biol Trace Elem Res. 2021;199:1280–90.
Luo T, Chen S, Cai J, Liu Q, Gou R, Mo X, et al. Association between combined exposure to plasma heavy metals and dyslipidemia in a Chinese population. Lipids Health Dis. 2022;21:131.
Jiang Q, Xiao Y, Long P, Li W, Yu Y, Liu Y, et al. Associations of plasma metal concentrations with incident dyslipidemia: prospective findings from the Dongfeng-Tongji cohort. Chemosphere. 2021;285:131497.
Zhao M, Yin G, Xu J, Ge X, Li A, Mei Y, et al. Independent, combine and interactive effects of heavy metal exposure on dyslipidemia biomarkers: a cross-sectional study in northeastern China. Ecotoxicol Environ Saf. 2023;250:114494.
Huang J-H, Tao L, Wu Y, He W, Wang J-X, Chen X, et al. Cobalt exposure and dyslipidemia in elderly population: the mediating role of systemic inflammation and lipid peroxidation. Environ Sci Pollut Res Int. 2023;30:50402–11.
Xu H, Mao Y, Xu B, Hu Y. Low-level environmental lead and cadmium exposures and dyslipidemia in adults: findings from the NHANES 2005-2016. J Trace Elem Med Biol. 2021;63:126651.
Li S, Liu R, Wu Y, Liang R, Zhou Z, Chen J, et al. Elevated serum lead and cadmium levels associated with increased risk of dyslipidemia in children aged 6 to 9 years in Shenzhen, China. Environ Sci Pollut Res Int. 2023. https://doi.org/10.1007/s11356-023-27335-0
Xiao L, Zhou Y, Ma J, Cao L, Wang B, Zhu C, et al. The cross-sectional and longitudinal associations of chromium with dyslipidemia: a prospective cohort study of urban adults in China. Chemosphere. 2019;215:362–9.
Lopes-Araújo A, Arrifano GP, Macchi BM, Augusto-Oliveira M, Santos-Sacramento L, Rodríguez Martín-Doimeadios RC, et al. Hair mercury is associated with dyslipidemia and cardiovascular risk: an anthropometric, biochemical and genetic cross-sectional study of Amazonian vulnerable populations. Environ Res. 2023;229:115971.
Stranges S, Galletti F, Farinaro E, D’Elia L, Russo O, Iacone R, et al. Associations of selenium status with cardiometabolic risk factors: an 8-year follow-up analysis of the Olivetti Heart study. Atherosclerosis. 2011;217:274–8.
Chen C, Jin Y, Unverzagt FW, Cheng Y, Hake AM, Liang C, et al. The association between selenium and lipid levels: a longitudinal study in rural elderly Chinese. Arch Gerontol Geriatr. 2015;60:147–52.
Cold F, Winther KH, Pastor-Barriuso R, Rayman MP, Guallar E, Nybo M, et al. Randomised controlled trial of the effect of long-term selenium supplementation on plasma cholesterol in an elderly Danish population. Br J Nutr. 2015;114:1807–18.
Ju W, Li X, Li Z, Wu GR, Fu XF, Yang XM, et al. The effect of selenium supplementation on coronary heart disease: a systematic review and meta-analysis of randomized controlled trials. J Trace Elem Med Biol. 2017;44:8–16.
Howe CG, Margetaki K, Vafeiadi M, Roumeliotaki T, Karachaliou M, Kogevinas M, et al. Prenatal metal mixtures and child blood pressure in the Rhea mother-child cohort in Greece. Environ Health. 2021;20:1.
Shih Y-H, Howe CG, Scannell Bryan M, Shahriar M, Kibriya MG, Jasmine F, et al. Exposure to metal mixtures in relation to blood pressure among children 5–7 years old. Environ Epidemiol. 2021;5:e135.
Liu M, Li M, Guo W, Zhao L, Yang H, Yu J, et al. Co-exposure to priority-controlled metals mixture and blood pressure in Chinese children from two panel studies. Environ Pollut. 2022;306:119388.
Ma Y, Liang C, Wang Z, Wang X, Xie L, Tao S, et al. Association between prenatal metals exposure and blood pressure in 5-6 years children: a birth cohort study. Environ Res. 2023;219:114974.
Desai G, Niu Z, Luo W, Frndak S, Shaver AL, Kordas K. Low-level exposure to lead, mercury, arsenic, and cadmium, and blood pressure among 8-17-year-old participants of the 2009–2016 National Health and Nutrition Examination Survey. Environ Res. 2021;197:111086.
Kupsco A, Kioumourtzoglou M-A, Just AC, Amarasiriwardena C, Estrada-Gutierrez G, Cantoral A, et al. prenatal metal concentrations and childhood cardiometabolic risk using Bayesian kernel machine regression to assess mixture and interaction effects. Epidemiology. 2019;30:263–73.
Grigg J. Environmental toxins; their impact on children’s health. Arch Dis Child. 2004;89:244–50.
Michas G, Karvelas G, Trikas A. Cardiovascular disease in Greece; the latest evidence on risk factors. Hell J Cardiol. 2019;60:271–5.
Touloumi G, Karakosta A, Kalpourtzi N, Gavana M, Vantarakis A, Kantzanou M, et al. High prevalence of cardiovascular risk factors in adults living in Greece: the EMENO National Health Examination Survey. BMC Public Health. 2020;20:1665.
Chatzi L, Leventakou V, Vafeiadi M, Koutra K, Roumeliotaki T, Chalkiadaki G, et al. Cohort profile: the mother-child cohort in Crete, Greece (Rhea study). Int J Epidemiol. 2017;46:1392–1393k.
Vafeiadi M, Myridakis A, Roumeliotaki T, Margetaki K, Chalkiadaki G, Dermitzaki E, et al. Association of early life exposure to phthalates with obesity and cardiometabolic traits in childhood: sex specific associations. Front Public Health. 2018;6:327.
Daraki V, Georgiou V, Papavasiliou S, Chalkiadaki G, Karahaliou M, Koinaki S, et al. Metabolic profile in early pregnancy is associated with offspring adiposity at 4 years of age: the Rhea pregnancy cohort Crete, Greece. PLoS One. 2015;10:e0126327.
Chatzi L, Ierodiakonou D, Margetaki K, Vafeiadi M, Chalkiadaki G, Roumeliotaki T, et al. Associations of prenatal exposure to cadmium with child growth, obesity, and cardiometabolic traits. Am J Epidemiol. 2019;188:141–50.
Kippler M, Goessler W, Nermell B, Ekström EC, Lönnerdal B, El Arifeen S, et al. Factors influencing intestinal cadmium uptake in pregnant Bangladeshi women–a prospective cohort study. Environ Res. 2009;109:914–21.
Martinez-Morata I, Sobel M, Tellez-Plaza M, Navas-Acien A, Howe CG, Sanchez TR. A state-of-the-science review on metal biomarkers. Curr Environ Health Rep. 2023. https://doi.org/10.1007/s40572-023-00402-x.
Leventakou V, Georgiou V, Chatzi L, Sarri K. Relative validity of an FFQ for pre-school children in the mother-child ‘Rhea’ birth cohort in Crete, Greece. Public Health Nutr. 2015;18:421–7.
Bobb JF, Claus Henn B, Valeri L, Coull BA. Statistical software for analyzing the health effects of multiple concurrent exposures via Bayesian kernel machine regression. Environ Health. 2018;17:67.
Keil AP, Buckley JP, O’Brien KM, Ferguson KK, Zhao S, White AJ. A quantile-based g-computation approach to addressing the effects of exposure mixtures. Environ Health Perspect. 2020;128:047004.
National Institutes of Health Office of Dietary Supplements. Selenium fact sheet for health professionals. https://ods.od.nih.gov/factsheets/Selenium-HealthProfessional/. Accessed 12 Jun 2023.
National Institutes of Health Office of Dietary Supplements. Manganese fact sheet for health professionals. https://ods.od.nih.gov/factsheets/Manganese-HealthProfessional/. Accessed 21 Feb 2024.
National Institutes of Health Office of Dietary Supplements. Molybdenum fact sheet for health professionals. https://ods.od.nih.gov/factsheets/Molybdenum-HealthProfessional/. Accessed 21 Feb 2024.
Schwalfenberg GK, Genuis SJ. Vitamin D, essential minerals, and toxic elements: exploring interactions between nutrients and toxicants in clinical medicine. ScientificWorldJournal. 2015;2015:318595.
Peng X, Li C, Zhao D, Huang L. Associations of micronutrients exposure with cadmium body burden among population: a systematic review. Ecotoxicol Environ Saf. 2023;256:114878.
Flora G, Gupta D, Tiwari A. Toxicity of lead: a review with recent updates. Interdiscip Toxicol. 2012;5:47–58.
Sun L, Yuan J-L, Chen Q-C, Xiao W-K, Ma G-P, Liang J-H, et al. Red meat consumption and risk for dyslipidaemia and inflammation: a systematic review and meta-analysis. Front Cardiovasc Med. 2022;9:996467.
Kuang H, Yang F, Zhang Y, Wang T, Chen G. The impact of egg nutrient composition and its consumption on cholesterol homeostasis. Cholesterol. 2018;2018:6303810.
Kiesswetter E, Stadelmaier J, Petropoulou M, Morze J, Grummich K, Roux I, et al. Effects of dairy intake on markers of cardiometabolic health in adults: a systematic review with network meta-analysis. Adv Nutr. 2023;14:438–50.
Giosuè A, Calabrese I, Vitale M, Riccardi G, Vaccaro O. Consumption of dairy foods and cardiovascular disease: a systematic review. Nutrients. 2022;14:831.
Radkhah N, Zarezadeh M, Jamilian P, Ostadrahimi A. The effect of vitamin D supplementation on lipid profiles: an umbrella review of meta-analyses. Adv Nutr. 2023;14:1479–98.
Dludla PV, Nkambule BB, Nyambuya TM, Ziqubu K, Mabhida SE, Mxinwa V, et al. Vitamin C intake potentially lowers total cholesterol to improve endothelial function in diabetic patients at increased risk of cardiovascular disease: a systematic review of randomized controlled trials. Front Nutr. 2022;9:1011002.
Urbano T, Filippini T, Lasagni D, De Luca T, Sucato S, Polledri E, et al. Associations between urinary and dietary selenium and blood metabolic parameters in a healthy northern Italy population. Antioxidants. 2021;10:1193.
Ma X, Jiang S, Yan S, Li M, Wang C, Pan Y, et al. Association between copper, zinc, iron, and selenium intakes and TC/HDL-C ratio in US adults. Biol Trace Elem Res. 2020;197:43–51.
Abasilim C, Persky V, Turyk ME. Association of Blood Total Mercury with Dyslipidemia in a sample of US Adolescents: results from the National Health and Nutrition Examination Survey Database, 2011–2018. Hyg Environ Health Adv. 2023;6:100047.
Ge X, Yang A, Huang S, Luo X, Hou Q, Huang L, et al. Sex-specific associations of plasma metals and metal mixtures with glucose metabolism: an occupational population-based study in China. Sci Total Environ. 2021;760:143906.
Jin T, Park EY, Kim B, Oh J-K. Association between blood mercury concentration and prevalence of borderline hypercholesterolemia among adolescents: the Korea National Health and Nutrition Examination Survey (KNHANES) 2010-2013 and 2016. Toxics. 2021;9:242.
Frei B, Forte TM, Ames BN, Cross CE. Gas phase oxidants of cigarette smoke induce lipid peroxidation and changes in lipoprotein properties in human blood plasma. Protective effects of ascorbic acid. Biochem J. 1991;277:133–8.
Church DF, Pryor WA. Free-radical chemistry of cigarette smoke and its toxicological implications. Environ Health Perspect. 1985;64:111–26.
Pryor WA, Hales BJ, Premovic PI, Church DF. The radicals in cigarette tar: their nature and suggested physiological implications. Science. 1983;220:425–7.
Pryor WA, Stone K, Zang LY, Bermúdez E. Fractionation of aqueous cigarette tar extracts: fractions that contain the tar radical cause DNA damage. Chem Res Toxicol. 1998;11:441–8.
Yıldırım F, Sermetow K, Aycicek A, Kocyigit A, Erel O. Increased oxidative stress in preschool children exposed to passive smoking. J Pediatr. 2011;87:523–8.
Shermatov K, Zeyrek D, Yildirim F, Kilic M, Cebi N, Kocyigit A. DNA damage in children exposed to secondhand cigarette smoke and its association with oxidative stress. Indian Pediatr. 2012;49:958–62.
Smoking and Inflammation. PLoS Med. 2005;2:e198.
Lee J, Taneja V, Vassallo R. Cigarette smoking and inflammation. J Dent Res. 2012;91:142–9.
van der Vaart H, Postma DS, Timens W, ten Hacken NH. Acute effects of cigarette smoke on inflammation and oxidative stress: a review. Thorax. 2004;59:713–21.
García OP, Long KZ, Rosado JL. Impact of micronutrient deficiencies on obesity. Nutr Rev. 2009;67:559–72.
Klop B, Elte JWF, Cabezas MC. Dyslipidemia in obesity: mechanisms and potential targets. Nutrients. 2013;5:1218–40.
Tinkov AA, Aschner M, Ke T, Ferrer B, Zhou J-C, Chang J-S, et al. Adipotropic effects of heavy metals and their potential role in obesity. Fac Rev. 2021;10:32.
Bobb J _bkmr: Bayesian Kernel Machine Regression_. R package version 0.2.2. 2022. https://CRAN.R-project.org/package=bkmr.
Keil A _qgcomp: Quantile G-Computation_. R package version 2.10.1. 2022. https://CRAN.R-project.org/package=qgcomp.
Burk RF. Selenium, an antioxidant nutrient. Nutr Clin Care. 2002;5:75–79.
Papp LV, Lu J, Holmgren A, Khanna KK. From selenium to selenoproteins: synthesis, identity, and their role in human health. Antioxid Redox Signal. 2007;9:775–806.
Barceloux DG. Selenium. J Toxicol Clin Toxicol. 1999;37:145–72.
Filippini T, Michalke B, Wise LA, Malagoli C, Malavolti M, Vescovi L, et al. Diet composition and serum levels of selenium species: a cross-sectional study. Food Chem Toxicol. 2018;115:482–90.
Filippini T, Cilloni S, Malavolti M, Violi F, Malagoli C, Tesauro M, et al. Dietary intake of cadmium, chromium, copper, manganese, selenium and zinc in a Northern Italy community. J Trace Elem Med Biol. 2018;50:508–17.
Stoffaneller R, Morse NL. A review of dietary selenium intake and selenium status in Europe and the Middle East. Nutrients. 2015;7:1494–537.
Letsiou S, Nomikos T, Panagiotakos D, Pergantis SA, Fragopoulou E, Antonopoulou S, et al. Dietary habits of Greek adults and serum total selenium concentration: the ATTICA study. Eur J Nutr. 2010;49:465–72.
Godos J, Giampieri F, Micek A, Battino M, Forbes-Hernández TY, Quiles JL, et al. Effect of Brazil nuts on selenium status, blood lipids, and biomarkers of oxidative stress and inflammation: a systematic review and meta-analysis of randomized clinical trials. Antioxidants. 2022;11:403.
Bleys J, Navas-Acien A, Guallar E. Serum selenium and diabetes in U.S. adults. Diabetes Care. 2007;30:829–34.
Laclaustra M, Navas-Acien A, Stranges S, Ordovas JM, Guallar E. Serum selenium concentrations and diabetes in U.S. adults: National Health and Nutrition Examination Survey (NHANES) 2003–2004. Environ Health Perspect. 2009;117:1409–13.
Bleys J, Navas-Acien A, Stranges S, Menke A, Miller ER, Guallar E. Serum selenium and serum lipids in US adults. Am J Clin Nutr. 2008;88:416–23.
Laclaustra M, Stranges S, Navas-Acien A, Ordovas JM, Guallar E. Serum selenium and serum lipids in US adults: National Health and Nutrition Examination Survey (NHANES) 2003-2004. Atherosclerosis. 2010;210:643–8.
Stranges S, Laclaustra M, Ji C, Cappuccio FP, Navas-Acien A, Ordovas JM, et al. Higher selenium status is associated with adverse blood lipid profile in British adults. J Nutr. 2010;140:81–87.
Stranges S, Marshall JR, Natarajan R, Donahue RP, Trevisan M, Combs GF, et al. Effects of long-term selenium supplementation on the incidence of type 2 diabetes: a randomized trial. Ann Intern Med. 2007;147:217–23.
Stranges S, Sieri S, Vinceti M, Grioni S, Guallar E, Laclaustra M, et al. A prospective study of dietary selenium intake and risk of type 2 diabetes. BMC Public Health. 2010;10:564.
Ju W, Ji M, Li X, Li Z, Wu G, Fu X, et al. Relationship between higher serum selenium level and adverse blood lipid profile. Clin Nutr. 2018;37:1512–7.
Vinceti M, Filippini T, Cilloni S, Crespi CM. The epidemiology of selenium and human cancer. Adv Cancer Res. 2017;136:1–48.
Vinceti M, Filippini T, Wise LA. Environmental selenium and human health: an update. Curr Environ Health Rep. 2018;5:464–85.
Stahel P, Kim JJ, Cieslar SRL, Warrington JM, Xiao C, Cant JP. Supranutritional selenium intake from enriched milk casein impairs hepatic insulin sensitivity via attenuated IRS/PI3K/AKT signaling and decreased PGC-1α expression in male Sprague-Dawley rats. J Nutr Biochem. 2017;41:142–50.
Bi C-L, Wang H, Wang Y-J, Sun J, Dong J-S, Meng X, et al. Selenium inhibits Staphylococcus aureus-induced inflammation by suppressing the activation of the NF-κB and MAPK signalling pathways in RAW264.7 macrophages. Eur J Pharm. 2016;780:159–65.
Nazıroglu M. Role of selenium on calcium signaling and oxidative stress-induced molecular pathways in epilepsy. Neurochem Res. 2009;34:2181–91.
Galan-Chilet I, Tellez-Plaza M, Guallar E, De Marco G, Lopez-Izquierdo R, Gonzalez-Manzano I, et al. Plasma selenium levels and oxidative stress biomarkers: a gene-environment interaction population-based study. Free Radic Biol Med. 2014;74:229–36.
Yang Z, Yan C, Liu G, Niu Y, Zhang W, Lu S, et al. Plasma selenium levels and nonalcoholic fatty liver disease in Chinese adults: a cross-sectional analysis. Sci Rep. 2016;6:37288.
Wang X, Seo YA, Park SK. Serum selenium and non-alcoholic fatty liver disease (NAFLD) in U.S. adults: National Health and Nutrition Examination Survey (NHANES) 2011–2016. Environ Res. 2021;197:111190.
Dhingra S, Bansal MP. Hypercholesterolemia and LDL receptor mRNA expression: modulation by selenium supplementation. Biometals. 2006;19:493–501.
Nassir F, Moundras C, Bayle D, Sérougne C, Gueux E, Rock E, et al. Effect of selenium deficiency on hepatic lipid and lipoprotein metabolism in the rat. Br J Nutr. 1997;78:493–500.
Magnussen CG, Venn A, Thomson R, Juonala M, Srinivasan SR, Viikari JSA, et al. The association of pediatric low- and high-density lipoprotein cholesterol dyslipidemia classifications and change in dyslipidemia status with carotid intima-media thickness in adulthood evidence from the cardiovascular risk in Young Finns study, the Bogalusa Heart study, and the CDAH (Childhood Determinants of Adult Health) study. J Am Coll Cardiol. 2009;53:860–9.
Raitakari O, Kartiosuo N, Pahkala K, Hutri-Kähönen N, Bazzano LA, Chen W, et al. Lipoprotein(a) in youth and prediction of major cardiovascular outcomes in adulthood. Circulation. 2023;147:23–31.
Whanger P, Vendeland S, Park YC, Xia Y. Metabolism of subtoxic levels of selenium in animals and humans. Ann Clin Lab Sci. 1996;26:99–113.
Fang H, He X, Wu Y, Chen S, Zhang M, Pan F, et al. Association between selenium level in blood and glycolipid metabolism in residents of Enshi prefecture, China. Biol Trace Elem Res. 2021;199:2456–66.
Fan Y, Zhang C, Bu J. Relationship between selected serum metallic elements and obesity in children and adolescent in the U.S. Nutrients. 2017;9:104.
Longnecker MP, Stram DO, Taylor PR, Levander OA, Howe M, Veillon C, et al. Use of selenium concentration in whole blood, serum, toenails, or urine as a surrogate measure of selenium intake. Epidemiology. 1996;7:384–90.
Nawrot TS, Staessen JA, Roels HA, Den Hond E, Thijs L, Fagard RH, et al. Blood pressure and blood selenium: a cross-sectional and longitudinal population study. Eur Heart J. 2007;28:628–33.
Li J, Lo K, Shen G, Feng Y-Q, Huang Y-Q. Gender difference in the association of serum selenium with all-cause and cardiovascular mortality. Postgrad Med. 2020;132:148–55.
R Cardoso B, Hare DJ, Macpherson H. Sex-dependent association between selenium status and cognitive performance in older adults. Eur J Nutr. 2021;60:1153–9.
Angstwurm MWA, Engelmann L, Zimmermann T, Lehmann C, Spes CH, Abel P, et al. Selenium in Intensive Care (SIC): results of a prospective randomized, placebo-controlled, multiple-center study in patients with severe systemic inflammatory response syndrome, sepsis, and septic shock. Crit Care Med. 2007;35:118–26.
Zhang J-W, Lin Y, Liu Y-M, Wang M-M, Gong J-G, Shen X-G, et al. Excess selenium intake is associated with microalbuminuria in female but not in male among adults with obesity: results from NHANES 2009-2018. Front Nutr. 2023;10:1043395.
Kander MC, Cui Y, Liu Z. Gender difference in oxidative stress: a new look at the mechanisms for cardiovascular diseases. J Cell Mol Med. 2017;21:1024–32.
Riese C, Michaelis M, Mentrup B, Götz F, Köhrle J, Schweizer U, et al. Selenium-dependent pre- and posttranscriptional mechanisms are responsible for sexual dimorphic expression of selenoproteins in murine tissues. Endocrinology. 2006;147:5883–92.
Schomburg L. Selene, the goddess of the moon: does she shine on men only? Eur Heart J. 2007;28:2043–4.
Järup L, Akesson A. Current status of cadmium as an environmental health problem. Toxicol Appl Pharm. 2009;238:201–8.
Agency for Toxic Substances and Disease Registry (ATSDR). ATSDR’s substance priority list. https://www.atsdr.cdc.gov/spl/index.html. Accessed 19 May 2023.
Tinkov AA, Filippini T, Ajsuvakova OP, Skalnaya MG, Aaseth J, Bjørklund G, et al. Cadmium and atherosclerosis: a review of toxicological mechanisms and a meta-analysis of epidemiologic studies. Environ Res. 2018;162:240–60.
Samarghandian S, Azimi-Nezhad M, Shabestari MM, Azad FJ, Farkhondeh T, Bafandeh F. Effect of chronic exposure to cadmium on serum lipid, lipoprotein and oxidative stress indices in male rats. Interdiscip Toxicol. 2015;8:151–4.
Zwolak I, Zaporowska H. Selenium interactions and toxicity: a review. Selenium interactions and toxicity. Cell Biol Toxicol. 2012;28:31–46.
Zwolak I. The role of selenium in arsenic and cadmium toxicity: an updated review of scientific literature. Biol Trace Elem Res. 2020;193:44–63.
Parízek J, Ostádalová I, Benes I, Babický A. Pregnancy and trace elements: the protective effect of compounds of an essential trace element–selenium–against the peculiar toxic effects of cadmium during pregnancy. J Reprod Fertil. 1968;16:507–9.
Li L-L, Cui Y-H, Lu L-Y, Liu Y-L, Zhu C-J, Tian L-J, et al. Selenium stimulates cadmium detoxification in caenorhabditis elegans through thiols-mediated nanoparticles formation and secretion. Environ Sci Technol. 2019;53:2344–52.
Al-Saleh I, Al-Rouqi R, Obsum CA, Shinwari N, Mashhour A, Billedo G, et al. Interaction between cadmium (Cd), selenium (Se) and oxidative stress biomarkers in healthy mothers and its impact on birth anthropometric measures. Int J Hyg Environ Health. 2015;218:66–90.
Everson TM, Kappil M, Hao K, Jackson BP, Punshon T, Karagas MR, et al. Maternal exposure to selenium and cadmium, fetal growth, and placental expression of steroidogenic and apoptotic genes. Environ Res. 2017;158:233–44.
Wang Y, Wu Y, Luo K, Liu Y, Zhou M, Yan S, et al. The protective effects of selenium on cadmium-induced oxidative stress and apoptosis via mitochondria pathway in mice kidney. Food Chem Toxicol. 2013;58:61–67.
Zhou Y-J, Zhang S-P, Liu C-W, Cai Y-Q. The protection of selenium on ROS mediated-apoptosis by mitochondria dysfunction in cadmium-induced LLC-PK(1) cells. Toxicol Vitr. 2009;23:288–94.
Liu L, Zhang J, Zhang Z, Yao H, Sun G, Xu S. Protective roles of selenium on nitric oxide-mediated apoptosis of immune organs induced by cadmium in chickens. Biol Trace Elem Res. 2014;159:199–209.
Yu R, Chen X. [Effects of selenium on rat hepatocellular DNA damage, apoptosis and changes of cell cycle induced by cadmium in vivo]. Zhonghua Yu Fang Yi Xue Za Zhi. 2004;38:155–8.
Wahba ZZ, Coogan TP, Rhodes SW, Waalkes MP. Protective effects of selenium on cadmium toxicity in rats: role of altered toxicokinetics and metallothionein. J Toxicol Environ Health. 1993;38:171–82.
Battin EE, Perron NR, Brumaghim JL. The central role of metal coordination in selenium antioxidant activity. Inorg Chem. 2006;45:499–501.
Zhang C, Lin J, Ge J, Wang L-L, Li N, Sun X-T, et al. Selenium triggers Nrf2-mediated protection against cadmium-induced chicken hepatocyte autophagy and apoptosis. Toxicol Vitr. 2017;44:349–56.
Filippidis FT, Vardavas CI, Loukopoulou A, Behrakis P, Connolly GN, Tountas Y. Prevalence and determinants of tobacco use among adults in Greece: 4 year trends. Eur J Public Health. 2013;23:772–6.
Passa A, Agtzidis L, Tsaousidou M, Passa KF. The attitudes of Greeks towards second-hand smoke and the anti-tobacco legislation. https://doi.org/10.1101/2020.11.26.20234666. Accessed 20 Feb 2024.
Raghuveer G, White DA, Hayman LL, Woo JG, Villafane J, Celermajer D, et al. Cardiovascular consequences of childhood secondhand tobacco smoke exposure: prevailing evidence, burden, and racial and socioeconomic disparities: a scientific statement from the American Heart Association. Circulation. 2016;134:e336–e359.
Thompson FE, Patterson BH, Weinstein SJ, McAdams M, Spate VL, Hamman RF, et al. Serum selenium and the risk of cervical cancer among women in the United States. Cancer Causes Control. 2002;13:517–26.
Kim Y, Wei J, Citronberg J, Hartman T, Fedirko V, Goodman M. Relation of vitamin E and selenium exposure to prostate cancer risk by smoking status: a review and meta-analysis. Anticancer Res. 2015;35:4983–96.
Cassano PA, Guertin KA, Kristal AR, Ritchie KE, Bertoia ML, Arnold KB, et al. A randomized controlled trial of vitamin E and selenium on rate of decline in lung function. Respir Res. 2015;16:35.
Al-Mubarak AA, Grote Beverborg N, Suthahar N, Gansevoort RT, Bakker SJL, Touw DJ, et al. High selenium levels associate with reduced risk of mortality and new-onset heart failure: data from PREVEND. Eur J Heart Fail. 2022;24:299–307.
Gümüştekín K, Seven B, Karabulut N, Aktaş O, Gürsan N, Aslan S, et al. Effects of sleep deprivation, nicotine, and selenium on wound healing in rats. Int J Neurosci. 2004;114:1433–42.
Sreekala S, Indira M. Effects of exogenous selenium on nicotine-induced oxidative stress in rats. Biol Trace Elem Res. 2009;130:62–71.
Alfaradhi MZ, Fernandez-Twinn DS, Martin-Gronert MS, Musial B, Fowden A, Ozanne SE. Oxidative stress and altered lipid homeostasis in the programming of offspring fatty liver by maternal obesity. Am J Physiol Regul Integr Comp Physiol. 2014;307:R26–34.
Trapani L, Segatto M, Pallottini V. Regulation and deregulation of cholesterol homeostasis: the liver as a metabolic “power station”. World J Hepatol. 2012;4:184–90.
Ali W, Zhang H, Junaid M, Mao K, Xu N, Chang C, et al. Insights into the mechanisms of arsenic-selenium interactions and the associated toxicity in plants, animals, and humans: a critical review. Crit Rev Environ Sci Technol. 2021;51:704–50.
Karavoltsos S, Sakellari A, Mihopoulos N, Dassenakis M, Scoullos MJ. Evaluation of the quality of drinking water in regions of Greece. Desalination. 2008;224:317–29.
Miklavčič A, Casetta A, Snoj Tratnik J, Mazej D, Krsnik M, Mariuz M, et al. Mercury, arsenic and selenium exposure levels in relation to fish consumption in the Mediterranean area. Environ Res. 2013;120:7–17.
Vardavas C, Patelarou E, Chatzi L, Vrijheid M, Koutis A, Fthenou E, et al. Determinants of blood cadmium, lead, arsenic, uranium, mercury and molybdenum levels among pregnant women in Crete, Greece. Epidemiology. 2009;20:S174.
Vardavas CI, Patelarou E, Grandér M, Chatzi L, Palm B, Fthenou E, et al. The association between active/passive smoking and toxic metals among pregnant women in Greece. Xenobiotica. 2011;41:456–63.
Stratakis N, Conti DV, Borras E, Sabido E, Roumeliotaki T, Papadopoulou E, et al. Association of fish consumption and mercury exposure during pregnancy with metabolic health and inflammatory biomarkers in children. JAMA Netw Open. 2020;3:e201007.
Cho HW, Kim S-H, Park MJ. An association of blood mercury levels and hypercholesterolemia among Korean adolescents. Sci Total Environ. 2020;709:135965.
Zhang Y, Xu C, Fu Z, Shu Y, Zhang J, Lu C, et al. Associations between total mercury and methyl mercury exposure and cardiovascular risk factors in US adolescents. Environ Sci Pollut Res Int. 2018;25:6265–72.
Buhari O, Dayyab FM, Igbinoba O, Atanda A, Medhane F, Faillace RT. The association between heavy metal and serum cholesterol levels in the US population: National Health and Nutrition Examination Survey 2009-2012. Hum Exp Toxicol. 2020;39:355–64.
Liu Y, Ettinger AS, Téllez-Rojo M, Sánchez BN, Zhang Z, Cantoral A, et al. Prenatal lead exposure, type 2 diabetes, and Cardiometabolic risk factors in Mexican children at age 10-18 years. J Clin Endocrinol Metab. 2020;105:210–8.
Steiner MJ, Skinner AC, Perrin EM. Fasting might not be necessary before lipid screening: a nationally representative cross-sectional study. Pediatrics. 2011;128:463–70.
Filippini T, Ferrari A, Michalke B, Grill P, Vescovi L, Salvia C, et al. Toenail selenium as an indicator of environmental exposure: a cross-sectional study. Mol Med Rep. 2017;15:3405–12.
Yu R, Wang Z, Ma M, Xu P, Liu L, Tinkov AA, et al. Associations between circulating SELENOP level and disorders of glucose and lipid metabolism: a meta-analysis. Antioxidants. 2022;11:1263.
Mozaffarian D, Rimm EB. Fish intake, contaminants, and human health: evaluating the risks and the benefits. JAMA. 2006;296:1885–99.
Golding J, Taylor C, Iles-Caven Y, Gregory S. The benefits of fish intake: Results concerning prenatal mercury exposure and child outcomes from the ALSPAC prebirth cohort. NeuroToxicology. 2022;91:22–30.
Amigó N, Akinkuolie AO, Chiuve SE, Correig X, Cook NR, Mora S. Habitual fish consumption, n‐3 fatty acids, and nuclear magnetic resonance lipoprotein subfractions in women. J Am Heart Assoc. 2020;9:e014963.
Navas-Acien A, Francesconi KA, Silbergeld EK, Guallar E. Seafood intake and urine concentrations of total arsenic, dimethylarsinate and arsenobetaine in the US population. Environ Res. 2011;111:110–8.
Signes-Pastor AJ, Romano ME, Jackson B, Braun JM, Yolton K, Chen A, et al. Associations of maternal urinary arsenic concentrations during pregnancy with childhood cognitive abilities: the HOME study. Int J Hyg Environ Health. 2022;245:114009.
Acknowledgements
The Rhea project was financially supported by Horizon 2020—European Framework Programme for Research and Innovation, ATHLETE, the European Union (grant numbers EU FP6–2003-Food-3-NewGeneris, EU FP6. STREP Hiwate, EU FP7 ENV.2007.1.2.2.2. Project No 211250 Escape, EU FP7–2008-ENV-1.2.1.4 Envirogenomarkers, EU FP7-HEALTH-2009- single stage CHICOS, EU FP7 ENV.2008.1.2.1.6. Proposal No 226285 ENRIECO, EU- FP7- HEALTH-2012 Proposal No 308333 HELIX), and the Greek Ministry of Health. The present study was also funded by Karolinska Institutet and the Swedish Research Council (Project No. 2015-03655). LC was financially supported by NIEHS (grant numbers R01ES030691, R01ES029944, R01 ES030364, P30ES007048, R01ES016813), CGH is supported by a NIH Pathway to Independence Award (R00 ES030400). We would like to thank the Rhea cohort study participants, as well as our colleagues, medical, nursing, and research staff, for their contributions to this study.
Author information
Authors and Affiliations
Contributions
GY: Formal analysis, Visualization, Writing—original draft. KM: Data curation, Writing—review & editing. MER: Writing—review & editing. MK: Writing—review & editing. MV: Writing—review & editing. TR: Data curation, Writing—review & editing. VB: Investigation, Writing—review & editing. SFF: Conceptualization, Writing—review & editing. LC: Supervision, Funding acquisition, Writing—review & editing. CGH: Conceptualization, Supervision, Writing—review & editing.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Yim, G., Margetaki, K., Romano, M.E. et al. Metal mixture exposures and serum lipid levels in childhood: the Rhea mother-child cohort in Greece. J Expo Sci Environ Epidemiol (2024). https://doi.org/10.1038/s41370-024-00674-x
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41370-024-00674-x