Abstract
Abnormalities in the central nervous system and renal function are seen together in a variety of congenital syndromes. This Review examines the clinical presentation and the genetic basis of several such syndromes. The X-linked oculocerebrorenal syndrome of Lowe is characterized by developmental delay, blindness, renal tubular dysfunction, and progressive renal failure. This syndrome results from mutations in the OCRL gene, which encodes a phosphatase involved in endosomal trafficking. Mutations in OCRL also occur in Dent disease, which has a milder disease phenotype than Lowe syndrome. Patients with Joubert syndrome have cerebellar ataxia, pigmentary retinopathy, and nephronophthisis. Joubert syndrome is a genetically heterogeneous condition associated with mutations in at least five genes that encode ciliary proteins. Bardet–Biedl syndrome is a clinically variable condition associated with learning disabilities, progressive visual loss, obesity, polydactyly, hypogonadism, and cystic and fibrotic renal changes that can lead to renal failure. Most of the 12 genes mutated in Bardet–Biedl syndrome are also involved in ciliary function, as are the genes implicated in other 'ciliopathies' with similar phenotypes, including Meckel syndrome.
Key Points
-
A number of rare conditions with defined genetic abnormalities are characterized by a set of specific cerebrorenal symptoms including Lowe syndrome, Joubert syndrome, and Bardet–Biedl syndrome
-
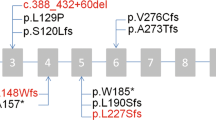
Lowe syndrome is an X-linked disorder that results from mutations in OCRL, a gene that encodes a phosphatase involved in endosomal trafficking
-
Boys with Lowe syndrome have Fanconi-type renal tubular dysfunction and progressive renal failure with developmental delay and blindness
-
Joubert syndrome is a genetically heterogeneous ciliopathy; affected patients can display cerebellar ataxia, pigmentary retinopathy and nephronophthisis
-
Bardet–Biedl syndrome is a clinically variable and genetically heterogeneous ciliopathy; patients can present with cystic and fibrotic renal changes that can lead to renal failure, along with learning disabilities, progressive vision loss, obesity, and hypogonadism
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout





Similar content being viewed by others
References
Lowe, C. U., Terrey, M. & MacLachlan, E. A. Organic-aciduria, decreased renal ammonia production, hydrophthalmos, and mental retardation; a clinical entity. AMA Am. J. Dis. Child. 83, 164–184 (1952).
UK Lowe Syndrome Trust [online], (2009).
Gaary, E. A., Rawnsley, E., Marin-Padilla, J. M., Morse, C. L. & Crow, H. C. In utero detection of fetal cataracts. J. Ultrasound Med. 12, 234–236 (1993).
Lewis, R. A., Nussbaum, R. L. & Brewer, E. D. Lowe Syndrome, GeneReviews [online], (2007).
McSpadden, K., Dolinsky, Z. & Schroerlucke, K. Report on the Lowe's Syndrome Comprehensive Survey. (Lowe Syndrome Association, West Lafayette, 1991).
Walton, D. S., Katsavounidou, G. & Lowe, C. U. Glaucoma with the oculocerebrorenal syndrome of Lowe. J. Glaucoma 14, 181–185 (2005).
Kenworthy, L., Park, T. & Charnas, L. R. Cognitive and behavioral profile of the oculocerebrorenal syndrome of Lowe. Am. J. Med. Genet. 46, 297–303 (1993).
McSpadden, K. Living with Lowe's Syndrome: A Guide for Families, Friends, and Professionals. (ed. Lowe Syndrome Association) (2000).
Bockenhauer, D. et al. Renal phenotype in Lowe Syndrome: a selective proximal tubular dysfunction. Clin. J. Am. Soc. Nephrol. 3, 1430–1436 (2008).
Scheinman, S. J. in Genetic Diseases of the Kidney (eds Lifton, R., Somlo, S., Giebisch, G. & Seldin, D.) 213–226 (Elsevier, New York, 2009).
Kleta, R. Fanconi or not Fanconi? Lowe syndrome revisited. Clin. J. Am. Soc. Nephrol. 3, 1244–1245 (2008).
Laube, G. F., Russell-Eggitt, I. M. & van't Hoff, W. G. Early proximal tubular dysfunction in Lowe's syndrome. Arch. Dis. Child. 89, 479–480 (2004).
Vilasi, A. et al. Combined proteomic and metabonomic studies in three genetic forms of the renal Fanconi syndrome. Am. J. Physiol. Renal Physiol. 293, F456–F467 (2007).
Norden, A. G., Gardner, S. C., van' t Hoff, W. & Unwin, R. J. Lysosomal enzymuria is a feature of hereditary Fanconi syndrome and is related to elevated CI-mannose-6-P-receptor excretion. Nephrol. Dial. Transplant. 23, 2795–2800 (2008).
Charnas, L. R., Bernardini, I., Rader, D., Hoeg, J. M. & Gahl, W. A. Clinical and laboratory findings in the oculocerebrorenal syndrome of Lowe, with special reference to growth and renal function. N. Engl. J. Med. 324, 1318–1325 (1991).
Sliman, G. A., Winters, W. D., Shaw, D. W. & Avner, E. D. Hypercalciuria and nephrocalcinosis in the oculocerebrorenal syndrome. J. Urol. 153, 1244–1246 (1995).
Norden, A. G. et al. Glomerular protein sieving and implications for renal failure in Fanconi syndrome. Kidney Int. 60, 1885–1892 (2001).
Nandedkar, M. A., Minus, H. & Nandedkar, M. A. Eruptive vellus hair cysts in a patient with Lowe syndrome. Pediatr. Dermatol. 21, 54–57 (2004).
Athreya, B. H. et al. Arthropathy of Lowe's (oculocerebrorenal) syndrome. Arthritis Rheum. 26, 728–735 (1983).
Charnas, L. R. & Gahl, W. A. The oculocerebrorenal syndrome of Lowe. Adv. Pediatr. 38, 75–107 (1991).
Attree, O. et al. The Lowe's oculocerebrorenal syndrome gene encodes a protein highly homologous to inositol polyphosphate-5-phosphatase. Nature 358, 239–242 (1992).
Lowe, M. Structure and function of the Lowe syndrome protein OCRL1. Traffic 6, 711–719 (2005).
Choudhury, R. et al. Lowe syndrome protein OCRL1 interacts with clathrin and regulates protein trafficking between endosomes and the trans-Golgi network. Mol. Biol. Cell 16, 3467–3479 (2005).
Jänne, P. A. et al. Functional overlap between murine Inpp5b and Ocrl1 may explain why deficiency of the murine ortholog for OCRL1 does not cause Lowe syndrome in mice. J. Clin. Invest. 101, 2042–2053 (1998).
Erdmann, K. S. et al. A role of the Lowe syndrome protein OCRL in early steps of the endocytic pathway. Dev. Cell 13, 377–390 (2007).
Suchy, S. F. & Nussbaum, R. L. The deficiency of PIP2 5-phosphatase in Lowe syndrome affects actin polymerization. Am. J. Hum. Genet. 71, 1420–1427 (2002).
McCrea, H. J. et al. All known patient mutations in the ASH-RhoGAP domains of OCRL affect targeting and APPL1 binding. Biochem. Biophys. Res. Commun. 369, 493–499 (2008).
Norden, A. G. et al. Urinary megalin deficiency implicates abnormal tubular endocytic function in Fanconi syndrome. J. Am. Soc. Nephrol. 13, 125–133 (2002).
Faucherre, A. et al. Lowe syndrome protein Ocrl1 is translocated to membrane ruffles upon Rac GTPase activation: a new perspective on Lowe syndrome pathophysiology. Hum. Mol. Genet. 14, 1441–1448 (2005).
Shrimpton, A. E. et al. OCRL1 mutations in Dent 2 patients suggest mechanism for phenotypic variability. Nephron Physiology 112, 27–36 (2009).
Utsch, B. et al. Novel OCRL1 mutations in patients with the phenotype of Dent disease. Am. J. Kidney Dis. 48, 942e1–942e14 (2006).
Monnier, N., Satre, V., Lerouge, E., Berthoin, F. & Lunardi, J. OCRL1 mutation analysis in French Lowe syndrome patients: implications for molecular diagnosis strategy and genetic counseling. Hum. Mutat. 16, 157–165 (2000).
Satre, V. et al. Characterization of a germline mosaicism in families with Lowe syndrome, and identification of seven novel mutations in the OCRL1 gene. Am. J. Hum. Genet. 65, 68–76 (1999).
Hildebrandt, F. & Zhou, W. Nephronophthisis-associated ciliopathies. J. Am. Soc. Nephrol. 18, 1855–1871 (2007).
Tobin, J. L. & Beales, P. L. Bardet-Biedl syndrome: beyond the cilium. Pediatr. Nephrol. 22, 926–936 (2007).
Huangfu, D. & Anderson, K. V. Cilia and hedgehog responsiveness in the mouse. Proc. Natl Acad. Sci. USA 102, 11325–11330 (2005).
Liu, A., Wang, B. & Niswander, L. E. Mouse intraflagellar transport proteins regulate both the activator and repressor functions of the Gli transcription factors. Development 132, 3103–3111 (2005).
Nauli, S. M. et al. Pllycystins 1 and 2 mediate mechanosensation in the primary cilium of kidney cells. Nat. Genet. 33, 129–137 (2003).
Gerdes, J. M. et al. Disruption of the basal body compromises proteasomal function and perturbs intracellular Wnt response. Nat. Genet. 39, 1350–1360 (2007).
Simons, M. et al. Inversin, the gene product mutated in nephronophthisis type II, functions as a molecular switch between Wnt signaling pathways. Nat. Genet. 37, 537–543 (2005).
Jho, E. H. et al. Wnt/beta-catenin/Tcf signaling induces the transcription of Axin2, a negative regulator of the signaling pathway. Mol. Cell. Biol. 22, 1172–1183 (2002).
Germino, G. G. Linking cilia to Wnts. Nat. Genet. 37, 455–457 (2005).
Ong, A. C. & Harris, P. C. Molecular pathogenesis of ADPKD: the polycystin complex gets complex. Kidney Int. 67, 1234–1247 (2005).
Mykytyn, K. et al. Bardet–Biedl syndrome type 4 (BBS4)-null mice implicate Bbs4 in flagella formation but not global cilia assembly. Proc. Natl Acad. Sci. USA 101, 8664–8669 (2004).
Tobin, J. L. et al. Inhibition of neural crest migration underlies craniofacial dysmorphology and Hirschsprung's disease in Bardet–Biedl syndrome. Proc. Natl Acad. Sci. USA 105, 6714–6719 (2008).
Valente, E. M., Brancati, F. & Dallapiccola, B. Genotypes and phenotypes of Joubert syndrome and related disorders. Eur. J. Med. Genet. 51, 1–23 (2008).
Parisi, M. A., Doherty, D., Chance, P. F. & Glass, I. A. Joubert syndrome (and related disorders) (OMIM 213300). Eur. J. Hum. Genet. 15, 511–521 (2007).
Maria, B. L., Boltshauser, E., Palmer, S. C. & Tran, T. X. Clinical features and revised diagnostic criteria in Joubert syndrome. J. Child. Neurol. 14, 583–590 (1999).
Raynes, H. R., Shanske, A., Goldberg, S., Burde, R. & Rapin, I. Joubert syndrome: monozygotic twins with discordant phenotypes. J. Child. Neurol. 14, 649–654 (1999).
Steinlin, M., Schmid, M., Landau, K. & Boltshauser, E. Follow-up in children with Joubert syndrome. Neuropediatrics 28, 204–211 (1997).
Braddock, B. A., Farmer, J. E., Deidrick, K. M., Iverson, J. M. & Maria, B. L. Oromotor and communication findings in joubert syndrome: further evidence of multisystem apraxia. J. Child. Neurol. 21, 160–163 (2006).
Haider, N. B., Carmi, R., Shalev, H., Sheffield, V. C. & Landau, D. A Bedouin kindred with infantile nephronophthisis demonstrates linkage to chromosome 9 by homozygosity mapping. Am. J. Hum. Genet. 63, 1404–1410 (1998).
Omran, H. et al. Identification of a new gene locus for adolescent nephronophthisis, on chromosome 3q22 in a large Venezuelan pedigree. Am. J. Hum. Genet. 66, 118–127 (2000).
Gretz, N., Schärer, K., Waldherr, R. & Strauch, M. Rate of deterioration of renal function in juvenile nephronophthisis. Pediatr. Nephrol. 3, 56–60 (1989).
Gleeson, J. G. et al. Molar tooth sign of the midbrain-hindbrain junction: occurrence in multiple distinct syndromes. Am. J. Med. Genet. A 125A, 125–134 (2004).
Harris, P. C. Genetic complexity in Joubert syndrome and related disorders. Kidney Int. 72, 1421–1423 (2007).
Parisi, M. A. et al. AHI1 mutations cause both retinal dystrophy and renal cystic disease in Joubert syndrome. J. Med. Genet. 43, 334–339 (2006).
Valente, E. M. et al. AHI1 gene mutations cause specific forms of Joubert syndrome-related disorders. Ann. Neurol. 59, 527–534 (2006).
Sayer, J. A. et al. The centrosomal protein nephrocystin-6 is mutated in Joubert syndrome and activates transcription factor ATF4. Nat. Genet. 38, 674–681 (2006).
Delous, M. et al. The ciliary gene RPGRIP1L is mutated in cerebello-oculo-renal syndrome (Joubert syndrome type B) and Meckel syndrome. Nat. Genet. 39, 875–881 (2007).
Alexiev, B. A., Lin, X., Sun, C. C. & Brenner, D. S. Meckel–Gruber syndrome: pathologic manifestations, minimal diagnostic criteria, and differential diagnosis. Arch. Pathol. Lab. Med. 130, 1236–1238 (2006).
Ross, A. & Beales, P. L. Bardet–Biedl Syndrome. GeneReviews [online], (2009).
Beales, P. L., Elcioglu, N., Woolf, A. S., Parker, D. & Flinter, F. A. New criteria for improved diagnosis of Bardet–Biedl syndrome: results of a population survey. J. Med. Genet. 36, 437–446 (1999).
Klein, D. & Ammann, F. The syndrome of Laurence–Moon–Bardet–Biedl and allied diseases in Switzerland. Clinical, genetic and epidemiological studies. J. Neurol. Sci. 9, 479–513 (1969).
Grace, C. et al. Energy metabolism in Bardet-Biedl syndrome. Int. J. Obes. Relat. Metab. Disord. 27, 1319–1324 (2003).
Cassart, M., Eurin, D., Didier, F., Guibaud, L. & Avni, E. F. Antenatal renal sonographic anomalies and postnatal follow-up of renal involvement in Bardet–Biedl syndrome. Ultrasound Obstet. Gynecol. 24, 51–54 (2004).
Harnett, J. D. et al. The spectrum of renal disease in Laurence–Moon–Biedl syndrome. N. Engl. J. Med. 319, 615–618 (1988).
Alton, D. J. & McDonald, P. Urographic findings in the Bardet–Biedl syndrome, formerly the Laurence–Moon–Biedl syndrome. Radiology 109, 659–663 (1973).
Rosenbaum, J. L. & Witman, G. B. Intraflagellar transport. Nat. Rev. Mol. Cell Biol. 3, 813–825 (2002).
Nauli, S. M. et al. Polycystins 1 and 2 mediate mechanosensation in the primary cilium of kidney cells. Nat. Genet. 33, 129–137 (2003).
Marshall, W. F. & Nonaka, S. Cilia: tuning in to the cell's antenna. Curr. Biol. 16, R604–R614 (2006).
Karmous-Benailly, H. et al. Antenatal presentation of Bardet–Biedl syndrome may mimic Meckel syndrome. Am. J. Hum. Genet. 76, 493–504 (2005).
Loken, A. C., Hanssen, O., Halvorsen, S. & Jolster, N. J. Hereditary renal dysplasia and blindness. Acta Paediatr. 50, 177–184 (1961).
Caridi, G. et al. Clinical and molecular heterogeneity of juvenile nephronophthisis in Italy: insights from molecular screening. Am. J. Kidney Dis. 35, 44–51 (2000).
Otto, E. A. et al. Nephrocystin-5, a ciliary IQ domain protein, is mutated in Senior–Loken syndrome and interacts with RPGR and calmodulin. Nat. Genet. 37, 282–288 (2005).
Betz, R. et al. Children with ocular motor apraxia type Cogan carry deletions in the gene (NPHP1) for juvenile nephronophthisis. J. Pediatr. 136, 828–831 (2000).
Sargent, M. A., Poskitt, K. J. & Jan, J. E. Congenital ocular motor apraxia: imaging findings. AJNR Am. J. Neuroradiol. 18, 1915–1922 (1997).
Acknowledgements
The authors are grateful to Dr. Thomas welch for helpful comments and to Michele O'Brien for manuscript preparation.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Rights and permissions
About this article
Cite this article
Schurman, S., Scheinman, S. Inherited cerebrorenal syndromes. Nat Rev Nephrol 5, 529–538 (2009). https://doi.org/10.1038/nrneph.2009.124
Issue Date:
DOI: https://doi.org/10.1038/nrneph.2009.124
This article is cited by
-
Transcriptome analysis of neural progenitor cells derived from Lowe syndrome induced pluripotent stem cells: identification of candidate genes for the neurodevelopmental and eye manifestations
Journal of Neurodevelopmental Disorders (2020)
-
Modeling the neuropsychiatric manifestations of Lowe syndrome using induced pluripotent stem cells: defective F-actin polymerization and WAVE-1 expression in neuronal cells
Molecular Autism (2018)
-
Digenic mutations of human OCRL paralogs in Dent’s disease type 2 associated with Chiari I malformation
Human Genome Variation (2016)
-
Craniovertebral junction abnormality in a case of Joubert syndrome
Child's Nervous System (2012)
-
Recognition of the F&H motif by the Lowe syndrome protein OCRL
Nature Structural & Molecular Biology (2011)