Abstract
Background/Objectives:
To quantify the rate of progressive failure of very-low-birth-weight (VLBW) infants over time in the neonatal intensive care unit to meet growth milestones.
Subjects/Methods:
In a prospective longitudinal study, 114 VLBW preterm infants (⩽1500 g) of both sexes, with normal and/or low weight for gestational age were included. At the start, weight, length, mid-upper arm (MUAC), thigh and cephalic circumferences were measured. Weight/age (W/A), length/age and weight/length (±2 z-score) indices were calculated. All measurements were taken at inclusion, at 7, 15 and 30 days of hospitalization. Chi-square test, analysis of variance and repeated-measures tests were estimated.
Results:
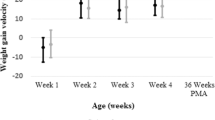
Thirteen cases (14%) died and were excluded soon after the first determinations. In all, 9 (8.9%) died during the study, 12 (11.9%) were discharged before 30 days of life and 80 (79.2%) completed the study. At 7 days, the percentage of preterm infants with an index of W/A <−2 z-scores increased from 44 to 67% (44–68 subjects; P<0.01), with no changes afterwards; the indicator MUAC <−2 z-scores increased at 7 days from 23 to 49% (23–49 subjects); at 15 from 23 to 65% (23–61 subjects) and at 30 days from 23 to 79% (23–63 subjects; P<0.001).
Conclusions:
Clinicians could use these indicators for earlier detection of growth failure in VLBW infants in order to target more aggressive nutrition early.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Adamkin DH (2005). Pragmatic approach to in-hospital nutrition in high-risk neonates. J Perinatol 25, 7–11.
Agostoni C, Buonocore G, Carnielli VP, De Curtis M, Darmaun D, Decsi T et al. (2010). Enteral nutrient supply for preterm infants: Commentary from the European Society for Paediatric Gastroenterology, Hepatology, and Nutrition Committee on Nutrition. J Pediatr Gastroenterol Nutr 50, 85–91.
Avila MC, Sierra T (2006). Factores de riesgo para presentar desnutrición al egreso en los pacientes hospitalizados en las salas de neonatología del Hospital Infantil de México Federico Gómez. Bol Med Hosp Infant Mex 63 (Supl 1), S19 (abstract).
Battaglia FC, Lubchenco LO (1967). A practical classification of newborn infants by weight and gestational age. J Pediatr 71, 159–163.
Benjamin D, Stoll B (2006). Infection in late preterm infants. Clin Perinatol 33, 871–882.
Briassoulis G, Zavras N, Hatzis T (2001). Malnutrition, nutrition indices and early enteral feeding in critically ill children. Nutrition 17, 548–557.
Cárdenas-López C, Haua-Navarro K, Suverza-Fernandez A, Perichart-Perera O (2005). Mediciones antropométricas del neonato. Bol Med Hosp Infant Mex 62, 214–224.
Dogan Y, Erkan T, Yalvac S, Altay S, Culu-Cokugra F, Aydin A et al. (2005). Nutrition status of patients hospitalized in pediatric clinic. Turk J Gastroenterol 16, 212–216.
Embleton NE, Pang N, Cooke RJ (2001). Postnatal malnutrition and growth retardation: an inevitable consequence of current recommendations in preterm infants? Pediatrics 107, 270–273.
Fomon SJ (1977). Nutritional Disorders of Children. US Department of Health, Education and Welfare Bureau of Community Services: Rockville, Maryland, pp 1–66.
Fomon SJ (1993). Nutrition of Normal Infants. Mosby Year Book, Inc.: St Louis, pp 36–84.
Hankard R, Bloch J, Martin P, Randrianasolo H, Bannier M F, Machinot S et al. (2006). Nutritional status and risk in hospitalized children. Arch Pediatr 8, 1203–1208.
Hendricks KM, Duggan C, Gallagher L, Carlin AC, Richardson DS, Collier SB et al. (1995). Malnutrition in hospitalized pediatric patients. Current prevalence. Arch Pediatr Adolesc Med 149, 1118–1122.
Hulst J, Joosten K, Zimmerman L, Hop W, Buuren S, Büller H et al. (2004a). Malnutrition in critically ill children: from admission to 6 months after discharge. Clin Nutr 23, 223–232.
Hulst JM, van Goudoever JB, Zimmermann LJ, Hop WC, Albers MJ, Tibboel D et al. (2004b). The effect of cumulative energy and protein deficiency on anthropometric parameters in a pediatric ICU population. Clin Nutr 23, 1381–1389.
Marino L, Goddard E, Workman L (2006). Determining the prevalence of malnutrition in hospitalized pediatric patients. S Afr Med J 96, 993–995.
Marteletti O, Caldari D, Guimber D, Mention K, Michaud L, Gottrand F (2005). Malnutrition screening in hospitalized children: influence of the hospital unit on its management. Arch Pediatr 12, 1226–1231.
Moreno J, Oliveros L, Pedrón C (2005). Desnutrición hospitalaria en niños. Pediatr Esp 63, 63–69.
Rocha GA, Rocha EJ, Martins CV (2006). The effects of hospitalization on the nutritional status of children. J Pediatr (Rio J) 82, 70–74.
Sasanow SR, Georgieff JK, Pereira GR (1986). Mid-arm circumference and mid-arm/head circumference ratios: standard curves for anthropometric assessment of neonatal nutritional status. J Pediatr 109, 311–315.
Shan HM, Cai W, Sun JH, Cao Y, Shi YY, Fang BH. (2007). Extra uterine growth retardation and correlated factors in premature neonates. Zhonghua Er Ke Za Zhi; 45, 183–188 (abstract).
Usher R, McLean F (1969). Intrauterine growth of live-born Caucasian infants at sea level: standards obtained from measurements in 7 dimensions of infants born between 25 and 44 weeks of gestation. J Pediatr 74, 901–910.
Van Goudoever JB, Sulkers EJ, Lafeber HN, Sauer PJ (2000). Short-term growth and substrate use in very-low-birth-weight infants fed formulas with different energy contents. Am J Clin Nutr 71, 816–821.
Wang DH (2009). Multicenter study of the nutritional status of premature infants in neonatal intensive care unit in China: report of 974 cases. Zhonghua Er Ke Za Zhi 47, 12–17 (abstract).
World Health Organization (1983). Measuring Change in Nutritional Status. Guidelines for Assessing the Nutritional Impact of Supplementary Feeding Programmes for Vulnerable Groups. WHO: Geneva.
Acknowledgements
We thank to Joyce Jackson for her technical assistance and grammatical editing of this document in English. This protocol was supported by the Civil Hospital of Guadalajara and the Institute of Human Nutrition of the University of Guadalajara.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Contributors: YEL-DT participated in the conception and design of the study, acquisition of data, and analysis and interpretation of data; drafting the article, final approval of the version to be submitted; EMV-G participated in the conception and design of the study, analysis and interpretation of data; drafting the article and revising it critically for important intellectual content; AG-O participated in the conception and design of the study, analysis and interpretation of data; JMR-V participated in revising it critically for important intellectual content; RT-S participated in analysis and interpretation of data; GC-F participated in acquisition and analysis of data; all authors read and approved the final manuscript.
Rights and permissions
About this article
Cite this article
Larios-Del Toro, Y., Vásquez-Garibay, E., González-Ojeda, A. et al. A longitudinal evaluation of growth outcomes at hospital discharge of very-low-birth-weight preterm infants. Eur J Clin Nutr 66, 474–480 (2012). https://doi.org/10.1038/ejcn.2011.191
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/ejcn.2011.191