Abstract
Background
The association between air pollutants and psychiatric disorders has been investigated in many countries. However, results for the association between air pollutants and emergency room (ER) visits for psychiatric disorders are inconsistent. Further, systematic large-scale studies relating to the same are lacking, especially in South Korea.
Objective
We aimed to investigate the acute and short-term cumulative effect of air pollutants on ER visits for psychiatric disorders in South Korea.
Methods
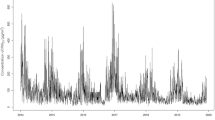
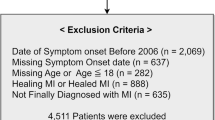
The data on nitrogen dioxide (NO2) and particulate matter (PM2.5 and PM10) and ER visits due to nine representative psychiatric disorders were collected from eight major cities in South Korea for three years. We estimated the relative risk (RR) at lag 0 and a cumulative 11-day RR by increasing a 10-unit for PM and 0.01-unit for NO2 using the Distributed Lag Nonlinear Model.
Results
During the study period, a total of 79,092 ER visits for psychiatric disorders were identified and tested for association with NO2, PM2.5, and PM10. The RR at lag 0 of depression per 0.01-unit increase in NO2 was the highest (3.127; 95% confidence interval [CI] 2.933 to 3.332) among the psychiatric disorders. The RRs at lag 0 of anxiety disorders per 10-unit increase in PM2.5 (1.709; 95% CI 1.424 to 2.053) and PM10 (2.168; 95% CI 1.957 to 2.403) were the highest among the psychiatric disorders.
Significance
Air pollutants increased ER visits for psychiatric disorders with the highest RR of depression due to NO2 and anxiety disorder due to PM2.5 and PM10. These results contribute evidence to the positive association between ambient exposure to air pollution and aggravation of psychiatric disorders, indicating air pollution may be a modifiable risk factor in mental health management.
Impact statement
We investigated the effect of air pollution on emergency room visits caused by major psychiatric disorders in prominent cities in South Korea. Using the Distributed Lag Nonlinear Model, an advanced analysis method, we calculated the acute effect and short-term cumulative effect. Air pollutants increased ER visits for psychiatric disorders with the highest relative risk of depression due to NO2 and anxiety disorder due to PM2.5 and PM10. These results reveal an association between ambient exposure to air pollution and aggravation of psychiatric disorders and suggest that air pollution may be a modifiable risk factor in mental health management.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 6 print issues and online access
$259.00 per year
only $43.17 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
World Health Organization. mhGAP: Mental Health Gap Action Programme: scaling up care for mental, neurological and substance use disorders. Geneva: World Health Organization; 2008. https://apps.who.int/iris/handle/10665/43809.
Steel Z, Marnane C, Iranpour C, Chey T, Jackson JW, Patel V, et al. The global prevalence of common mental disorders: a systematic review and meta-analysis 1980–2013. Int J Epidemiol. 2014;43:476–93. https://doi.org/10.1093/ije/dyu038.
GBD 2015 Disease and Injury Incidence and Prevalence Collaborators. Global, regional, and national incidence, prevalence, and years lived with disability for 310 diseases and injuries, 1990–2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet. 2016;388:1545–602. https://doi.org/10.1016/S0140-6736(16)31678-6.
Hazlett SB, McCarthy ML, Londner MS, Onyike CU. Epidemiology of Adult Psychiatric Visits to U.S. Emergency Departments. Article. Acad Emerg Med. 2004;11:193–5. https://doi.org/10.1197/j.aem.2003.09.014.
Theriault KM, Rosenheck RA, Rhee TG. Increasing emergency department visits for mental health conditions in the United States. J Clin Psychiatry. 2020;81:5456. https://doi.org/10.4088/JCP.20m13241.
Woo JH, Grinspan Z, Shapiro J, Rhee SY. Frequent users of hospital emergency departments in Korea characterized by claims data from the National Health Insurance: a cross sectional study. PloS one. 2016;11:e0147450. https://doi.org/10.1371/journal.pone.0147450.
Kim SH, Lee DW, Kwon J, Yang J, Park EC, Jang SI. Suicide Related Indicators and Trends in Korea in 2019. Health Policy Manag. 2021;31:232–9. https://doi.org/10.4332/KJHPA.2021.31.2.232.
Holland KM, Jones C, Vivolo-Kantor AM, Idaikkadar N, Zwald M, Hoots B, et al. Trends in US emergency department visits for mental health, overdose, and violence outcomes before and during the COVID-19 pandemic. JAMA Psychiatry. 2021;78:372–9. https://doi.org/10.1001/jamapsychiatry.2020.4402.
Buoli M, Grassi S, Caldiroli A, Carnevali GS, Mucci F, Iodice S, et al. Is there a link between air pollution and mental disorders? Environ Int. 2018;118:154–68. https://doi.org/10.1016/j.envint.2018.05.044.
Ha J, Yang HS. The Werther effect of celebrity suicides: Evidence from South Korea. PLoS ONE. 2021;16:e0249896. https://doi.org/10.1371/journal.pone.0249896.
Min M, Shi T, Ye P, Wang Y, Yao Z, Tian S, et al. Effect of apparent temperature on daily emergency admissions for mental and behavioral disorders in Yancheng, China: a time-series study. Environ Health. 2019;18:1–12. https://doi.org/10.1186/s12940-019-0543-x.
GBD 2016 Occupational Chronic Respiratory Risk Factors Collaborators; GBD 2016 occupational chronic respiratory risk factors collaborators. Global and regional burden of chronic respiratory disease in 2016 arising from non-infectious airborne occupational exposures: a systematic analysis for the global burden of disease study 2016. Occup Environ Med. 2020;77:142–50. https://doi.org/10.1136/oemed-2019-106013.
Shapiro M Transboundary air pollution in Northeast Asia: The political economy of yellow dust, particulate matter, and PM2. 5. Washington: Korean Economic Institute of America; 2016. pp 1-11. https://keia.org/publication/transboundary-air-pollution-in-northeast-asia-the-political-economy-of-yellow-dust-particulate-matter-and-pm2-5/.
World Health Organization. WHO global air quality guidelines: particulate matter (PM2. 5 and PM10), ozone, nitrogen dioxide, sulfur dioxide and carbon monoxide. Geneva: World Health Organization; 2021. https://apps.who.int/iris/handle/10665/345329.
Thilakaratne RA, Malig BJ, Basu R. Examining the relationship between ambient carbon monoxide, nitrogen dioxide, and mental health-related emergency department visits in California, USA. Sci Total Environ. 2020;746:140915. https://doi.org/10.1016/j.scitotenv.2020.140915.
Szyszkowicz M, Rowe BH, Colman I. Air pollution and daily emergency department visits for depression. Int J Occup Med Environ Health. 2009;22:355–62. https://doi.org/10.2478/v10001-009-0031-6.
Oudin A, Åström DO, Asplund P, Steingrimsson S, Szabo Z, Carlsen HK. The association between daily concentrations of air pollution and visits to a psychiatric emergency unit: a case-crossover study. Environ Health. 2018;17:4. https://doi.org/10.1186/s12940-017-0348-8.
Liu JJ, Wang F, Liu H, Wei YB, Li H, Yue J, et al. Ambient fine particulate matter is associated with increased emergency ambulance dispatches for psychiatric emergencies. Environ Res. 2019;177:108611. https://doi.org/10.1016/j.envres.2019.108611.
Gu X, Guo T, Si Y, Wang J, Zhang W, Deng F, et al. Association Between Ambient Air Pollution and Daily Hospital Admissions for Depression in 75 Chinese Cities. Am J Psychiatry. 2020;177:735–43. https://doi.org/10.1176/appi.ajp.2020.19070748.
Bernardini F, Trezzi R, Quartesan R, Attademo L. Air Pollutants and Daily Hospital Admissions for Psychiatric Care: A Review. Psychiatr Serv. 2020;71:1270–6. https://doi.org/10.1176/appi.ps.201800565.
Newbury JB, Stewart R, Fisher HL, Beevers S, Dajnak D, Broadbent M, et al. Association between air pollution exposure and mental health service use among individuals with first presentations of psychotic and mood disorders: retrospective cohort study. Br J Psychiatry. 2021;219:678–85. https://doi.org/10.1192/bjp.2021.119.
Braithwaite I, Zhang S, Kirkbride JB, Osborn DPJ, Hayes JF. Air Pollution (Particulate Matter) Exposure and Associations with Depression, Anxiety, Bipolar, Psychosis and Suicide Risk: A Systematic Review and Meta-Analysis. Environ Health Perspect. 2019;127:126002. https://doi.org/10.1289/EHP4595.
Guo Y, Gasparrini A, Armstrong B, Li S, Tawatsupa B, Tobias A, et al. Global variation in the effects of ambient temperature on mortality: a systematic evaluation. Epidemiology. 2014;25:781. https://doi.org/10.1097/EDE.0000000000000165.
Lee SW, Yon DK, James CC, Lee S, Koh HY, Sheen YH, et al. Short-term effects of multiple outdoor environmental factors on risk of asthma exacerbations: Age-stratified time-series analysis. J Allergy Clin Immunol. 2019;144:1542–50. https://doi.org/10.1016/j.jaci.2019.08.037.
Ventriglio A, Bellomo A, di Gioia I, Di Sabatino D, Favale D, De Berardis D, et al. Environmental pollution and mental health: a narrative review of literature. CNS Spectr. 2021;26:51–61. https://doi.org/10.1017/S1092852920001303.
Gasparrini A, Guo Y, Hashizume M, Lavigne E, Zanobetti A, Schwartz J, et al. Mortality risk attributable to high and low ambient temperature: a multicountry observational study. Lancet. 2015;386:369–75. https://doi.org/10.1016/S0140-6736(14)62114-0.
Guo Y, Li S, Tian Z, Pan X, Zhang J, Williams G. The burden of air pollution on years of life lost in Beijing, China, 2004-08: retrospective regression analysis of daily deaths. BMJ. 2013;347:f7139. https://doi.org/10.1136/bmj.f7139.
Li H, Zhang S, Qian ZM, Xie XH, Luo Y, Han R, et al. Short-term effects of air pollution on cause-specific mental disorders in three subtropical Chinese cities. Environ Res. 2020;191:110214. https://doi.org/10.1016/j.envres.2020.110214.
Wang KC, Lo YC, Liao CC, Jou YY, Huang HB. Associations Between Symptoms of Depression and Air Pollutant Exposure Among Older Adults: Results From the Taiwan Longitudinal Study on Aging (TLSA). Front Public Health. 2022;9:779192. https://doi.org/10.3389/fpubh.2021.779192.
Szyszkowicz M. Air pollution and emergency department visits for depression in Edmonton, Canada. Int J Occup Med Environ Health. 2007;20:241–5. https://doi.org/10.2478/v10001-007-0024-2.
Lim YH, Kim H, Kim JH, Bae S, Park HY, Hong YC. Air pollution and symptoms of depression in elderly adults. Environ Health Perspect. 2012;120:1023–8. https://doi.org/10.1289/ehp.1104100.
Lee H, Kang JM, Myung W, Choi J, Lee C, Na DL, et al. Exposure to ambient fine particles and neuropsychiatric symptoms in cognitive disorder: A repeated measure analysis from the CREDOS (Clinical Research Center for Dementia of South Korea) study. Sci Total Environ. 2019;668:411–8. https://doi.org/10.1016/j.scitotenv.2019.02.447.
Raison CL, Capuron L, Miller AH. Cytokines sing the blues: inflammation and the pathogenesis of depression. Trends Immunol. 2006;27:24–31. https://doi.org/10.1016/j.it.2005.11.006.
Sirivelu MP, MohanKumar SM, Wagner JG, Harkema JR, MohanKumar PS Activation of the stress axis and neurochemical alterations in specific brain areas by concentrated ambient particle exposure with concomitant allergic airway disease. Environ Health Perspect. 2006;870–4. https://doi.org/10.1289/ehp.8619.
van Berlo D, Albrecht C, Knaapen AM, Cassee FR, Gerlofs-Nijland ME, Kooter IM, et al. Comparative evaluation of the effects of short-term inhalation exposure to diesel engine exhaust on rat lung and brain. Arch Toxicol. 2010;84:553–62. https://doi.org/10.1007/s00204-010-0551-7.
Yan W, Ji X, Shi J, Li G, Sang N. Acute nitrogen dioxide inhalation induces mitochondrial dysfunction in rat brain. Environ Res. 2015;138:416–24. https://doi.org/10.1016/j.envres.2015.02.022.
Power MC, Kioumourtzoglou MA, Hart JE, Okereke OI, Laden F, Weisskopf MG. The relation between past exposure to fine particulate air pollution and prevalent anxiety: observational cohort study. BMJ. 2015;350:h1111. https://doi.org/10.1136/bmj.h1111.
Kuo CY, Hsieh CY, Hu CW, Chen SC, Yang HJ. PM10 concentration in relation to clinic visits for anxiety disorders: a population-based study of a high river-dust episode region in Taiwan. Air Qual, Atmosphere Health 2018;11:221–7. https://doi.org/10.1007/s11869-017-0534-4.
Zhou YM, Fan YN, Yao CY, Xu C, Liu XL, Li X, et al. Association between short-term ambient air pollution and outpatient visits of anxiety: A hospital-based study in northwestern China. Environ Res. 2021;197:111071. https://doi.org/10.1016/j.envres.2021.111071.
Borroni E, Pesatori AC, Bollati V, Buoli M, Carugno M. Air pollution exposure and depression: A comprehensive updated systematic review and meta-analysis. Environ Pollut. 2022;292:118245. https://doi.org/10.1016/j.envpol.2021.118245.
Manisalidis I, Stavropoulou E, Stavropoulos A, Bezirtzoglou E. Environmental and Health Impacts of Air Pollution: A Review. Front Public Health. 2020;8:14. https://doi.org/10.3389/fpubh.2020.00014.
Andersen ZJ, de Nazelle A, Mendez MA, Garcia-Aymerich J, Hertel O, Tjønneland A, et al. A study of the combined effects of physical activity and air pollution on mortality in elderly urban residents: the Danish Diet, Cancer, and Health Cohort. Environ Health Perspect. 2015;123:557–63. https://doi.org/10.1289/ehp.1408698.
Jung M, Cho D, Shin K. The Impact of Particulate Matter on Outdoor Activity and Mental Health: A Matching Approach. Int J Environ Res Public Health. 2019;16:2983. https://doi.org/10.3390/ijerph16162983.
Tong L, Li K, Zhou Q. Season, sex and age as modifiers in the association of psychosis morbidity with air pollutants: A rising problem in a Chinese metropolis. Sci Total Environ. 2016;541:928–33. https://doi.org/10.1016/j.scitotenv.2015.09.066.
Shin J, Park JY, Choi J. Long-term exposure to ambient air pollutants and mental health status: A nationwide population-based cross-sectional study. PLoS ONE. 2018;13:e0195607. https://doi.org/10.1371/journal.pone.0195607.
Funding
This research was supported by grants from the Gachon University Gil Medical Center (grant numbers 2019-11) and Research of Korea Centers for Disease Control and Prevention (grant number 2021ER120201). This work was also supported by the National Research Foundation of Korea (NRF) grant funded by the Korean government (MSIT) (NRF-2020R1A2C1007527 and NRF-2021R1A5A2030333). The sponsor of the study was not involved in study design, analysis and interpretation of data; writing of the report; or the decision to submit the study results for publication.
Author information
Authors and Affiliations
Contributions
Conceptualization: JJ, SGK; Data curation: JH; Formal analysis: JH; Funding acquisition: JJ, SGK; Investigation: SEC; Methodology: JH, JMK, SEC; Project administration: JJ, SGK; Resources: SEC; Software: JH, JMK, SEC; Supervision: JH, JMK, SEC, JJ, SGK; Validation: JH, JMK; Visualization: JH; Roles/Writing—original draft: JH, JMK; Writing—review and editing: SEC, JJ, SGK.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
This study was approved by the Institutional Review Board of the Gil Medical Center (GCIRB2020-432). Participant consent was waived by the ethics committee because the data involved routinely collected medical data that was processed anonymously at all stages. The study methods were carried out based on the Declaration of Helsinki.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Hong, J., Kang, J.M., Cho, SE. et al. Significant association between increased risk of emergency department visits for psychiatric disorders and air pollutants in South Korea. J Expo Sci Environ Epidemiol 33, 490–499 (2023). https://doi.org/10.1038/s41370-022-00504-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41370-022-00504-y
Keywords
This article is cited by
-
Wildfires are associated with increased emergency department visits for anxiety disorders in the western United States
Nature Mental Health (2024)
-
Medical experience as an influencing parameter in emergency medical care for psychiatric emergencies: retrospective analysis of a multicenter survey
BMC Emergency Medicine (2023)
-
Ecological correlation between short term exposure to particulate matter and hospitalization for mental disorders in Shijiazhuang, China
Scientific Reports (2023)
-
Environmental toxicant-mediated cardiovascular diseases: an insight into the mechanism and possible preventive strategy
Toxicology and Environmental Health Sciences (2023)