Abstract
The popularity of tattooing has increased significantly over recent years. This has raised concerns about the safety of tattoo inks and their metabolites/degradation products. The photolytic and metabolic degradation of tattoo pigments may result in the formation of toxic compounds, with unforeseen health risks. A systematic literature review was undertaken to determine the current state of knowledge of tattoo pigments’ degradation products when irradiated with sunlight, laser light or metabolised. The review demonstrates that there is a lack of knowledge regarding tattoo pigment degradation/metabolism, with only eleven articles found pertaining to the photolysis of tattoo pigments and two articles on the metabolism of tattoo pigments. The limited research indicates that the photolysis of tattoo pigments could result in many toxic degradation products, including hydrogen cyanide and carcinogenic aromatic amines.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 6 print issues and online access
$259.00 per year
only $43.17 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
Cui Y, Spann AP, Couch LH, Gopee NV, Evans FE, Churchwell MI, et al. Phtodeceomposition of pigment yellow 74, a pigment used in tattoo inks. Photochem Photobio Sci. 2004;80:175–84.
Samadelli M, Melis M, Miccoli M, Vigl EE, Zink AR. Complete mapping of the tattoos of the 5300-year-old tyrolean iceman. J Cult Herit. 2015;16:753–8.
Heywood W, Patrick K, Smith AM, Simpson JM, Pitts MK, Richters J, et al. Who gets tattoos? Demographic and behavioral correlates of ever being tattooed in a representative sample of men and women. Ann Epidemiol. 2012;22:51–6.
Makkai T, McAllister I. Prevalence of tattooing and body piercing in the Australian community. Commun Dis Intell Q Rep. 2001;25:67–72.
Fell A. Tattoos in Australia: perceptions, trends and regrets. NSW, Australia: Mccrindle; 2021. Available from: https://mccrindle.com.au/insights/blog/tattoos-on-the-rise-among-aussies/.
Laumann AE, Derick AJ. Tattoos and body piercings in the United States: a national data set. J Am Acad Dermatol. 2006;55:413–21.
Kluger N, Seité S, Taieb C. The prevalence of tattooing and motivations in five major countries over the world. J Eur Acad Dermatol Venereol. 2019;33:e484–6.
Laux P, Tralau T, Tentschert J, Blume A, Al Dahouk S, Bäumler W, et al. A medical-toxicological view of tattooing. Lancet. 2016;387:395–402.
Bauer EM, De Caro T, Tagliatesta P, Carbone M. Unraveling the real pigment composition of tattoo inks: the case of bi-components phthalocyanine-based greens. Dyes Pigm. 2019;167:225–35.
Engel E, Santarelli F, Vasold R, Maisch T, Ulrich H, Prantl L, et al. Modern tattoos cause high concentrations of hazardous pigments in skin. Contact Derm. 2008;58:228–33.
Council of Europe Committee of Ministers. Resolution Resap(2008)1. 2008. Available from: https://rm.coe.int/16805d3dc4.
New Zealand Ministry of Health. Survey of selected samples of tattoo inks for the presence of heavy metals. Wellington, New Zealand; 2013. Available from: https://www.abc.net.au/cm/lb/5060760/data/nz-survey-of-selected-samples-of-tattoo-inks-for-the-presence-o-data.pdf.
Bicca JF, Duquia RP, Breunig JdA, Souza PRMd, Almeida HLd, Jr. Tattoos on 18-year-old male adolescents-characteristics and associated factors. Bras Dermatol. 2013;88:925–8.
Naga LI, Alster TS. Laser tattoo removal: an update. Am J Clin Dermatol. 2017;18:59–65.
Bernstein EF. Laser treatment of tattoos. Clin Dermatol. 2006;24:43–55.
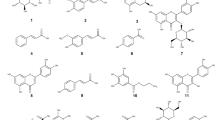
Bäumler W, Eibler ET, Hohenleutner U, Sens B, Sauer J, Landthaler MQ. Switch laser and tattoo pigments: first results of the chemical and photophysical analysis of 41 compounds. Lasers Surg Med. 2000;26:13–21.
Engel E, Spannberger A, Vasold R, König B, Landthaler M, Bäumler W. Photochemical cleavage of a tattoo pigment by Uvb radiation or natural sunlight. J Dtsch Dermatol Ges. 2007;5:583–9.
Gaugler S. Analysis of bioactive compounds in tattoo inks before and after irradiation with sunlight using Hptlc and in situ detection with Vibrio Fischeri. Thesis, University of Hohenheim, Stuttgart; 2011.
Schreiver I, Hutzler C, Laux P, Berlien H-P, Luch A. Formation of highly toxic hydrogen cyanide upon ruby laser irradiation of the tattoo pigment phthalocyanine blue. Sci Rep. 2015;5:12915.
Hering H, Sung AY, Roder N, Hutzler C, Berlien H-P, Laux P. Laser irradiation of organic tattoo pigments releases carcinogens with 3, 3′-dichlorobenzidine inducing DNA strand breaks in human skin cells. J Invest Dermatol. 2018;138:2687–90.
Schreiver I. Tattoo pigments: biodistribution and toxicity of corresponding laser induced decomposition products. Germany, Berlin: Free University of Berlin; 2018.
Pagdin P. Personal communication with Phil Pagdin from The Tattoo Removal Co. concenring tattoo removal processes. 2020.
Howard PC, Sams RL II, Bucher JR, Allaben WT. Phototoxicology and photocarcinogenesis at the USfood and Drug Administrationos National Center for Toxicological Research. J Food Drug Anal. 2002;10:4.
Wezel K. Examination of the behaviour of tattoo inks and pigments under the influence of light. Master thesis, Justus-Liebig University, Gießen, Germany; 2013.
Cui Y, Churchwell MI, Couch LH, Doerge DR, Howard PC. Metabolism of pigment yellow 74 by rat and human microsomal proteins. Drug Metab Dispos. 2005;33:1459–65.
Hauri U, Hohl C. Photostability and breakdown products of pigments currently used in tattoo inks. Curr Probl Dermatol. 2015;48:164–9.
Bauer EM, Scibetta EV, Cecchetti D, Piccirillo S, Antonaroli S, Sennato S, et al. Treatments of a phthalocyanine‑based green ink for tattoo removal purposes: generation of toxic fragments and potentially harmful morphologies. Arch Toxicol. 2020.
Vasold R, Naarmann N, Ulrich H, Fischer D, Könlg B, Landthaler M, et al. Tattoo pigments are cleaved by laser light—the chemical analysis in vitro provide evidence for hazardous compounds. Photochem Photobio Sci. 2004;80:185–90.
Agnello M, Fontana M. Survey on European studies of the chemical characterisation of tattoo ink products and the measurement of potentially harmful ingredients. Tattooed Ski Health. 2015;48:142–51.
Klügl I, Hiller K-A, Landthaler M, Bäumler W. Incidence of health problems associated with tattooed skin: a nation-wide survey in German-speaking countries. J Dermatol. 2010;221:43–50.
Scheme NICNaA. Characterisation of tattoo inks used in Australia. Australia; 2016.
Brady BG, Gold H, Leger EA, Leger MC. Self‐reported adverse tattoo reactions: a New York City Central Park study. Contact Derm. 2015;73:91–9.
Kluger N, Koljonen V. Tattoos, inks, and cancer. Lancet Oncol. 2012;13:e161–8.
Polefka TG, Meyer TA, Agin PP, Bianchini RJ. Effects of solar radiation on the skin. J Cosmet Dermatol. 2012;11:134–43.
Garibyan L, Fisher DE. How sunlight causes melanoma. Curr Oncol Rep. 2010;12:319–26.
ATLAS. Atlas Stability Testing of Cosmetics. AMETEK; 2019. Available from: https://www.atlas-mts.com/applications/applications-overview/cosmetics.
Yengi LG, Xiang Q, Pan J, Scatina J, Kao J, Ball SE, et al. Quantitation of cytochrome P450 Mrna levels in human skin. Anal Biochem. 2003;316:103–10.
Rolsted K, Kissmeyer A-M, Rist GM, Hansen SH. Evaluation of cytochrome P450 activity in vitro, using dermal and hepatic microsomes from four species and two keratinocyte cell lines in culture. Arch Dermatol Res. 2008;300:11–8.
Saeki M, Saito Y, Nagano M, Teshima R, Ozawa S, Sawada J-i. Mrna expression of multiple cytochrome P450 isozymes in four types of cultured skin cells. Int Arch Allergy Immunol. 2002;127:333–6.
Wiegand C, Hewitt NJ, Merk HF, Reisinger K. Dermal xenobiotic metabolism: a comparison between native human skin, four in vitro skin test systems and a liver system. Skin Pharmacol Physiol. 2014;27:263–75.
Luu-The V, Duche D, Ferraris C, Meunier J-R, Leclaire J, Labrie F. Expression profiles of phases 1 and 2 metabolizing enzymes in human skin and the reconstructed skin models Episkin™ and full thickness model from Episkin™. J Steroid Biochem Mol Biol. 2009;116:178–86.
Sepehri M, Sejersen T, Qvortrup K, Lerche CM, Serup J. Tattoo pigments are observed in the Kupffer cells of the liver indicating blood-borne distribution of tattoo ink. J Dermatol. 2017;233:86–93.
Kluger N, Cohen-Valensi R, Nezri M. Black lymph nodes—and a colourful skin. Lancet. 2008;371:1214.
Friedman T, Westreich M, Mozes SN, Dorenbaum A, Herman O. Tattoo pigment in lymph nodes mimicking metastatic malignant melanoma. Plast Reconstr Surg. 2003;111:2120–2.
Honegger MM, Hesseltine SM, Gross JD, Singer C, Cohen J-M. Tattoo pigment mimicking axillary lymph node calcifications on mammography. AJR Am J Roentgenol. 2004;183:831–2.
Lock EA, Reed CJ. Xenobiotic metabolizing enzymes of the kidney. Toxicol Pathol. 1998;26:18–25.
Haehner BD, Gorski JC, Vandenbranden M, Wrighton SA, Janardan SK, Watkins PB, et al. Bimodal distribution of renal cytochrome P450 3a activity in humans. Mol Pharm. 1996;50:52–9.
Park BK, Pirmohamed M, Kitteringham NR. The role of cytochrome P450 enzymes in hepatic and extrahepatic human drug toxicity. Clin Pharm Ther. 1995;68:385–424.
Ding X, Kaminsky LS. Human extrahepatic cytochromes P450: function in xenobiotic metabolism and tissue-selective chemical toxicity in the respiratory and gastrointestinal tracts. Annu Rev Pharm Toxicol. 2003;43:149–73.
Zhao G, Allis JW. Kinetics of bromodichloromethane metabolism by cytochrome P450 isoenzymes in human liver microsomes. Chem Biol Interact. 2002;140:155–68.
Persson KP, Ekehed S, Otter C, Lutz EM, McPheat J, Masimirembwa CM, et al. Evaluation of human liver slices and reporter gene assays as systems for predicting the cytochrome P450 induction potential of drugs in vivo in humans. Pharm Res. 2006;23:56–69.
Chang TK, Chen J, Pillay V, Ho J-Y, Bandiera SM. Real-time polymerase chain reaction analysis of Cyp1b1 gene expression in human liver. Toxicol Sci. 2003;71:11–9.
Global Chemwatch Msds Database—Goldffx [Internet]. 2021. Available from: https://jr.chemwatch.net/chemwatch.web/.
Benzonitrile [Internet]. European Chemicals Agency (ECHA). 2021. Available from: https://echa.europa.eu/brief-profile/-/briefprofile/100.002.596.
ChemWatch. Material safety data sheet: benzonitrile. 2017 [updated Material Safety Data Sheet]. Available from: https://jr.chemwatch.net/chemwatch.web/home.
Bonacker D, Stoiber T, Böhm KJ, Unger E, Degen GH, Thier R, et al. Chromosomal genotoxicity of nitrobenzene and benzonitrile. Arch Toxicol. 2004;78:49–57.
ChemWatch. Material safety data sheet: aniline. 2017 [updated Material Safety Data Sheet]. Available from: https://jr.chemwatch.net/chemwatch.web/home.
Jenkins F, Robinson J, Gellatly J, Salmond G. The no-effect dose of aniline in human subjects and a comparison of aniline toxicity in man and the rat. Food Cosmet Toxicol. 1972;10:671–9.
Agency for Toxic Substances and Disease Registry. Medical management guidelines for aniline Atlanta. Toxicology and Human Health Sciences; 2014. Available from: https://www.atsdr.cdc.gov/MMG/MMG.asp?id=448&tid=79.
Jacobson KH. Acute oral toxicity of mono-and di-alkyl ring-substituted derivatives of aniline. Toxicol Appl Pharm. 1972;22:153–4.
ChemWatch. Material safety data sheet: 3,3’-dichlorobenzidine. 2017 [updated Material Safety Data Sheet]. Available from: https://jr.chemwatch.net/chemwatch.web/home.
Gnomes R, Meek ME. Concise international chemical assessment document 2 3,3’-dichlorobenzidine. Geneva: World Health Organisation; 1998.
Wang L, Yan J, Hardy W, Mosley C, Wang S, Yu H. Light-induced mutagenicity in salmonella Ta102 and genotoxicity/cytotoxicity in human T-cells by 3, 3′-dichlorobenzidine: a chemical used in the manufacture of dyes and pigments and in tattoo inks. J Toxicol. 2005;207:411–8.
Zeilmaker M, Van Kranen H, Van Veen M, Janus J. Cancer risk assessment of azo dyes and aromatic amines from tattoo bands, folders of paper, toys, bed clothes, watch straps and ink. Netherlands; 2000. Available from: https://www.rivm.nl/bibliotheek/rapporten/601503019.html.
Hauri U. Inks for tattoos and permanent make-up—pigments, preservatives, aromatic amines, polyaromatic hydrocarbons and nitrosamines. Basel, Switzerland; 2014. Available from: https://www.kantonslabor.bs.ch/dam/jcr:d12e5456-c71d-4e59-8f29-4a7d8c38d15d/Tattoo_PMU_2014_EN(UK).pdf.
Sabbioni G, Hauri U. Carcinogenic tattoos?. Epidemiol Biostat Public Health. 2016;13:4.
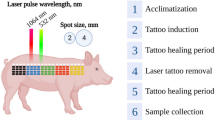
Engel E, Vasold R, Santarelli F, Maisch T, Gopee NV, Howard PC, et al. Tattooing of skin results in transportation and light‐induced decomposition of tattoo pigments—a first quantification in vivo using a mouse model. Exp Dermatol. 2010;19:54–60.
Westland D. Design and apply laser tattoo removal treatments: student learning guide. Australian College of Laser Therapy; 2019.
Poon KW, Dadour IR, McKinley AJ. In situ chemical analysis of modern organic tattooing inks and pigments by micro‐Raman spectroscopy. J Raman Spectrosc. 2008;39:1227–37.
Chen H. Recent advances in azo dye degrading enzyme research. Curr Protein Pept Sci. 2006;7:101–11.
Ortho-Toluidine. Chemical agents and related occupations: IARC monographs on the evaluation of carcinogenic risks to humans, volume 100F. Lyon, France: International Agency for Research on Cancer; 2012. p. 93–9.
European Chemical Agency. 5-Nitro-O-Toluidine. 2021. Available from: https://echa.europa.eu/brief-profile/-/briefprofile/100.002.514.
Acknowledgements
The authors would Like to acknowledge Deborah Westland (CEO of the Australian College of Laser Therapy) for discussing the tattoo laser removal process. The authors would also like to acknowledge Associate Professor Ingo Koeper and Maximillian Mann from Flinders University (Bedford Park, South Australia) for their aid in translating articles written in German. The authors would like to thank the Australian Government Department of Education, Skills and Employment for providing an Australian Research Training Program Scholarship to TRF.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Fraser, T.R., Ross, K.E., Alexander, U. et al. Current knowledge of the degradation products of tattoo pigments by sunlight, laser irradiation and metabolism: a systematic review. J Expo Sci Environ Epidemiol 32, 343–355 (2022). https://doi.org/10.1038/s41370-021-00364-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41370-021-00364-y
This article is cited by
-
Solar photodegradation of irinotecan in water: optimization and robustness studies by experimental design
Photochemical & Photobiological Sciences (2022)