Abstract
INTRODUCTION: Arterial blood gases are essential in the management of critically ill neonates. A new technology using the Neotrend system (Diametrics Medical) allows for continuous measurement of pH, PaCO2, and PaO2, and calculates oxygen saturation, bicarbonate, and base excess.
OBJECTIVE: To evaluate and compare the results of continuous blood gas measurement using the Neotrend system with a standard system of blood gas analysis in our intensive care unit.
DESIGN: Prospective, controlled, interventional study.
SETTING: The neonatal intensive care unit of a tertiary referral center.
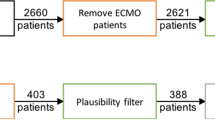
PATIENTS: Neonates with respiratory distress who required respiratory support and frequent arterial blood gas sampling and had a UAC.
RESEARCH DESIGN AND METHOD: To enable Neotrend sensor access to an existing Argyle umbilical artery catheter (UAC) the catheter was cut at the 25-cm mark and connected to an 18-gauge blunt needle luer stub adaptor (Vygon 95440). The study began with the insertion of the Neotrend sensor. Subjects remained on the study until the UAC was discontinued and/or frequent blood gases were no longer needed. The blood gas results from the Neotrend system were not used in clinical management of the patient.
BLOOD GAS MEASUREMENT: During the study period, with each blood sample drawn for laboratory analysis, a printout from the Neotrend monitor was recorded for comparison.
RESULTS: A total of 217 pairs of blood gas samples were collected from seven neonates. The mean bias/precision for pH was 0.01/0.04; for PaO2 0.72/18.5 mm Hg; and for PaCO2 3.96/2.63 mm Hg. The correlation (r value) between the sensor reading and the blood gases were 0.85 for pH, 0.96 for PaO2, and 0.92 for PaCO2.
CONCLUSION: The blood gases compared in the two methods had a strong correlation for pH, PaCO2, PaO2, and oxygen saturation. Although the bicarbonate and base excess values showed suboptimal statistical correlation, the difference was not clinically relevant. Results of this study indicate that this technology provides an accurate means of monitoring continuous blood gas parameters in neonatal patients. It also allows reduced healthcare provider exposure to blood and decreased patient iatrogenic blood loss.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Shapiro BA, Mahutte CK, Cane RD, Gilmour IJ . Clinical performance of a blood gas monitor: a prospective, multicenter trial Crit Care Med 1993; 21: 487–94
Hallor M, Kilger E, Briegel J, Frost H, Peter K . Continuous intra-arterial blood gas and pH monitoring in critically ill patients with severe respiratoryfailure: a prospective, criterion standard study Crit Care Med 1994; 22: 580–6
Venkatesh B, Clutton-Brock TH, Hendry SP . A multiparameter sensor for continuous intra-arterial blood gas monitoring: a prospective evaluation Crit Care Med 1994; 22: 588–94
Venkatesh B, Clutton-Brock TH, Hendry SP . Continuous measurement of blood gases using a combined electrochemical and spectophotometric sensor J Med Eng Technol 1994; 18: 165–8
Weiss IK, Fink S, Harrison R, Feldman JD, Brill JE . Clinical use of continuous arterial blood gas monitoring in the pediatric intensive care unit Pediatrics 1999; 103: 440–5
Morgan C, Dear PR, Newell SJ . Effect of changes in oscillatory amplitude on PaCO2 and PaO2 during high-frequency oscillatory ventilation Arch Dis Child Fetal Neonat Ed 2000; 82: F237–42
Morgan C, Newell SJ, Ducker DA et al. Continuous neonatal blood gas monitoring using a multiparameter intra-arterial sensor Arch Dis Child Fetal Neonat Ed 1999; 80: F93–8
Bland JM, Altman DG . Statistical methods for assessing agreement between two methods of clinical measurement Lancet 1986; 1: 307–10
Zimmerman JE, Seneff MG, Sun X, Wagner DP, Knaus WA . Evaluating laboratory usage in the intensive care unit: patient and institutional characteristics that influence frequency of blood sampling Crit Care Med 1997; 25: 737–48
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Rais-Bahrami, K., Rivera, O., Mikesell, G. et al. Continuous Blood Gas Monitoring Using an In-Dwelling Optode Method: Clinical Evaluation of the Neotrend Sensor Using a Luer Stub Adaptor to Access the Umbilical Artery Catheter. J Perinatol 22, 367–369 (2002). https://doi.org/10.1038/sj.jp.7210735
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.jp.7210735
This article is cited by
-
Bioengineering aspects of sensors and instruments for continuous monitoring of a ventilated newborn
International Journal of Precision Engineering and Manufacturing (2009)