Abstract
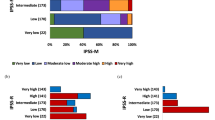
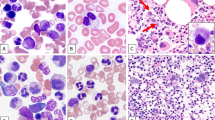
The differences in clinical features and prognosis between hypoplastic myelodysplastic syndrome (h-MDS) and normo-/hypercellular MDS (NH-MDS) remain unsettled. In this study, the characteristics of 37 h-MDS patients and 152 NH-MDS patients were compared. Peripheral-blood white blood cell counts and bone marrow blast percentage were lower in h-MDS patients than in NH-MDS patients (P=0.012 and 0.016, respectively). Refractory anemia (RA) was predominant (56.8%) in h-MDS, whereas RA with excess of blast (RAEB) was most common (44.7%) in NH-MDS. Chromosomal abnormalities −7/7q− occurred less frequently in h-MDS patients than in NH-MDS patients (0 vs 18.3%, P=0.022). There was no significant difference in the prevalence of mutations of RAS, AML1, JAK2, PTPN11, FLT3/ITD, and hypermethylation of SOCS1 and SHP1 between these two groups. International Prognostic Scoring System (IPSS) was ideal for predicting prognoses in h-MDS patients (P=0.002). In low- or intermediate-1 (Int-1)-risk MDS patients, h-MDS patients had a superior survival than NH-MDS patients (P=0.01). In conclusion, distinct from NH-MDS, h-MDS patients have different patterns of hemogram, distribution of French–American–British subtypes, cytogenetic changes and prognoses. IPSS is applicable in h-MDS as in NH-MDS. In patients with low- or Int-1-risk MDS, h-MDS patients have a better prognosis than NH-MDS patients.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
Barrett J, Saunthararajah Y, Molldrem J . Myelodysplastic syndrome and aplastic anemia: distinct entities or diseases linked by a common pathophysiology? Semin Hematol 2000; 37: 15–29.
Nand S, Godwin JE . Hypoplastic myelodysplastic syndrome. Cancer 1988; 62: 958–964.
Chen B, Zhao WL, Jin J, Xue YQ, Cheng X, Chen XT et al. Clinical and cytogenetic features of 508 Chinese patients with myelodysplastic syndrome and comparison with those in Western countries. Leukemia 2005; 19: 767–775.
Lee JH, Lee JH, Shin YR, Lee JS, Kim WK, Chi HS et al. Application of different prognostic scoring systems and comparison of the FAB and WHO classifications in Korean patients with myelodysplastic syndrome. Leukemia 2003; 17: 305–313.
Greenberg PL . Apoptosis and its role in the myelodysplastic syndromes: implications for disease natural history and treatment. Leuk Res 1998; 22: 1123–1136.
Tien HF, Tang JH, Tsay W, Liu MC, Lee FY, Wang CH et al. Methylation of the p15(INK4B) gene in myelodysplastic syndrome: it can be detected early at diagnosis or during disease progression and is highly associated with leukaemic transformation. Br J Haematol 2001; 112: 148–154.
Wu SJ, Yao M, Chou WC, Tang JL, Chen CY, Ko BS et al. Clinical implications of SOCS1 methylation in myelodysplastic syndrome. Br J Haematol 2006; 135: 317–323.
Backx B, Broeders L, Touw I, Lowenberg B . Blast colony-forming cells in myelodysplastic syndrome: decreased potential to generate erythroid precursors. Leukemia 1993; 7: 75–79.
Kook H, Zeng W, Guibin C, Kirby M, Young NS, Maciejewski JP . Increased cytotoxic T cells with effector phenotype in aplastic anemia and myelodysplasia. Exp Hematol 2001; 29: 1270–1277.
Nakao M, Horiike S, Fukushima-Nakase Y, Nishimura M, Fujita Y, Taniwaki M et al. Novel loss-of-function mutations of the haematopoiesis-related transcription factor, acute myeloid leukaemia 1/runt-related transcription factor 1, detected in acute myeloblastic leukaemia and myelodysplastic syndrome. Br J Haematol 2004; 125: 709–719.
Georgiou G, Karali V, Zouvelou C, Kyriakou E, Dimou M, Chrisochoou S et al. Serial determination of FLT3 mutations in myelodysplastic syndrome patients at diagnosis, follow up or acute myeloid leukaemia transformation: incidence and their prognostic significance. Br J Haematol 2006; 134: 302–306.
Paquette RL, Landaw EM, Pierre RV, Kahan J, Lubbert M, Lazcano O et al. N-ras mutations are associated with poor prognosis and increased risk of leukemia in myelodysplastic syndrome. Blood 1993; 82: 590–599.
Tien HF, Wang CH, Chuang SM, Chow JM, Lee FY, Liu MC et al. Cytogenetic studies, ras mutation, and clinical characteristics in primary myelodysplastic syndrome. A study on 68 Chinese patients in Taiwan. Cancer Genet Cytogenet 1994; 74: 40–49.
Greenberg P, Cox C, LeBeau MM, Fenaux P, Morel P, Sanz G et al. International scoring system for evaluating prognosis in myelodysplastic syndromes. Blood 1997; 89: 2079–2088.
Bennett JM, Catovsky D, Daniel MT, Flandrin G, Galton DA, Gralnick HR et al. Proposals for the classification of the myelodysplastic syndromes. Br J Haematol 1982; 51: 189–199.
Tien HF, Wang CH, Chen YC, Shen MC, Lin DT, Lin KH . Characterization of acute myeloid leukemia (AML) coexpressing lymphoid markers: different biologic features between T-cell antigen positive and B-cell antigen positive AML. Leukemia 1993; 7: 688–695.
Maschek H, Kaloutsi V, Rodriguez-Kaiser M, Werner M, Choritz H, Mainzer K et al. Hypoplastic myelodysplastic syndrome: incidence, morphology, cytogenetics, and prognosis. Ann Hematol 1993; 66: 117–122.
Tuzuner N, Cox C, Rowe JM, Bennett JM . Bone marrow cellularity in myeloid stem cell disorders: impact of age correction. Leuk Res 1994; 18: 559–564.
Brodsky RA, Jones RJ . Aplastic anaemia. Lancet 2005; 365: 1647–1656.
Chou WC, Tang JL, Lin LI, Yao M, Tsay W, Chen CY et al. Nucleophosmin mutations in de novo acute myeloid leukemia: the age-dependent incidences and the stability during disease evolution. Cancer Res 2006; 66: 3310–3316.
Harada H, Harada Y, Niimi H, Kyo T, Kimura A, Inaba T . High incidence of somatic mutations in the AML1/RUNX1 gene in myelodysplastic syndrome and low blast percentage myeloid leukemia with myelodysplasia. Blood 2004; 103: 2316–2324.
Lin LI, Chen CY, Lin DT, Tsay W, Tang JL, Yeh YC et al. Characterization of CEBPA mutations in acute myeloid leukemia: most patients with CEBPA mutations have biallelic mutations and show a distinct immunophenotype of the leukemic cells. Clin Cancer Res 2005; 11: 1372–1379.
Shih LY, Huang CF, Wu JH, Lin TL, Dunn P, Wang PN et al. Internal tandem duplication of FLT3 in relapsed acute myeloid leukemia: a comparative analysis of bone marrow samples from 108 adult patients at diagnosis and relapse. Blood 2002; 100: 2387–2392.
Chen CY, Lin LI, Tang JL, Tsay W, Chang HH, Yeh YC et al. Acquisition of JAK2, PTPN11, and RAS mutations during disease progression in primary myelodysplastic syndrome. Leukemia 2006; 20: 1155–1158.
Goemans BF, Zwaan CM, Miller M, Zimmermann M, Harlow A, Meshinchi S et al. Mutations in KIT and RAS are frequent events in pediatric core-binding factor acute myeloid leukemia. Leukemia 2005; 19: 1536–1542.
Chen CY, Tsay W, Tang JL, Shen HL, Lin SW, Huang SY et al. SOCS1 methylation in patients with newly diagnosed acute myeloid leukemia. Genes Chromosomes Cancer 2003; 37: 300–305.
Oka T, Ouchida M, Koyama M, Ogama Y, Takada S, Nakatani Y et al. Gene silencing of the tyrosine phosphatase SHP1 gene by aberrant methylation in leukemias/lymphomas. Cancer Res 2002; 62: 6390–6394.
Bartl R, Frisch B, Baumgart R . Morphologic classification of the myelodysplastic syndromes (MDS): combined utilization of bone marrow aspirates and trephine biopsies. Leuk Res 1992; 16: 15–33.
Delacretaz F, Schmidt PM, Piguet D, Bachmann F, Costa J . Histopathology of myelodysplastic syndromes. The FAB classification (proposals) applied to bone marrow biopsy. Am J Clin Pathol 1987; 87: 180–186.
Kitagawa M, Kamiyama R, Takemura T, Kasuga T . Bone marrow analysis of the myelodysplastic syndromes: histological and immunohistochemical features related to the evolution of overt leukemia. Virchows Arch B Cell Pathol Incl Mol Pathol 1989; 57: 47–53.
Lambertenghi-Deliliers G, Annaloro C, Oriani A, Soligo D, Pozzoli E, Polli EE . Prognostic relevance of histological findings on bone marrow biopsy in myelodysplastic syndromes. Ann Hematol 1993; 66: 85–91.
Mangi MH, Mufti GJ . Primary myelodysplastic syndromes: diagnostic and prognostic significance of immunohistochemical assessment of bone marrow biopsies. Blood 1992; 79: 198–205.
Rios A, Canizo MC, Sanz MA, Vallespi T, Sanz G, Torrabadella M et al. Bone marrow biopsy in myelodysplastic syndromes: morphological characteristics and contribution to the study of prognostic factors. Br J Haematol 1990; 75: 26–33.
Toyama K, Ohyashiki K, Yoshida Y, Abe T, Asano S, Hirai H et al. Clinical and cytogenetic findings of myelodysplastic syndromes showing hypocellular bone marrow or minimal dysplasia, in comparison with typical myelodysplastic syndromes. Int J Hematol 1993; 58: 53–61.
Tricot G, De Wolf-Peeters C, Hendrickx B, Verwilghen RL . Bone marrow histology in myelodysplastic syndromes. I. Histological findings in myelodysplastic syndromes and comparison with bone marrow smears. Br J Haematol 1984; 57: 423–430.
Yoshida Y, Oguma S, Uchino H, Maekawa T . Refractory myelodysplastic anaemias with hypocellular bone marrow. J Clin Pathol 1988; 41: 763–767.
Jaffe ES . Pathology and Genetics of Tumours of Haematopoietic and Lymphoid Tissues. IARC Press: Lyon. Oxford University Press: Oxford, 2001, pp 47.
Harris NL, Jaffe ES, Diebold J, Flandrin G, Muller-Hermelink HK, Vardiman J et al. World Health Organization classification of neoplastic diseases of the hematopoietic and lymphoid tissues: report of the Clinical Advisory Committee meeting-Airlie House, Virginia, November 1997. J Clin Oncol 1999; 17: 3835–3849.
Tuzuner N, Cox C, Rowe JM, Watrous D, Bennett JM . Hypocellular myelodysplastic syndromes (MDS): new proposals. Br J Haematol 1995; 91: 612–617.
Chen CY, Lin LI, Tang JL, Ko BS, Tsay W, Chou WC et al. RUNX1 gene mutation in primary myelodysplastic syndrome—the mutation can be detected early at diagnosis or acquired during disease progression and is associated with poor outcome. Br J Haematol 2007; 139: 405–414.
Riccardi A, Giordano M, Girino M, Cazzola M, Montecucco CM, Cassano E et al. Refractory cytopenias: clinical course according to bone marrow cytology and cellularity. Blut 1987; 54: 153–163.
Acknowledgements
This work was sponsored in part by grants from the National Science Council of Taiwan NSC 94-2314-B-002-143 and 95-2314-B-002-042. We are grateful to Ms Fen-Yu Lee and Ms Min-Chih Liu for their help in chromosome study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Huang, TC., Ko, BS., Tang, JL. et al. Comparison of hypoplastic myelodysplastic syndrome (MDS) with normo-/hypercellular MDS by International Prognostic Scoring System, cytogenetic and genetic studies. Leukemia 22, 544–550 (2008). https://doi.org/10.1038/sj.leu.2405076
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.leu.2405076
Keywords
This article is cited by
-
Hypocellular myelodysplastic syndromes (h-MDS): from clinical description to immunological characterization in the Italian multi-center experience
Leukemia (2022)
-
Influence of platelet count at diagnosis and during the course of disease on prognosis in MDS patients
Annals of Hematology (2021)
-
Enumeration of CD34+ blasts by immunohistochemistry in bone marrow biopsies from MDS patients may have significant impact on final WHO classification
Journal of Hematopathology (2020)
-
Outcome of allogeneic hematopoietic stem cell transplantation for hypoplastic myelodysplastic syndrome
International Journal of Hematology (2020)
-
Impact of somatic mutations in myelodysplastic patients with isolated partial or total loss of chromosome 7
Leukemia (2020)