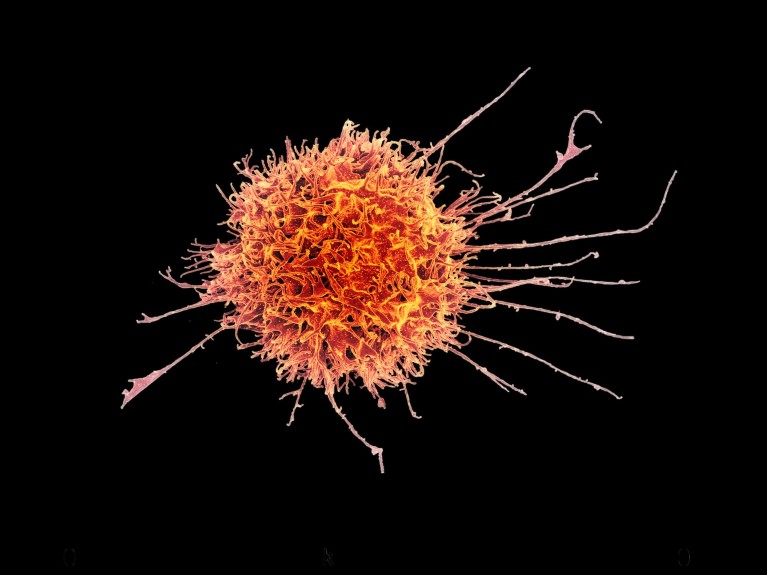
Colourised scanning electron micrograph of a natural killer cell from a human donorCredit: NIAID
Two separate studies, in Kenya and Uganda, have offered clues on how malaria immunity is obtained and how long it lasts. The work reveals for the first time the role of a subset of natural killer cells in naturally acquired immunity.
Previous studies have shown that continual exposure to Plasmodium falciparum, the malaria-causing parasite, provides temporary immunity against the disease, but the precise mechanism that drives this immunity has not been clearly understood.
This has been an area of interest to immunologists since the 1960s when antibodies from people who had become immune to malaria were successfully used to treat malaria patients.
“Scientists have been trying to understand exactly how that happened,” says Faith Osier, co-director of the Institute of Infection, and chair in immunology and vaccinology at the Imperial College, London.
She says scientists have sought to understand: to which parasite proteins do the antibodies bind; and once the antibodies are bound to their targets, how was the parasite infection cleared?
Researchers have focused on neutralising or blocking antibodies that simply stop the parasites from entering the red blood cells, where they multiply and cause disease. “"This blocking activity does not seem to be important when we study blood samples from people who are immune to malaria,” says Osier.
However, two new studies conducted in Kenya and Uganda now offer clues on how the immunity is obtained. The studies, published in Science Translational Medicine, give insights into the role of a subset of cells known as natural killer cells in providing the immunity.
“We reveal for the first time the role of a subset of natural killer cells (CD56 negative NK cells), in naturally acquired immunity against clinical malaria,” explains Isaac Ssewanyana, a research scientist at the Infectious Diseases Research Collaboration (IDRC). He says that they have been able to provide insight into one of the possible mechanisms by which these cells mediate antibody-mediated immunity.
The Uganda study showed that there was a sharp decline in the number of natural killer cells in children following a decline in malaria transmission. What this suggests, according to researchers, is that the natural killer cells rely on repeated exposure to the malaria parasite to maintain their defensive properties.
“These NK cell subsets previously observed in chronic infection rapidly wane in the absence of malaria parasite infection, and therefore, may partly explain the loss of immunity to malaria in the absence of continuous exposure to infection,” observes Ssewanyana, who is also the laboratory director at Central Public Health Laboratories/ National Health Laboratory & Diagnostic Services (NHLDS).
Natural killer cell populations were profiled in 264 children in two Ugandan districts. A distinct group of natural killer cells that lacked the CD56 marker was identified after repeated exposure to malaria.
It was found that children in high-transmission Tororo district had more of these cells than children in Jinja district – a low-transmission area, and that higher number of CD56 natural killer cells corresponded with stronger protection from malaria symptoms and lower parasite loads.
“We found that repeated P. falciparum exposure was associated with the expansion of an atypical population of NK cells that lack expression of the cell marker CD56,” explains Prasanna Jagannathan, assistant professor, Division of Infectious Diseases and Geographic Medicine at Stanford University.
He adds: “In the absence of malaria transmission, CD56 negative cells rapidly decreased, thus suggesting that continuous exposure to P. falciparum is needed to maintain this NK cell subset.”
The Kenyan study arrived at similar conclusions. The natural killer cells were shown to release antimicrobial compounds through a process known as degranulation as well as releasing the inflammatory molecule IFN-y. These molecules helped stop parasites from invading the red blood cells.
The study included both adult and children. The 142 adult volunteers were deliberately infected with malaria and monitored for clinical symptoms. The children had been infected under natural conditions in their places of residence.
“By studying both adults and children, we get a better picture of which parasite proteins and mechanisms are important,” Osier says.
The 293 samples obtained from children living in Junju – a high malaria transmission region on the Kenyan coast – showed the antibody-dependent natural killer cells rose with age and spiked during infection with P. falciparum.
Scientists are hopeful that understanding the factors that drive the programming of the natural killer cells will help guide therapeutic translation, including vaccine-elicited protection.
Osier says that the new study shows that the action of antibodies, working in concert with immune cells – specifically natural killer cells – leads to the destruction of parasites. More importantly however, it helps identify people who are immune to malaria.
“We will go on to identify parasite proteins that lead to this activity. This means that this mechanism can be used to evaluate new vaccines against malaria,” she says.
