Abstract
Objective:
(1) Quantify and compare the family's and the nurse's perception regarding the family's discharge preparedness. (2) Determine which elements contribute to a family's discharge preparedness.
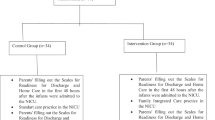
Study Design:
We studied the families of all the infants discharged from a neonatal intensive care unit after a minimum of a 2-week admission. The families rated their overall discharge preparedness with a 9-point Likert scale on the day of discharge. Independently, the discharging nurse evaluated the family's discharge preparedness. Families were considered discharge ‘prepared’ if they rated themselves and the nurse rated their technical and emotional preparedness as ⩾7 on the Likert scale.
Result:
We had 867 (58%) family–nurse pairs who completed the survey. Most families (87%) were prepared for discharge as assessed by the concordant questionnaire (Likert scores of ⩾7 by the parent and the nurse). In multivariate analysis, confidence in their child's health and maturity (odds ratios, OR=2.5 95% confidence interval, CI (1.2, 5.3)), their readiness for their infants to come home (OR=2.9 95% CI (1.0, 8.3)), and selecting a pediatrician (OR=4.2 95% CI (1.6, 11.0)) were statistically significant.
Conclusion:
Assistance with pediatrician selection and home preparation may improve the percentage of families prepared for discharge.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
References
American Academy of Pediatrics Committee on Fetus and Newborn. Hospital discharge of the high-risk neonate. Pediatrics 2008; 122 (5): 1119–1126.
Bernstein HH, Spino C, Baker A, Slora EJ, Touloukian CL, McCormick MC . Postpartum discharge: do varying perceptions of readiness impact health outcomes? Ambul Pediatr 2002; 2 (5): 388–395.
Weiss ME, Ryan P, Lokken L . Validity and reliability of the perceived readiness for discharge after birth scale. J Obstet Gynecol Neonatal Nurs 2006; 35 (1): 34–45.
Lamarche-Vadel A, Blondel B, Truffer P, Burguet A, Cambonie G, Selton D et al. Re-hospitalization in infants younger than 29 weeks’ gestation in the EPIPAGE cohort. Acta Paediatr 2004; 93 (10): 1340–1345.
Resch B, Pasnocht A, Gusenleitner W, Muller W . Rehospitalisations for respiratory disease and respiratory syncytial virus infection in preterm infants of 29–36 weeks gestational age. J Infect 2005; 50 (5): 397–403.
Scherf RF, Reid KW . Going home: what NICU nurses need to know about home care. Neonatal Netw 2006; 25 (6): 421–425.
Sheikh L, O’Brien M, McCluskey-Fawcett K . Parent preparation for the NICU-to-home transition: staff and parent perceptions. Child Health Care 1993; 22 (3): 227–239.
Smith VC, Zupancic JA, McCormick MC, Croen LA, Green J, Escobar GJ et al. Rehospitalization in the first year of life among infants with bronchopulmonary dysplasia. J Pediatr 2004; 144 (6): 799–803.
Behrman R, Butler A (eds). Committee on Understanding Preterm Birth and Assuring Healthy Outcomes Preterm Birth: Causes, Consequences and Prevention. National Academies Press: Washington, DC, 2006.
Hotaling AJ, Zablocki H, Madgy DN . Pediatric tracheotomy discharge teaching: a comprehensive checklist format. Int J Pediatr Otorhinolaryngol 1995; 33 (2): 113–126.
Sullivan M . The new subjective medicine: taking the patient's point of view on health care and health. Soc Sci Med 2003; 56 (7): 1595–1604.
Britton JR, Baker A, Spino C, Bernstein HH . Postpartum discharge preferences of pediatricians: results from a national survey. Pediatrics 2002; 110 (1 Pt 1): 53–60.
American Academy of Pediatrics Committee on Fetus and Newborn. Hospital discharge of the high-risk neonate—proposed guidelines. Pediatrics 1998; 102 (2 Pt 1): 411–417.
Greenland S . Modeling and variable selection in epidemiologic analysis. Am J Public Health 1989; 79 (3): 340–349.
Knaus WA, Wagner DP, Zimmerman JE, Draper EA . Variations in mortality and length of stay in intensive care units. Ann Intern Med 1993; 118 (10): 753–761.
Render ML, Kim HM, Welsh DE, Timmons S, Johnston J, Hui S et al. Automated intensive care unit risk adjustment: results from a National Veterans Affairs study. Crit Care Med 2003; 31 (6): 1638–1646.
Robinson A, Miller M . Making information accessible: developing plain English discharge instructions. J Adv Nurs 1996; 24 (3): 528–535.
Bruder MB, Cole M . Critical elements of transition from NICU to home and follow-up. Child Health Care 1991; 20 (1): 40–49.
Broedsgaard A, Wagner L . How to facilitate parents and their premature infant for the transition home. Int Nurs Rev 2005; 52 (3): 196–203.
Baker K, Kuhlmann T, Magliaro BL . Homeward bound. Discharge teaching for parents of newborns with special needs. Nurs Clin North Am 1989; 24 (3): 655–664.
London F . How to prepare families for discharge in the limited time available. Pediatr Nurs 2004; 30 (3): 212–214, 227.
Titler MG, Pettit DM . Discharge readiness assessment. J Cardiovasc Nurs 1995; 9 (4): 64–74.
Brazy JE, Anderson BM, Becker PT, Becker M . How parents of premature infants gather information and obtain support. Neonatal Netw 2001; 20 (2): 41–48.
Swartz MK . Parenting preterm infants: a meta-synthesis. MCN Am J Matern Child Nurs 2005; 30 (2): 115–120.
Acknowledgements
Funding for the project was from NRSA institutional training grant AHRQ T32 HS 000063 to the Harvard Pediatric Health Services Research Fellowship Program and the Harvard School of Public Health Department of Maternal Child Health Educational training grant MCHP 2T 76MC 00001-47. An early version of the pilot work for this manuscript was presented in abstract and poster form at the Pediatric Academic Societies’ Annual Meeting in San Francisco, California in May 2004. We have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Smith, V., Young, S., Pursley, D. et al. Are families prepared for discharge from the NICU?. J Perinatol 29, 623–629 (2009). https://doi.org/10.1038/jp.2009.58
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/jp.2009.58
Keywords
This article is cited by
-
Predictors of Improvement in Parental Stress After the First Three Months at Home with a Medically Fragile Infant
Maternal and Child Health Journal (2023)
-
The association of care transitions measure-15 score and outcomes after discharge from the NICU
BMC Pediatrics (2021)
-
Evaluating Maternal Discharge Readiness in Kangaroo Mother Care
Indian Pediatrics (2021)
-
The color of health: how racism, segregation, and inequality affect the health and well-being of preterm infants and their families
Pediatric Research (2020)
-
Health literacy of parents of very preterm infants at NICU admission and discharge: a prospective cohort study
Journal of Perinatology (2019)