Abstract
Data sources
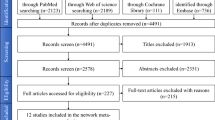
The Cochrane Oral Health Group's Trials Register, Cochrane Central Register of Controlled Trials, Medline and Embase were searched. Handsearching included several dental journals. Authors of all identified trials, an internet discussion group and 55 dental implant manufacturers were contacted to find unpublished randomised controlled trials (RCT).
Study selection
RCT were selected of root-form osseo-integrated oral implants that had a followup of 6 months–1 year and which compared the same osseo-integrated root-form implants immediately (within 1 week), early (1 week–2 months) and conventionally loaded (after 2 months), giving the following outcome measures: failures, implant failures and marginal bone levels on intra-oral radiographs.
Data extraction and synthesis
Data were independently extracted, in duplicate, by two review authors. Authors were contacted for details of randomisation and withdrawals and a quality assessment was carried out. The Cochrane Oral Health Group's statistical guidelines were followed.
Results
Twenty RCT were identified and 11 trials comprising a total of 300 patients were included. Six trials compared immediate versus conventional loading, three early versus conventional loading and two immediate versus early loading. On a patient, rather than per implant basis, there were no statistically significant differences for any of the meta-analyses.
Conclusions
It is possible to successfully load dental implants immediately or early after their placement in selected patients, but not all clinicians achieve optimal results when loading the implant immediately. A high degree of primary implant stability (high value of insertion torque) seems to be one of the prerequisites for a successful immediate/ early loading procedure. More well-designed RCT are needed. Priority should be given to trials comparing immediately versus early loaded implants to improve patient satisfaction and decrease treatment time and trials should be reported according to the CONSORT guidelines (http://www.consort-statement.org/).
Similar content being viewed by others
Commentary
To date, there has been limited systematic comparison of the effect of the timing of implant loading on failure rates. Experience and anecdotal opinions favour a conventional approach to implant loading, but currently it seems popular to attempt to complete treatment in the shortest period of time: immediate and early loading have therefore been suggested. The authors of this article deserve credit for investigating such a contentious aspect of implantology.
Rigorous searching resulted in 20 RCT being identified, of which 11 were eventually included. Both published and unpublished literature have been looked at in this review, with regard to the clinical performance of implants loaded at different times and with a followup of up to 1 year after loading. Although the chosen timeframe is appropriate for short-term complications, we are unable to use this review to comment on long-term complications; for example, patient factors such as change in oral hygiene and parafunctional habits need careful consideration.
Two review authors were involved in the data collection process and a third review author was involved if differences occurred. All authors were contacted for missing information and clarification of information.
The outcome measures used were described as prosthesis failure, implant failure and marginal bone levels on intra-oral radiographs but the definition of failure was varied. It should be noted that the statistical unit was the patient and not the implant. The trials involving patients at high risk of implant failure were excluded (smokers, bone grafted areas, irradiated bone, systemic disease, type IV bone, previous history of implant failure and those in whom primary stability of implants were not satisfactory).
In total, 790 implants in 300 patients were included: 253 were immediately loaded (64 maxillary); 230 were early loaded (132 maxillary); and 307 were conventionally loaded (90 maxillary). At the 1-year review, six of the immediately loaded implants failed, eight of the early loaded ones failed, and six of the conventionally loaded ones failed. The results showed no evidence of heterogeneity and clearly illustrated that there is no statistical significance between failure rates at different times of loading. Numerous failures occurred in certain studies and not in others, however.
We agree with the authors' conclusion that it is possible to successfully load implants immediately or early after implant placement, but that not all clinicians achieve optimal results. Case selection and the degree of primary implant stability was a primary requisite for success.
Author information
Authors and Affiliations
Additional information
Address for correspondence: Luisa Fernandez, Oral Health Group Co-ordinator, MANDEC, 3rd Floor Dental Hospital, University of Manchester, Higher Cambridge Street, Manchester M15 6FH, UK. E-mail: luisa.fernandez@manchester.ac.uk
Esposito M, Grusovin MG, Willings M, Coulthard P, Worthington HV. Interventions for replacing missing teeth: different times for loading dental implants. Cochrane Database Syst Rev 2007; issue 2
Rights and permissions
About this article
Cite this article
Eliyas, S., Al-Khayatt, A. No difference between failure rates of early and conventionally loaded implants. Evid Based Dent 9, 50 (2008). https://doi.org/10.1038/sj.ebd.6400583
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.ebd.6400583
This article is cited by
-
Correlation between resonance frequency, insertion torque and bone-implant contact in self-cutting threaded implants
Odontology (2017)
-
A randomized, 12-month controlled trial to evaluate non-inferiority of early compared to conventional loading of modSLA implants in single tooth gaps
International Journal of Implant Dentistry (2016)