Abstract
Diseases complicated by abnormal growth of vessels or excessive leakage are the most prevalent cause of moderate or severe vision loss in developed countries. Recent progress unraveling the molecular pathogenesis of several of these disease processes has led to new drug therapies that have provided major benefits to patients. However, those treatments often require frequent intraocular injections, and despite monthly injections, some patients have a suboptimal response. Gene transfer of antiangiogenic proteins is an alternative approach that has the potential to provide long-term suppression of neovascularization (NV) and/or excessive vascular leakage in the eye. Studies in animal models of ocular NV have demonstrated impressive results with a number of transgenes, and a clinical trial in patients with advanced neovascular age-related macular degeneration has provided proof-of-concept. Two ongoing clinical trials, one using an adeno-associated viral (AAV) vector to express a vascular endothelial growth factor-binding protein and another using a lentiviral vector to express endostatin and angiostatin, will provide valuable information that should help to inform future trials and provide a foundation on which to build.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
References
Klein R, Klein BEK, Moss SE, Davis MD, DeMets DL . The Wisconsin Epidemiologic Study of Diabetic Retinopathy. II. Prevalence and risk of diabetic retinopathy when age at diagnosis is less than 30 years. Arch Ophthalmol 1984; 102: 520–526.
Klein R, Klein BE, Linton KL . Prevalence of age-related maculopathy. The Beaver Dam Eye Study. Ophthalmology 1992; 99: 933–943.
Kwak N, Okamoto N, Wood JM, Campochiaro PA . VEGF is an important stimulator in a model of choroidal neovascularization. Invest Ophthalmol Vis Sci 2000; 41: 3158–3164.
Okamoto N, Tobe T, Hackett SF, Ozaki H, Vinores MA, LaRochelle W et al. Transgenic mice with increased expression of vascular endothelial growth factor in the retina: a new model of intraretinal and subretinal neovascularization. Am J Pathol 1997; 151: 281–291.
Yannuzzi LA, Negrao S, Iida T, Carvalho C, Rodriguez-Coleman H, Slakter JS et al. Retinal angiomatous proliferation in age-related macular degeneration. Retina 2001; 21: 416–434.
Oshima Y, Oshima S, Nambu H, Kachi S, Hackett SF, Melia M et al. Increased expression of VEGF in retinal pigmented epithelial cells is not sufficient to cause choroidal neovascularization. J Cell Physiol 2004; 201: 393–400.
Tobe T, Ortega S, Luna JD, Ozaki H, Okamoto N, Derevjanik NL et al. Targeted disruption of the FGF2 gene does not prevent choroidal neovascularization in a murine model. Am J Pathol 1998; 153: 1641–1646.
Yamada H, Yamada E, Kwak N, Ando A, Suzuki A, Esumi N et al. Cell injury unmasks a latent proangiogenic phenotype in mice with increased expression of FGF2 in the retina. J Cell Physiol 2000; 185: 135–142.
Saishin Y, Saishin Y, Takahashi K, Lima Silva R, Hylton D, Rudge J et al. VEGF-TRAPR1R2 suppresses choroidal neovascularization and VEGF-induced breakdown of the blood-retinal barrier. J Cell Physiol 2003; 195: 241–248.
Rosenfeld PJ, Brown DM, Heier JS, Boyer DS, Kaiser PK, Chung CY et al. Ranibizumab for neovascular age-related macular degeneration. N Eng J Med 2006; 355: 1419–1431.
Brown DM, Kaiser PK, Michels M, Soubrane G, Heier JS, Kim RY et al. Ranibizumab versus verteporfin for neovascular age-related macular degeneration. N Eng J Med 2006; 355: 1432–1444.
Ozaki H, Yu A, Della N, Ozaki K, Luna JD, Yamada H et al. Hypoxia inducible factor-1a is increased in ischemic retina: temporal and spatial correlation with VEGF expression. Invest Ophthalmol Vis Sci 1999; 40: 182–189.
Kelly BD, Hackett SF, Hirota K, Oshima Y, Cai Z, Berg-Dixon S et al. Cell type-specific regulation of angiogenic growth factor gene expression and induction of angiogenesis in nonischemic tissue by a constitutively active form of hypoxia-inducible factor 1. Circ Res 2003; 93: 1074–1081.
Oshima Y, Deering T, Oshima S, Nambu H, Reddy PS, Kaleko M et al. Angiopoietin-2 enhances retinal vessel sensitivity to vascular endothelial growth factor. J Cell Physiol 2004; 199: 412–417.
Oshima Y, Oshima S, Nambu H, Kachi S, Takahashi K, Umeda N et al. Different effects of angiopoietin 2 in different vascular beds in the eye; new vessels are most sensitive. FASEB J 2005; 19: 963–965.
Aiello LP, Pierce EA, Foley ED, Takagi H, Chen H, Riddle L et al. Suppression of retinal neovascularization in vivo by inhibition of vascular endothelial growth factor (VEGF) using soluble VEGF-receptor chimeric proteins. Proc Natl Acad Sci USA 1995; 92: 10457–10461.
Seo M-S, Kwak N, Ozaki H, Yamada H, Okamoto N, Fabbro D et al. Dramatic inhibition of retinal and choroidal neovascularization by oral administration of a kinase inhibitor. Am J Pathol 1999; 154: 1743–1753.
Ozaki H, Seo M-S, Ozaki K, Yamada H, Yamada E, Hofmann F et al. Blockade of vascular endothelial cell growth factor receptor signaling is sufficient to completely prevent retinal neovascularization. Am J Pathol 2000; 156: 679–707.
Nguyen QD, Tatlipinar S, Shah SM, Haller JA, Quinlan E, Sung J et al. Vascular endothelial growth factor is a critical stimulus for diabetic macular edema. Am J Ophthalmol 2006; 142: 961–969.
Nguyen QD, Shah SM, Heier JS, Do DV, Lim J, Boyer D et al. Primary End Point (Six Months) Results of the Ranibizumab for Edema of the mAcula in Diabetes (READ-2) Study. Ophthalmology 2009; 116: 2175–2181.
Nguyen QD, Shah SM, Khwaja AA, Channa R, Hatef E, Do DV et al. Two-year outcomes of the Ranibizumab for Edema of the mAcula in Diabetes (READ-2) study. Ophthalmology 2010; 117: 2146–2151.
Network TDRCR. Randomized trial evaluating ranibzumab plus prompt or deferred laser or triamcinolone plus prompt laser for diabetic macular edema. Ophthalmolgy 2010; 117: 1064–1077.
Campochiaro PA, Hafiz G, Shah SM, Nguyen QD, Ying H, Do DV et al. Ranibizumab for macular edema due to retinal vein occlusions; implication of VEGF as a critical stimulator. Mol Ther 2008; 16: 791–799.
Campochiaro PA, Hafiz G, Channa R, Shah SM, Nguyen QD, Ying H et al. Antagonism of vascular endothelial growth factor for macular edema caused by retinal vein occlusion: two-year outcomes. Ophthalmology 2010; 117: 2387–2394.
Campochiaro PA, Heier JS, Feiner L, Gray S, Saroj N, Rundle AC et al. Ranibizumab for macular edema following branch retinal vein occlusion: 6-month primary endpoint results of a phase III study. Ophthalmology 2010; 117: 1102–1112.
Brown DM, Campochiaro PA, Singh RP, Gray S, Rundle AC, Li Z et al. Efficacy and safety of ranibizumab in the treatment of macular edema secondary to central retinal vein occlusion:6-month results of the phase III CRUISE study. Ophthalmology 2010; 117: 1124–1133.
Kendall RL, Wang GL, Thomas KA . Identification of a natural soluble form of the vascular endothelial growth factor receptor, FLT-1, and its heterodimerization with KDR. Biochem Biophys Res Comm 1996; 226: 324–328.
He Y, Smith SK, Day KA, Clark DE, Licence DR, Charnock-Jones DS . Alternative splicing of vascular endothelial growth factor (VEGF)-R1 (FLT-1) pre-mRNA is important for the regulation of VEGF activity. Mol Endocrinol 1999; 13: 537–545.
Tombran-Tink J, Chader GG, Johnson SV . PEDF: a pigment epithelium derived factor with potent neuronal differentiating activity. Exp Eye Res 1991; 53: 411–414.
Dawson DW, Volpert OV, Gillis P, Crawford SE, Xu H-J, Benedict W et al. Pigment epithelium-derived factor: a potent inhibitor of angiogenesis. Science 1999; 285: 245–248.
O’Reilly MS, Holmgren S, Shing Y, Chen C, Rosenthal RA, Moses M et al. Angiostatin: a novel angiogenesis inhibitor that mediates the suppression of metastases by a Lewis lung carcinoma. Cell 1994; 79: 315–328.
O’Reilly MS, Boehm T, Shing Y, Fukai N, Vasios G, Lane WS et al. Endostatin: an endogenous inhibitor of angiogenesis and tumor growth. Cell 1997; 88: 277–285.
Della NG, Campochiaro PA, Zack DJ . Localization of TIMP-3 mRNA expression to the retinal pigment epithelium. Invest Ophthalmol Vis Sci 1996; 37: 1921–1924.
Kamei M, Hollyfield JG . TIMP-3 in Bruch's membrane: changes during aging and in age-related macular degeneration. Invest Ophthalmol Vis Sci 1999; 40: 2367–2375.
Apte SS, Olsen BR, Murphy G . The gene structure of tissue inhibitor of metalloproteinases (TIMP)-3 and its inhibitory activities define the distinct TIMP gene family. J Biol Chem 1995; 270: 14313–14318.
Watanabe K, Hasegawa Y, Yamashita H, Shimizu K, Ding Y, Abe M et al. Vasohibin as an endothelium-derived negative feedback regulator of angiogenesis. J Clin Invest 2004; 114: 898–907.
Steele FR, Chader GJ, Johnson LV, Tombran-Tink J . Pigment epithelium-derived factor: neurotrophic activity and identification as a member or the serine protease inhibitor gene family. Proc Natl Acad Sci USA 1993; 90: 1526–1530.
Araki T, Taniwaki T, Becerra SP, Chader GJ, Schwartz JP . Pigment epithelium-derived factor (PEDF) differentially protects immature but not mature cerebellar granule cells against apoptotic cell death. J Neurosci Res 1998; 53: 7–15.
Bilak MM, Corse AM, Bilak SR, Lehar M, Tombran-Tink J, Kuncl RW . Pigment epithelium-derived factor (PEDF) protects motor neurons from chronic glutamate-mediated neurodegeneration. J Neuropathol Exp Neurol 1999; 58: 719–728.
Cao W, Tombran-Tink J, Elias R, Sezate S, Mrazek D, McGinnis JF . In vivo protection of photoreceptors from light damage by pigment epithelium-derived factor. Invest Ophthalmol Vis Sci 2001; 42: 1642–1652.
Mori K, Duh E, Gehlbach P, Ando A, Takahashi K, Pearlman J et al. Pigment epithelium-derived factor inhibits retinal and choroidal neovascularization. J Cell Physiol 2001; 188: 253–263.
Mori K, Gehlbach P, Ando A, McVey D, Wei L, Campochiaro PA . Regression of ocular neovascularization by increased expression of pigment epithelium-derived factor. Invest Ophthalmol Vis Sci 2001; 43: 2428–2434.
Mori K, Gehlbach P, Yamamoto S, Duh E, Zack DJ, Li Q et al. AAV-mediated gene transfer of pigment epithelium-derived factor inhibits choroidal neovascularization. Invest Ophthalmol Vis Sci 2002; 43: 1994–2000.
Auricchio A, Behling KC, Maguire AM, O’Conner EM, Bennett J, Wilson JM et al. Inhibition of retinal neovascularization by intraocular viral-mediated delivery of anti-angiogenic agents. Mol Ther 2002; 6: 490–494.
Raisler BJ, Berns KI, Grant MB, Beliaev D, Hauswirth WW . Adeno-associated virus type 2 expression of pigmented epithelium-derived factor or Kringles 1-3 of angiostatin reduce retinal neovascularization. Proc Natl Acad Sci USA 2002; 99: 8909–8914.
Gehlbach P, Demetriades AM, Yamamoto S, Deering T, Duh EJ, Yang HS et al. Periocular injection of an adenoviral vector encoding pigment epithelium-derived factor inhibits choroidal neovascularization. Gene Ther 2003; 10: 637–646.
Demetriades AM, Deering T, Liu H, Lu L, Gehlbach P, Packer JD et al. Trans-scleral delivery of antiangiogenic proteins. J Ocul Pharmacol Ther 2008; 24: 70–79.
Saishin Y, Lima Silva R, Saishin Y, Callahan K, Schoch C, Ahlheim M et al. Periocular injection of microspheres containing PKC412 inhibits choroidal neovascularization in a porcine model. Invest Ophthalmol Vis Sci 2003; 44: 4989–4993.
Campochiaro PA, Nguyen QD, Shah SM, Klein ML, Holz E, Frank RN et al. Adenoviral vector-delivered pigment epithelium-derived factor for neovascular age-related macular degeneration: results of a phase I clinical trial. Hum Gene Ther 2006; 17: 167–176.
Honda M, Sakamoto T, Ishibashi T, Inomata H, Ueno H . Experimental subretinal neovascularization is inhibited by adenovirus-mediated soluble VEGF.flt-1 receptor gene transfection: a role of VEGF and possible treatment for SRN in age-related macular degeneration. Gene Ther 2000; 7: 978–985.
Rota R, Riccioni T, Zaccarini M, Lamartina S, Gallo AD, Fusco A et al. Marked inhibition of retinal neovascularization in rats following soluble-flt-1 gene transfer. J Gene Med 2004; 6: 992–1002.
Bainbridge J, Mistry A, Alwis MD, Paleolog E, Baker A, Thrasher AJ et al. Inhibition of retinal neovascularization by gene transfer of soluble VEGF receptor sFlt-1. Gene Ther 2002; 9: 320–326.
Lai CM, Shen WY, Brankov M, Lai YK, Barnett NL, Lee SY et al. Long-term evaluation of AAV-mediated sFlt-1 gene therapy for ocular neovascularization in mice and monkeys. Mol Ther 2005; 12: 659–668.
Lai YK, Shen WY, Brankov M, Lai CM, Constable IJ, Rakoczy PE . Potential long-term inhibition of ocular neovascularization by recombinant adeno-associated virus-mediated secretion gene therapy. Gene Ther 2002; 9: 804–813.
Gehlbach P, Demetriades AM, Yamamoto S, Deering T, Xiao WH, Duh EJ et al. Periocular gene transfer of sFlt-1 suppresses ocular neovascularization and VEGF-induced breakdown of the blood-retinal barrier. Hum Gene Ther 2003; 14: 129–141.
Pechan P, Rubin H, Lukason M, Ardinger J, DuFresne E, Hauswirth WW et al. Novel anti-VEGF chimeric molecules delivered by AAV vectors for inhibition of retinal neovascularization. Gene Ther 2009; 16: 10–16.
Lukason M, Dufresne E, Hillard R, Pechan P, Li Q, Kim I et al. Inhibition of choroidal neovascularization in a nonhuman primate model by intravitreal administration of an AAV2 vector expressin a novel anti-VEGF molecule. Mol Ther 2011; 19: 260–265.
Nishijima K, Ng YS, Zhong L, Bradley J, Schubert W, Jo N et al. Vascular endothelial growth factor-A is a survival factor for retinal neurons and a critical neuroprotectant during the adaptive response to ischemic injury. Am J Pathol 2007; 171: 53–67.
Saint-Geniez M, Raharaj ASR, Walshe TE, Tucker BA, Sekiyama E, Kurihara T et al. Endogenous VEGF is required for visual function: evidence for a survival role on Muller cells and photoreceptors. Plos One 2008; 3: e3554: 3551–3511.
Saint-Geniez M, Kurihara T, Sekiyama E, Maldonado AE, D’Amore PA . An essential role for RPE-derived soluble VEGF in the maintenance of the choriocapillaris. Proc Natl Acad Sci USA 2009; 106: 18751–18756.
Ueno S, Pease ME, Wersinger DMB, Masuda T, Vinores SA, Licht T et al. Prolonged blockade of VEGF family members does not cause identifiable damage to retinal neurons or vessels. J Cell Physiol 2008; 217: 13–22.
Lee S, Chen TT, Barber CL, Jordan MC, Murdock J, Desai S et al. Autocrine VEGF signaling is required for vascular homeostasis. Cell 2007; 130: 691–703.
Miki A, Ueno S, Wesinger DM, Berlinicke C, Shaw GC, Usui S et al. Prolonged blockade of VEGF receptors does not damage retinal photoreceptors or ganglion cells. J Cell Physiol 2010; 224: 262–272.
Maclachian TK, Lukason M, Collins M, Munger R, Isenberger E, Rogers C et al. Preclinical safety evaluation of AAV2-sFLT01-a gene therapy for age-related macular degeneration. Mol Ther 2011; 19: 326–334.
Fukai N, Eklund L, Marneros AG, Oh SP, Keene DR, Tamarkin L et al. Lack of collagen XVIII/endostatin results in eye abnormalities. EMBO J 2002; 21: 1535–1544.
Mori K, Ando A, Gehlbach P, Nesbitt D, Takahashi K, Goldsteen D et al. Inhibition of choroidal neovascularization by intravenous injection of adenoviral vectors expressing secretable endostatin. Am J Pathol 2001; 159: 313–320.
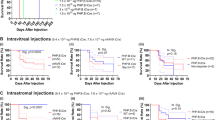
Takahashi K, Saishin Y, Saishin Y, Lima Silva R, Oshima Y, Oshima S et al. Intraocular expression of endostatin reduces VEGF-induced retinal vascular permeability, neovascularization, and retinal detachment. FASEB J 2003; 17: 896–898.
Ohno-Matsui K, Hirose A, Yamamoto S, Saikia J, Okamoto N, Gehlbach P et al. Inducible expression of vascular endothelial growth factor in photoreceptors of adult mice causes severe proliferative retinopathy and retinal detachment. Am J Pathol 2002; 160: 711–719.
Lai C-C, Wu W-C, Chen S-L, Xiao X, Tsai T-C, Huan S-J et al. Suppression of choroidal neovascularization by adeno-associated virus vector expressing angiostatin. Invest Ophthalmol Vis Sci 2001; 42: 2401–2407.
Igarashi T, Miyake K, Kato K, Watanabe A, Ishizaki M, Ohara K et al. Lentivirus-mediated expression of angiostatin efficiently inhibits neovascularization in a murine proliferative retinopathy model. Gene Ther 2003; 10: 219–226.
Balaggan KS, Binley K, Esapa M, MacLaren RE, Iqball S, Duran Y et al. EIAV vector-mediated delivery of endostatin or angiostatin inhibits angiogenesis and vascular hyperpermeability in experimental CNV. Gene Ther 2006; 13: 1153–1165.
Kachi S, Binley K, Yokoi K, Umeda N, Akiyama H, Muramatu D et al. EIAV vector-mediated co-delivery of endostatin and angiostatin driven by the RPE-specific VMD2 promoter inhibits choroidal neovascularization. Hum Gene Ther 2009; 20: 31–39.
Weber BHF, Vogt G, Pruett RC, Stohr H, Felbor U . Mutations in the tissue inhibitor of metalloproteinases-3 (TIMP3) in patients with Sorsby's fundus dystrophy. Nat Genet 1994; 8: 352–356.
Soboleva G, Geis B, Schrewe H, Weber BHF . Sorsby fundus dystrophy mutation Timp3s156C affects the morphological and biochemical phenotype but not metalloproteinase homeostasis. J Cell Physiol 2003; 197: 149–156.
Fariss RN, Apte SS, Suthert PJ, Bird AC, Milam AH . Accumulation of tissue inhibitor of metalloproteinases-3 in human eyes with Sorsby's fundus dystrophy or retinitis pigmentosa. Br J Ophthalmol 1998; 82: 1329–1334.
Takahashi T, Nakamura T, Hayashi A, Kamei M, Nakabayashi M, Okada AA et al. Inhibition of experimental choroidal neovascularization by overexpression of tissue inhibitor of metalloproteinases-3 in retinal pigment epithelium. Am J Ophthalmol 2000; 130: 774–781.
Shimizu K, Watanabe K, Yamashita H, Abe M, Yoshimatsu H, Ohta H et al. Gene regulation of a novel angiogenesis inhibitor, vasohibin, in endothelial cells. Biochem Biophys Res Comm 2005; 327: 700–706.
Shen J, Yang XR, Xiao WH, Hackett SF, Sato Y, Campochiaro PA . Vasohibin is up-regulated by VEGF in the retina and suppresses VEGF receptor 2 and retinal neovascularization. FASEB J 2006; 20: 723–725.
Acknowledgements
This study was supported by grants EY05951, EY12609 and EY10017 from the National Eye Institute and a grant from the Juvenile Diabetes Research Foundation. PAC is the George S and Dolores Dore Eccles Professor of Ophthalmology.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The author declares no conflict of interest.
Rights and permissions
About this article
Cite this article
Campochiaro, P. Gene transfer for ocular neovascularization and macular edema. Gene Ther 19, 121–126 (2012). https://doi.org/10.1038/gt.2011.164
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/gt.2011.164
Keywords
This article is cited by
-
Assessing the long-term evolution of type 3 neovascularization in age-related macular degeneration using optical coherence tomography angiography
Graefe's Archive for Clinical and Experimental Ophthalmology (2021)
-
An Endostatin-lentivirus (ES-LV)-EPC gene therapy agent for suppression of neovascularization in oxygen-induced retinopathy rat model
BMC Molecular and Cell Biology (2020)
-
The role of hypoxia-inducible factors in neovascular age-related macular degeneration: a gene therapy perspective
Cellular and Molecular Life Sciences (2020)
-
Ophthalmic Administration of a DNA Plasmid Harboring the Murine Tph2 Gene: Evidence of Recombinant Tph2-FLAG in Brain Structures
Molecular Biotechnology (2020)
-
Gene Transfer of Prolyl Hydroxylase Domain 2 Inhibits Hypoxia-inducible Angiogenesis in a Model of Choroidal Neovascularization
Scientific Reports (2017)