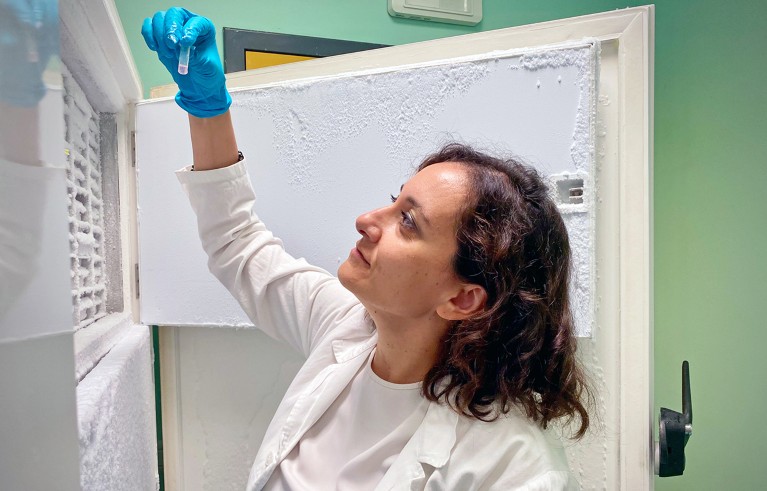
This is a scene from my daily routine in my lab in Milan where we study hematopoietic stem cells, from which all types of blood cells originate. We take these cells from donated umbilical cords, healthy stem cells donors, or leukemia patients. We keep them in vitro, and we modify them to study what happens when they age and are exposed to stress.
Blood stem cells are particularly intriguing. They are more powerful than other adult stem cells, such as muscle or brain ones, because they have a very high turnover, can regenerate quickly and guarantee all different cell lines. Because of this ability to continuously differentiate and self-renew, they must have unique repair and stability mechanisms. But there are many unanswered questions. How do these cells ensure that their DNA remains stable, while doing so many different things? What are their checkpoints, their quality control mechanisms? And are some of their features shared with other stem cell types?
My path to this field was not a straight one. For my PhD at IFOM, also in Milan, I worked on lymphomas, and on how oncogenes break DNA and cause ageing in cells. Then I moved to New York University, where I worked on all types of stem cells, from embryos to adult to cancer. I got interested in how the same mechanisms that preserve the identity of a stem cells become detrimental in cancer, because the same stem cells can evade immune system and resist drugs.
When I came back to Italy, I decided to merge my molecular biology expertise with techniques that are used in clinical settings, in gene therapy, and to focus on blood cells. It was a new field for me, and changing field is quite risky in science. It took some time for the lab to establish itself in the field and begin to publish results. But we were confident that we could answer questions that others were not tackling.
We modify stem cells with viral vectors, CRISPR or other cut-and-paste techniques. We use genomics, imaging, and transplantation into mice to study how they react and understand their biology. This could lead us to improve therapies for tumours, in particular leukemia, or rare diseases.
Gene therapy with techniques such as CRISPR now allows us to take stem cells from patients with blood diseases, correct them and put them back in the patient, avoiding rejection. Some of these therapies made it to the market, but we do not have many data on long-term results. It is possible than in the short term these corrected stem cells successfully repopulate the organism, but in the long term they may age faster than normal, or create an environment that leads again to cancer risk. That’s where we want to contribute. We use experiments to anticipate the long-term effects, and we hope our research can led to “gene therapy 2.0”.
I do this work thanks to an ERC Consolidator grant, and to a similar one from the New York Stem Cell Foundation of which I am particularly proud, because I was the first Italian to get it. My group at SR-Tiget, in Milan, is quite diverse, with cell biologists, computational biologists, and biomedical engineers. They are all Italians, but many of them have come back to Italy after a PhD or a postdoc abroad. I always encourage my PhD students to go abroad for their postdoc. Not because I want them to leave Italy, but because I consider mobility an essential for scientific work. I would like to have more non-Italians in the group, but lower salaries still make it difficult to attract them. Hopefully that can change in the future.