Abstract
Background/objective
This work applied a newly developed low-cost sensing (LCS) device (AS-LUNG-P) and a certified medical LCS device (Rooti RX) to assessing PM2.5 impacts on heart rate variability (HRV) and determining important exposure sources, with less inconvenience to subjects.
Methods
Observations using AS-LUNG-P were corrected by side-by-side comparison with GRIMM instruments. Thirty-six nonsmoking healthy subjects aged 20–65 years were wearing AS-LUNG-P and Rooti RX for 2–4 days in both Summer and Winter in Taiwan.
Results
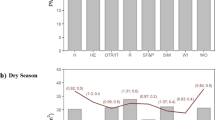
PM2.5 exposures were 12.6 ± 8.9 µg/m3. After adjusting for confounding factors using the general additive mixed model, the standard deviations of all normal to normal intervals reduced by 3.68% (95% confidence level (CI) = 3.06–4.29%) and the ratios of low-frequency power to high-frequency power increased by 3.86% (CI = 2.74–4.99%) for an IQR of 10.7 µg/m3 PM2.5, with impacts lasting for 4.5–5 h. The top three exposure sources were environmental tobacco smoke, incense burning, and cooking, contributing PM2.5 increase of 8.53, 5.85, and 3.52 µg/m3, respectively, during 30-min intervals.
Significance
This is a pioneer in demonstrating application of novel LCS devices to assessing close-to-reality PM2.5 exposure and exposure–health relationships. Significant HRV changes were observed in healthy adults even at low PM2.5 levels.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 6 print issues and online access
$259.00 per year
only $43.17 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
Change history
15 September 2020
An amendment to this paper has been published and can be accessed via a link at the top of the paper.
References
Chen LJ, Ho YH, Lee HC, Wu HC, Liu HM, Hsieh HH, et al. An open framework for participatory PM2.5 monitoring in smart cities. IEEE Access. 2017;5:14441–54.
Wang XW, Liu Z, Zhang T. Flexible sensing electronics for wearable/attachable health monitoring. Small. 2017;13:19.
van Donkelaar A, Martin RV, Brauer M, Boys BL. Use of satellite observations for long-term exposure assessment of global concentrations of fine particulate matter. Environ Health Perspect. 2015;123:135–43.
WHO. Ambient (outdoor) air quality and health. World Health Organization; 2018. http://www.who.int/mediacentre/factsheets/fs313/en/. Accessed 9 Sept 2019.
Brauer M, Freedman G, Frostad J, van Donkelaar A, Martin RV, Dentener F, et al. Ambient air pollution exposure estimation for the global burden of disease 2013. Environ Sci Technol. 2016;50:79–88.
IARC. IARC Scientific Publication No. 161: Air Pollution and Cancer. International Agency for Research on Cancer (IARC), Lyon, France; 2013.
Forouzanfar MH, Afshin A, Alexander LT, Anderson HR, Bhutta ZA, Biryukov S, et al. Global, regional, and national comparative risk assessment of 79 behavioural, environmental and occupational, and metabolic risks or clusters of risks, 1990-2015: a systematic analysis for the global burden of disease study 2015. Lancet. 2016;388:1659–724.
Lelieveld J, Evans JS, Fnais M, Giannadaki D, Pozzer A. The contribution of outdoor air pollution sources to premature mortality on a global scale. Nature. 2015;525:367.
USEPA. Air Quality Criteria for Particulate Matter, United States Environmental Protection Agency, Washington DC, USA; 2004.
Fonken LK, Xu X, Weil ZM, Chen G, Sun Q, Rajagopalan S, et al. Air pollution impairs cognition, provokes depressive-like behaviors and alters hippocampal cytokine expression and morphology. Mol Psychiatry. 2011;16:987–95.
Pope CA, Dockery DW, Spengler JD, Raizenne ME. Respiratory health and PM10 pollution—a daily time-series analysis. Am Rev Respir Dis. 1991;144:668–74.
Volk HE, Lurmann F, Penfold B, Hertz-Picciotto I, McConnell R. Traffic-related air pollution, particulate matter, and autism. JAMA Psychiatry. 2013;70:71–7.
Buteau S, Goldberg MS. A structured review of panel studies used to investigate associations between ambient air pollution and heart rate variability. Environ Res. 2016;148:207–47.
Curtis L, Rea W, Smith-Willis P, Fenyves E, Pan Y. Adverse health effects of outdoor air pollutants. Environ Int. 2006;32:815–30.
Pieters N, Plusquin M, Cox B, Kicinski M, Vangronsveld J, Nawrot TS. An epidemiological appraisal of the association between heart rate variability and particulate air pollution: a meta-analysis. Heart. 2012;98:1127–35.
Trasande L, Thurston GD. The role of air pollution in asthma and other pediatric morbidities. J Allergy Clin Immunol. 2005;115:689–99.
Kleiger RE, Miller JP, Bigger JT, Moss AJ. Decreased heart-rate-variability and its association with increased mortality after acute myocardial-infarction. American J Cardiol. 1987;59:256–62.
Tsuji H, Larson MG, Venditti FJ, Manders ES, Evans JC, Feldman CL, et al. Impact of reduced heart rate variability on risk for cardiac events—the Framingham heart study. Circulation. 1996;94:2850–5.
Jerrett M, Burnet RT, Ma R, Pope CA, Krewski D, Newbold B, et al. Spatial analysis of air pollution and mortality in Los Angeles. Epidemiology. 2006;17:S69.
Pope CA, Burnett RT, Thun MJ, Calle EE, Krewski D, Ito K, et al. Lung cancer, cardiopulmonary mortality, and long-term exposure to fine particulate air pollution. JAMA. 2002;287:1132–41.
Lung SCC, Mao IF, Liu LJS. Residents’ particle exposures in six different communities in Taiwan. Sci Total Environ. 2007;377:81–92.
Tang CS, Wu TY, Chuang KJ, Chang TY, Chuang HC, Lung SCC, et al. Impacts of in-cabin exposure to size-fractionated particulate matters and carbon monoxide on changes in heart rate variability for healthy public transit commuters. Atmosphere. 2019;10:17.
Wu SW, Deng FR, Niu J, Huang QS, Liu YC, Guo XB. Association of heart rate variability in taxi drivers with marked changes in particulate air pollution in Beijing in 2008. Environ Health Perspect. 2010;118:87–91.
Lung SCC, Kao MC. Worshippers’ exposure to particulate matter in two temples in Taiwan. J Air Waste Manage Assoc. 2003;53:130–5.
Brook RD, Rajagopalan S, Pope CA, Brook JR, Bhatnagar A, Diez-Roux AV, et al. Particulate matter air pollution and cardiovascular disease an update to the scientific statement from the American heart association. Circulation. 2010;121:2331–78.
Hamanaka RB, Mutlu GM. Particulate matter air pollution: effects on the cardiovascular system. Front Endocrinol. 2018;9:680.
Barbosa CMG, Terra-Filho M, de Albuquerque ALP, Di Giorgi D, Grupi C, Negrao CE, et al. Burnt sugarcane harvesting–cardiovascular effects on a group of healthy workers, Brazil. PLoS ONE. 2012;7:e46142.
Li H, Cai J, Chen R, Zhao Z, Ying Z, Wang L, et al. Particulate matter exposure and stress hormone levels: a randomized, double-blind, crossover trial of air purification. Circulation. 2017;136:618–27.
Garza JL, Mittleman MA, Zhang JM, Christiani DC, Cavallari JM. Time course of heart rate variability response to PM2.5 exposure from secondhand smoke. Plos ONE. 2016;11:e0154783.
Riediker M, Franc Y, Bochud M, Meier R, Rousson V. Exposure to fine particulate matter leads to rapid heart rate variability changes. Front Environ Sci. 2018;6:2.
Kelly KE, Whitaker J, Petty A, Widmer C, Dybwad A, Sleeth D, et al. Ambient and laboratory evaluation of a low-cost particulate matter sensor. Environ Pollut. 2017;221:491–500.
Lung SCC, Wang WC, Wen TY, Liu CH, Hu SC. A versatile low-cost sensing device for assessing PM2.5 spatiotemporal variation and qualifying source contribution. Sci Total Environ. 2020. https://doi.org/10.1016/j.scitotenv.2020.137145.
Wang WCV, Lung SCC, Liu CH, Wen TYJ, Hu SC, Chen LJ. Evaluation and application of a novel low-cost wearable sensing device in assessing real-time PM2.5 exposure in major Asian transportation modes, submitted to J Expo Sci Environ Epidemiol. 2020, under revision.
Karaoguz MR, Yurtseven E, Asian G, Deliormanli BG, Adiguzel O, Gonen M, et al. The quality of ECG data acquisition, and diagnostic performance of a novel adhesive patch for ambulatory cardiac rhythm monitoring in arrhythmia detection. J Electrocardiol. 2019;54:28–35.
Suh HH, Zanobetti A. Exposure error masks the relationship between traffic-related air pollution and heart rate variability. J Occup Environ Med. 2010;52:685–92.
Adar SD, Gold DR, Coull BA, Schwartz J, Stone PH, Suh H. Focused exposures to airborne traffic particles and heart rate variability in the elderly. Epidemiology. 2007;18:95–103.
Cole-Hunter T, Weichenthal S, Kubesch N, Foraster M, Carrasco-Turigas G, Bouso L, et al. Impact of traffic-related air pollution on acute changes in cardiac autonomic modulation during rest and physical activity: a cross-over study. J Expo Sci Environ Epidemiol. 2016;26:133–40.
Liu WT, Ma CM, Liu IJ, Han BC, Chuang HC, Chuang KJ. Effects of commuting mode on air pollution exposure and cardiovascular health among young adults in Taipei, Taiwan. Int J Hyg Environ Health. 2015;218:319–23.
Shields KN, Cavallari JM, Hunt MJO, Lazo M, Molina M, Molina L, et al. Traffic-related air pollution exposures and changes in heart rate variability in Mexico City: a panel study. Environ Health. 2013;12:7.
Tang CS, Chuang KJ, Chang TY, Chuang HC, Chen LH, Lung SCC, et al. Effects of personal exposures to micro- and nano-particulate matter, black carbon, particle-bound polycyclic aromatic hydrocarbons, and carbon monoxide on heart rate variability in a panel of healthy older subjects. Int J Environ Res Public Health. 2019;16:4672.
Wu SW, Deng FR, Niu J, Huang QS, Liu YC, Guo XB. Exposures to PM2.5 components and heart rate variability in taxi drivers around the Beijing 2008 Olympic games. Sci Total Environ. 2011;409:2478–85.
Lung SCC, Hsiao PK, Wen TY, Liu CH, Fu CB, Cheng YT. Variability of intra-urban exposure to particulate matter and CO from Asian-type community pollution sources. Atmos Environ. 2014;83:6–13.
USEPA. Quality assurance handbook for air pollution measurement systems: “Volume II: ambient air quality monitoring program”. United States Environmental Protection Agency; 2017. https://www3.epa.gov/ttn/amtic/qalist.html. Accessed 9 Sept 2019.
USEPA. Air sensor guidebook. United States Environmental Protection Agency; 2014. https://cfpub.epa.gov/si/si_public_record_report.cfm?Lab=NERL&dirEntryId=277996. Accessed 9 Sept 2019.
Pinter A, Szatmari S, Horvath T, Penzlin AI, Barlinn K, Siepmann M, et al. Cardiac dysautonomia in depression—heart rate variability biofeedback as a potential add-on therapy. Neuropsychiatr Dis Treat. 2019;15:1287–310.
Huffman JC, Celano CM, Januzzi JL. The relationship between depression, anxiety, and cardiovascular outcomes in patients with acute coronary syndromes. Neuropsychiatr Dis Treat. 2010;6:123–36.
Young HA, Benton D. Heart-rate variability: a biomarker to study the influence of nutrition on physiological and psychological health? Behav Pharmacol. 2018;29:140–51.
Dominici F, Peng RD, Barr CD, Bell ML. Protecting human health from air pollution shifting from a single-pollutant to a multipollutant approach. Epidemiology. 2010;21:187–94.
Taiwan EPA. Taiwan air quality monitoring network (English version). Taiwan Environmental Protection Administration; 2020. https://taqm.epa.gov.tw/taqm/en/default.aspx. Accessed 23 Mar 2020.
Acknowledgements
The authors would like to acknowledge the funding support from Academia Sinica under “Establishment of PM2.5 Mobile Sensing Technology (Project No. 022324),” “Integrated Multi-source and High-resolution Heat Wave Vulnerability Assessment of Taiwan (AS-104-SS-A02),” and “Trans-disciplinary PM2.5 Exposure Research in Urban Areas for Health-oriented Preventive Strategies (AS-SS-107-03).” We also appreciate the assistance of those who help during the panel study. The contents of this paper are solely the responsibility of the authors and do not represent the official views of the aforementioned institutes and funding agencies.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Lung, SC.C., Chen, N., Hwang, JS. et al. Panel study using novel sensing devices to assess associations of PM2.5 with heart rate variability and exposure sources. J Expo Sci Environ Epidemiol 30, 937–948 (2020). https://doi.org/10.1038/s41370-020-0254-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41370-020-0254-y
Keywords
This article is cited by
-
Peaks, sources, and immediate health impacts of PM2.5 and PM1 exposure in Indonesia and Taiwan with microsensors
Journal of Exposure Science & Environmental Epidemiology (2024)
-
Detection of impending reflex syncope by means of an integrated multisensor patch-type recorder
Journal of Human Hypertension (2023)
-
Effects of low-frequency noise from wind turbines on heart rate variability in healthy individuals
Scientific Reports (2021)