Abstract
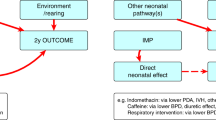
Pharmacologic study is needed in the extremely immature newborns who currently survive. Study is needed of both the drug treatment previously established in more mature neonates and of novel drug therapy. Carefully controlled studies are needed to identify accurately both beneficial and harmful drug therapy and the mechanisms of that toxicity. Careful pharmacologic study of drug disposition and its mechanisms might lead to dosing paradigms or patient selection that minimize toxicity and maximize efficacy. In vivo, translational models of neonatal diseases are limited, but can be used to identify novel treatments and study mechanisms of established, successful therapy. Findings from such studies can generate hypotheses for study in humans leading to a continuing scientific interchange from bedside to bench to bedside. Similarly, clinical observations can generate hypotheses for study in translational models where more invasive analyses are possible. Specific areas of drug treatment should focus on neonatal disorders with long-term, adverse outcomes, such as chronic lung disease, that is amenable to translational study with animal models. National data show a progressive decrease in the clinician-scientist pool entering biomedical research. The future of neonatal pharmacology studies requires an increase in training programs for the physician-scientist whose clinical education in neonatology can be complemented by rigorous basic-science training. Success as a clinician-scientist will require collaboration with full-time basic scientists who can continue studies during periods of clinical work and provide critical study methodology to the overall study design. Such a work environment must be supported by academic institutions and may require more flexibility in the promotion and tenure schedule and process, such as the nature of what it rewards. To complement this, the NIH could modify its grant reporting process to identify co-investigators in studies who may provide unique input to the study concepts and design, such as clinical correlations or clinical investigations.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Vohr BR, Wright LL, Dusick AM, Mele L, Verter J, Steichen JJ et al. Neurodevelopmental and functional outcomes of extremely low birth weight infants in the National Institute of Child Health and Human Development Neonatal Research Network, 1993–1994. Pediatrics 2000; 105: 1216.
Albertine KH, Jones GP, Starcher BC, Bohnsack JF, Davis PL, Cho SC et al. Chronic lung injury in preterm lambs. Disordered respiratory tract development. Am J Respir Crit Care Med 1999; 159: 945.
Ward RM, Beachy JC . Neonatal complications following preterm birth. Br J Obstet Gynec 2003; 110 (Suppl 20): 8.
O'Shea TM, Klinepeter KL, Goldstein DJ, Jackson BW, Dillard RG . Survival and developmental disability in infants with birth weights of 501 to 800 grams, born between 1979 and 1994. Pediatrics 1997; 100: 982.
O'Shea TM, Preisser JS, Klinepeter KL, Dillard RG . Trends in mortality and cerebral palsy in a geographically based cohort of very low birth weight neonates born between 1982 to 1994. Pediatrics 1998; 101: 642.
St John EB, Carlo WA . Respiratory distress syndrome in VLBW infants: changes in management and outcomes observed by the NICHD Neonatal Research Network. Semin Perinatol 2003; 27: 288.
Schreiber MD, Gin-Mestan K, Marks JD, Huo D, Lee G, Srisuparp P . Inhaled nitric oxide in premature infants with the respiratory distress syndrome. N Engl J Med 2003; 349: 2099.
Horbar JD, Stillman AL . Vermont Oxford Network Annual Database Summary for 2000. Vermont Oxford Network: Burlington; 2002.
Ward RM . Pharmacologic principles and practicalities. In: Taeusch HW, Ballard RA (eds). Avery's Diseases of the Newborn. W.B. Saunders: Philadelphia; 1998, pp 404–412.
Ward RM . Adverse effects of drugs in the newborn. In: Rudolph CD RA, Hostetter MK, Lister G, Siegel NJ (eds). Rudolph's Pediatrics. McGraw-Hill: New York; 2003, pp 146–148.
Burns LE, Hodgeman JE, Cass AB . Fatal and circulatory collapse in premature infants receiving chloramphenicol. N Engl J Med 1959; 261: 1318.
Ward RM, Daniel CH, Kendig JW . Oliguria and tolazoline pharmacokinetics in the newborn. Pediatrics 1986; 77: 307.
Lacroix D, Sonnier M, Moncion A, Cheron G, Cresteil T . Expression of CYP3A in the human liver – evidence that the shift between CYP3A7 and CYP3A4 occurs immediately after birth. Eur J Biochem 1997; 247: 625.
Mammel MC, Johnson DE, Green TP, Thompason TR . Controlled trial of dexamethasone therapy in infants with bronchopulmonary dysplasia. Lancet 1983; 1: 1356.
Avery GB, Fletcher AB, Kaplan M, Brudno DS . Controlled trial of dexamethasone in respirator-dependent infants with bronchopulmonary dysplasia. Pediatrics 1985; 75: 106.
Lugo RA, Nahata MC, Menke JA, McClead Jr RE . Pharmacokinetics of dexamethasone in premature neonates. Eur J Clin Pharmacol 1996; 49: 477.
Charles B, Schild P, Steer P, Cartwright D, Donovan T . Pharmacokinetics of dexamethasone following single-dose intravenous administration to extremely low birth weight infants. Dev Pharmacol Ther 1993; 20: 205.
Stark AR, Carlo WA, Tyson JE, Papile LA, Wright LL, Shankaran S et al. Adverse effects of early dexamethasone in extremely-low-birth-weight infants. National Institute of Child Health and Human Development Neonatal Research Network. N Engl J Med 2001; 344: 95.
Shinwell ES, Karplus M, Reich D, Weintraub Z, Blazer S, Bader D et al. Early postnatal dexamethasone treatment and increased incidence of cerebral palsy. Arch Dis Child Fetal Neonatal Ed 2000; 83: F177.
Yeh TF, Lin YJ, Lin HC, Huang CC, Hsieh WS, Lin CH et al. Outcomes at school age after postnatal dexamethasone therapy for lung disease of prematurity. N Engl J Med 2004; 350: 1304.
Romagnoli C, Zecca E, Luciano R, Torrioli G, Tortorolo G . A three year follow up of preterm infants after moderately early treatment with dexamethasone. Arch Dis Child Fetal Neonatal Ed 2002; 87: F55.
Canlon B, Erichsen S, Nemlander E, Chen M, Hossain A, Celsi G et al. Alterations in the intrauterine environment by glucocorticoids modifies the developmental programme of the auditory system. Eur J Neurosci 2003; 17: 2035.
Ikeda T, Mishima K, Yoshikawa T, Iwasaki K, Fujiwara M, Xia YX et al. Dexamethasone prevents long-lasting learning impairment following neonatal hypoxic-ischemic brain insult in rats. Behav Brain Res 2002; 136: 161.
Young TE, Kruyer LS, Marshall DD, Bose CL . Population-based study of chronic lung disease in very low birth weight infants in North Carolina in 1994 with comparisons with 1984. The North Carolina Neonatologists Association. Pediatrics 1999; 104: e17.
Van Marter LJ, Allred EN, Pagano M, Sanocka U, Parad R, Moore M et al. Do clinical markers of barotrauma and oxygen toxicity explain interhospital variation in rates of chronic lung disease? The Neonatology Committee for the Developmental Network. Pediatrics 2000; 105: 1194.
Bland RD, Albertine KH, Carlton DP, Kullama L, Davis P, Cho SC et al. Chronic lung injury in preterm lambs: abnormalities of the pulmonary circulation and lung fluid balance. Pediatr Res 2000; 48: 64.
Bland RD, Ling CY, Albertine KH, Carlton DP, MacRitchie AJ, Day RW et al. Pulmonary vascular dysfunction in preterm lambs with chronic lung disease. Am J Physiol Lung Cell Mol Physiol 2003; 285: L76.
Thomson MA, Yoder BA, Winter VT, Martin H, Catland D, Siler-Khodr TM et al. Treatment of immature baboons for 28 days with early nasal continuous positive airway pressure. Am J Respir Crit Care Med 2004; 169: 1054.
Darlow BA, Graham PJ . Vitamin A supplementation for preventing morbidity and mortality in very low birthweight infants. Cochrane Database Syst Rev 2002 CD000501.
OBrien EA, Zhao L, Dahl MJ, McKnight RA, Reyburn B, Callaway CW et al. NCPAP and vitamin A treatment increase pulmonary TGF-b and SMAD mRNA levels in premature sheep. Pediatr Res 2004; 55: 507A.
OBrien EA, Zhao L, McKnight RA, Dahl MJ, Callaway CW, Reyburn B et al. NCPAP and vitamin A treatment increase pulmonary c-myc and c-jun mRNA levels in the premature sheep. Pediatr Res 2004; 55: 507A.
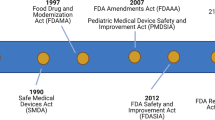
Grinder D, Ward RM . Public meeting on the FDA's proposed regulation requiring manufacturers to assess the safety and effectiveness of new drugs and biological products in pediatric patients. J Pediatr Pharm Pract 1997; 2: 331.
Ward RM . Children, drugs, and the Food and Drug Administration: studies of pediatric drugs are beginning to catch up. Pediatr Ann 2001; 30: 189.
Leeder JS, Kearns GL . Pharmacogenetics in pediatrics. Implications for practice. Pediatr Clin North Am 1997; 44: 55.
Acknowledgements
This study was supported in part by Grant NICHD PPRU 1 U10 HD045986-01 to RM Ward Grant R01 HD41075 to RH Lane; and Children's Health Research Center Grants R01 HL62875, P50 HL5640, and T35 HL07744 to KH Albertine
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ward, R., Lane, R. & Albertine, K. Basic and translational research in neonatal pharmacology. J Perinatol 26 (Suppl 2), S8–S12 (2006). https://doi.org/10.1038/sj.jp.7211423
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.jp.7211423
Keywords
This article is cited by
-
Fewer infants than older patients in paediatric randomised controlled trials
European Journal of Epidemiology (2010)