Abstract
Background
Prescribed agricultural burning is a common land management practice, but little is known about the health effects from the resulting smoke exposure.
Objective
To examine the association between smoke from prescribed burning and cardiorespiratory outcomes in the U.S. state of Kansas.
Methods
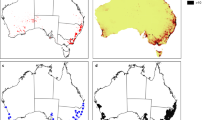
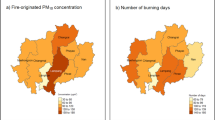
We analyzed a zip code-level, daily time series of primary cardiorespiratory emergency department (ED) visits for February–May (months when prescribed burning is common in Kansas) in the years 2009–2011 (n = 109,220). Given limited monitoring data, we formulated a measure of smoke exposure using non-traditional datasets, including fire radiative power and locational attributes from remote sensing data sources. We then assigned a population-weighted potential smoke impact factor (PSIF) to each zip code, based on fire intensity, smoke transport, and fire proximity. We used Poisson generalized linear models to estimate the association between PSIF on the same day and in the past 3 days and asthma, respiratory including asthma, and cardiovascular ED visits.
Results
During the study period, prescribed burning took place on approximately 8 million acres in Kansas. Same-day PSIF was associated with a 7% increase in the rate of asthma ED visits when adjusting for month, year, zip code, meteorology, day of week, holidays, and correlation within zip codes (rate ratio [RR]: 1.07; 95% confidence interval [CI]: 1.01, 1.13). Same-day PSIF was not associated with a combined outcome of respiratory ED visits (RR [95% CI]: 0.99 [0.97, 1.02]), or cardiovascular ED visits (RR [95% CI]: 1.01 [0.98, 1.04]). There was no consistent association between PSIF during the past 3 days and any of the outcomes.
Significance
These results suggest an association between smoke exposure and asthma ED visits on the same day. Elucidating these associations will help guide public health programs that address population-level exposure to smoke from prescribed burning.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 6 print issues and online access
$259.00 per year
only $43.17 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
Data availability
The computing code can be obtained by contacting the corresponding author. The data are not available because they include medical information that cannot be released.
References
Fann N, Alman B, Broome RA, Morgan GG, Johnston FH, Pouliot G, et al. The health impacts and economic value of wildland fire episodes in the U.S.: 2008-2012. Sci Total Environ. 2018;610-611:802–9.
Cascio WE. Wildland fire smoke and human health. Sci Total Environ. 2018;624:586–95.
Centers for Disease Control and Prevention. Protect Yourself from Wildfire Smoke. 2021. https://www.cdc.gov/nceh/features/wildfires/. Accessed March 15, 2021.
Ohlenbusch PD, Hartnet DC Prescribed burning as a management practice. Kansas State University, 2000.
U.S. Environmental Protection Agency. Agriculture and Air Quality: Prescribed Burning. 2021. https://www.epa.gov/agriculture/agriculture-and-air-quality#prescribedburning. Accessed June 28, 2021.
World Health Organization. Air quality and health. 2022. https://www.who.int/teams/environment-climate-change-and-health/air-quality-and-health/health-impacts. Accessed December 8, 2022.
Haikerwal A, Reisen F, Sim MR, Abramson MJ, Meyer CP, Johnston FH, et al. Impact of smoke from prescribed burning: Is it a public health concern? J Air Waste Manag Assoc. 2015;65:592–8.
Tian D, Wang Y, Bergin M, Hu Y, Liu Y, Russell AG. Air quality impacts from prescribed forest fires under different management practices. Environ Sci Technol. 2008;42:2767–72.
Hu Y, Odman MT, Chang ME, Jackson W, Lee S, Edgerton ES, et al. Simulation of air quality impacts from prescribed fires on an urban area. Environ Sci Technol. 2008;42:3676–82.
Whitehill AR, George I, Long R, Baker KR, Landis M. Volatile organic compound emissions from prescribed burning in Tallgrass Prairie ecosystems. Atmos. 2019;10:1–464.
Robinson MS, Chavez J, Velazquez S, Jayanty RK. Chemical speciation of PM2.5 collected during prescribed fires of the Coconino National Forest near Flagstaff, Arizona. J Air Waste Manag Assoc. 2004;54:1112–23.
Jaffe DA, O’Neill SM, Larkin NK, Holder AL, Peterson DL, Halofsky JE, et al. Wildfire and prescribed burning impacts on air quality in the United States. J Air Waste Manag Assoc. 2020;70:583–615.
Huang R, Hu Y, Russell AG, Mulholland JA, Odman MT The impacts of prescribed fire on PM2.5 air quality and human health: application to asthma-related emergency room visits in Georgia, USA. Int J Environ Res Public Health 2019;16:1–14.
Afrin S, Garcia-Menendez F. Potential impacts of prescribed fire smoke on public health and socially vulnerable populations in a Southeastern U.S. state. Sci Total Environ. 2021;794:148712.
Ravi V, Vaughan JK, Wolcott MP, Lamb BK. Impacts of prescribed fires and benefits from their reduction for air quality, health and visibility in the Pacific Northwest of the United States. J Air Waste Manag Assoc 2018; https://doi.org/10.1080/10962247.2018.1526721.
Mohler RL, Goodin DG. Mapping burned areas in the Flint Hills of Kansas and Oklahoma, 2000—2010. Great Plains. Research. 2012;22:15–25.
Anderson KL. Utilization of grasslands in the flint hills of Kansas. J Range Manag. 1953;6:86–93.
Kansas Department of Health and Environment. State of Kansas Flint Hills Smoke Management Plan. 2010. https://www.kdheks.gov/bar/air-monitor/flinthillsinfo/SMP_v10FINAL.pdf. Accessed June 28, 2010.
Liu Z Air quality concerns of prescribed range burning in Kansas. MF3121.: Manhattan, Kansas, 2014.
Liu Z, Liu Y, Maghirang R, Devlin D, Blocksome C. Estimating contributions of prescribed rangeland burning in Kansas to ambient PM2.5 through source apportionment with the Unmix receptor model. Trans ASABE. 2016;59:1267–75.
U.S. Environmental Protection Agency. 2017 National Emissions Inventory (NEI) Data. 2020. https://www.epa.gov/air-emissions-inventories/2017-national-emissions-inventory-nei-data. Accessed June 17, 2020.
National Aeronautics and Space Administration. Fire Information for Resource Management System (FIRMS). 2021. https://earthdata.nasa.gov/earth-observation-data/near-real-time/firms. Accessed April 22, 2021.
Li F, Zhang X, Roy DP, Kondragunta S. Estimation of biomass-burning emissions by fusing the fire radiative power retrievals from polar-orbiting and geostationary satellites across the conterminous United States. Atmos Environ. 2019;211:274–87.
Mota B, Wooster MJ. A new top-down approach for directly estimating biomass burning emissions and fuel consumption rates and totals from geostationary satellite fire radiative power (FRP). Remote Sens Environ. 2018;206:45–62.
Ichoku C, Ellison L. Global top-down smoke-aerosol emissions estimation using satellite fire radiative power measurements. Atmos Chem Phys. 2014;14:6643–67.
Ichoku C, Giglio L, Wooster MJ, Remer LA. Global characterization of biomass-burning patterns using satellite measurements of fire radiative energy. Remote Sens Environ. 2008;112:2950–62.
Waller LA, Louis TA, Carlin BP. Environmental justice and statistical summaries of differences in exposure distributions. J Expo Anal Environ Epidemiol. 1999;9:56–65.
National Aeronautics and Space Administration. Land Data Assimilation System. 2022. https://ldas.gsfc.nasa.gov/. Accessed July 14, 2022.
Zou B, Wilson JG, Zhan FB, Zeng Y. Air pollution exposure assessment methods utilized in epidemiological studies. J Environ Monit. 2009;11:475–90.
Li L, Losser T, Yorke C, Piltner R. Fast inverse distance weighting-based spatiotemporal interpolation: a web-based application of interpolating daily fine particulate matter PM2:5 in the contiguous U.S. using parallel programming and k-d tree. Int J Environ Res Public Health. 2014;11:9101–41.
Ye D, Klein M, Chang HH, Sarnat JA, Mulholland JA, Edgerton ES, et al. Estimating acute cardiorespiratory effects of ambient volatile organic compounds. Epidemiology. 2017;28:197–206.
Flanders WD, Strickland MJ, Klein M. A new method for partial correction of residual confounding in time-series and other observational studies. Am J Epidemiol. 2017;185:941–9.
Lipsitch M, Tchetgen Tchetgen E, Cohen T. Negative controls: a tool for detecting confounding and bias in observational studies. Epidemiology. 2010;21:383–8.
Flanders WD, Klein M, Darrow LA, Strickland MJ, Sarnat SE, Sarnat JA, et al. A method for detection of residual confounding in time-series and other observational studies. Epidemiology. 2011;22:59–67.
R Core Team. R: A language and environment for statistical computing. In. Vienna, Austria: R Foundation for Statistical Computing, 2021.
Kansas Department of Health and Environment. Flint Hills Wildland Fire Update. 2021 Summary. 2021. https://www.ksfire.org/new-media-archives/weeklyupdates/2021/Flint_Hills-Wildland_Fire_2021_Summary.pdf. Accessed March 15, 2021.
Towne EG, Craine JM. Ecological consequences of shifting the timing of burning tallgrass prairie. PLoS One. 2014;9:e103423.
Duncan ZM, Tajchman AJ, Ramirez MP, Lemmon J, Hollenbeck WR, Blasi DA, et al. Effects of prescribed fire timing on grazing performance of yearling beef cattle, forage biomass accumulation, and plant community characteristics on native tallgrass prairie in the Kansas Flint Hills. Transl Anim Sci. 2021;5:txab077.
Pate CA, Zahran HS, Qin X, Johnson C, Hummelman E, Malilay J. Asthma Surveillance—United States, 2006-2018. MMWR Surveill Summ. 2021;70:1–32.
Tsao CW, Aday AW, Almarzooq ZI, Alonso A, Beaton AZ, Bittencourt MS, et al. Heart Disease and Stroke Statistics-2022 Update: A Report From the American Heart Association. Circulation. 2022;145:e153–e639.
Acknowledgements
The authors thank Dr. Mitchel Klein for his assistance with the SAS programming for this analysis. The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention. This publication was supported by the Kansas Environmental Public Health Tracking Program through Cooperative Agreement Number NUE1EH001340-01 funded by the Centers for Disease Control and Prevention. Its contents are solely the responsibility of the authors and do not necessarily represent the official views of the Centers for Disease Control and Prevention or the Department of Health and Human Services.
Author information
Authors and Affiliations
Contributions
FY, FA, and KS conceived of the work. AP, AV, AM, MM, KS, and WDF contributed to study design. FA obtained the health data. AV and AM developed the exposure estimate. AP and WDF completed the analysis. AP and AV drafted the manuscript. All authors contributed to the interpretation of results and to the revision of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare they have no competing financial interests. Dr. Flanders discloses that he owns a consulting company, Epidemiologic Research & Methods, LLC that does consulting work for clients. He knows of no conflicts with this work.
Ethical approval
This activity was reviewed by the Centers for Disease Control and Prevention (CDC) and was conducted consistent with applicable federal law and CDC (See e.g., 45 C.F.R. part 46, 21 C.F.R. part 56; 42 U.S.C. §241(d); 5 U.S.C. §552a; 44 U.S.C. §3501 et seq.).
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Pennington, A.F., Vaidyanathan, A., Ahmed, F.S. et al. Large-scale agricultural burning and cardiorespiratory emergency department visits in the U.S. state of Kansas. J Expo Sci Environ Epidemiol 33, 663–669 (2023). https://doi.org/10.1038/s41370-023-00531-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41370-023-00531-3