Abstract
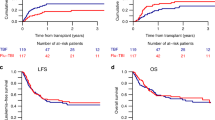
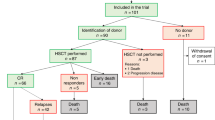
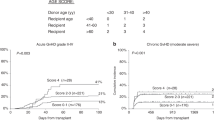
Twenty-nine consecutive patients with high-risk hematological malignancy aged from 3 to 58 years underwent an unmanipulated graft from an HLA-identical sibling after an irradiation-free preparative regimen consisting of idarubicin (IDA), 21 mg/m2/day administered by continuous infusion on days −12 and −11, followed by busulphan (BU), 4 mg/kg/day orally from day −7 to −4, and cyclophosphamide (CY), 60 mg/kg/day intravenously on days −3 and −2 (IDA-BUCY2). Most clinically relevant extra-hematological regimen-related toxicities consisted of stomatitis observed in all subjects and hemorrhagic cystitis occurred in five cases (17%) within 100 days after transplant. Six patients (21%) developed a grade 2 acute graft-versus-host disease (GVHD) and three (10%) a grade 3 or 4; extensive chronic GVHD was assessed in nine of 22 (41%) evaluable patients. So far, 12 patients have died and 17 are alive, 16 of whom disease-free, 5–41 months after transplant (median, 15 months). The causes of death were related to GVHD in three patients, to sepsis in one and to disease recurrence in the remaining eight. At present, only one of nine relapsed patients is alive. For all patients the actuarial probability of survival (OS) at 1 and 2 years ± standard error (s.e.) was 63 ± 9% and 52 ± 10%, respectively. The actuarial probabilities of disease-free survival (DFS), relapse and transplant-related mortality (TRM) at both 1 and 2 years ± s.e. were 53 ± 9%, 35 ± 9% and 16 ± 7%, respectively. These results are encouraging but not substantially different from those obtained in 28 patients with malignancy in advanced phase transplanted after the standard BUCY2 regimen, who had an actuarial probability of OS, DFS, relapse and TRM projected at 10 years ± s.e. of 54 ± 10%, 57 ± 9%, 36 ± 9% and 11 ± 6%, respectively. Although the retrospective comparison between the two groups does not seem to show any advantage in the use of the IDA intensified regimen, only a prospective randomized trial could answer this question.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Thomas ED . Marrow transplantation for malignant disease (Karnofsky Memorial Lecture) J Clin Oncol 1983 1: 517–531
Santos GW, Tutschka PJ, Brookmeyer R, Saral R, Beschorner WE, Bias WB, Braine HG, Burns WH, Effenbein GJ, Kaizer H, Mellits D, Sensenbrenner LL, Stuart RK, Yeager AM . Marrow transplantation for acute non-lymphocytic leukemia after treatment with busulphan and cyclophosphamide New Engl J Med 1983 309: 1347–1353
Tutschka PJ, Copelan EA, Klein JP . Bone marrow transplantation for leukemia following a new busulfan and cyclophosphamide regimen Blood 1987 70: 1382–1388
Blume KG, Kopecky KJ, Henslee-Downey JP, Forman SJ, Stiff PJ, LeMaistre CF, Appelbaum FR . A prospective randomized comparison of total body irradiation-etoposide versus busulfan-cyclophosphamide as preparatory regimens for bone marrow transplantation in patients with leukemia who were not in first remission: a Southwest Oncology Group Study Blood 1993 81: 2187–2193
Ringdèn O, Ruutu T, Remberger M, Nikoskelainen J, Volin L, Vindelov L, Parkkali T, Lenhoff S, Sallarfors B, Ljungman P, Mellander L, Jacobsen N for the Nordic Bone Marrow Transplantation Group . A randomized trial comparing busulphan with total body irradiation as conditioning in allogeneic marrow transplant recipients with leukemia: a report from the Nordic Bone Marrow Transplantation Group Blood 1994 83: 2723–2730
Ringdèn O, Labopin M, Tura S, Arcese W, Iriondo A, Zittoun R, Sierra J, Gorin C for the Acute Leukaemia Working Party of the EBMT . A comparison of busulphan versus total body irradiation combined with cyclophosphamide as conditioning for autograft or allograft bone marrow transplantation in patients with acute leukemia Br J Haematol 1996 93: 637–645
Linch MHE, Petersen FB, Appelbaum FR, Bensinger WI, Clift RA, Storb R, Sanders JE, Hansen JA, Buckner CD . Phase II study of busulfan, cyclophosphamide and fractionated total body irradiation as a preparatory regimen for allogeneic bone marrow transplantation in patients with advanced myeloid malignancies Bone Marrow Transplant 1995 15: 59–64
Demirer T, Buckner CD, Appelbaum FR, Lambert K, Bensinger WI, Clift R, Storb R, Slattery JT . Busulfan, cyclophosphamide and fractionated total body irradiation for allogeneic marrow transplantation in advanced acute and chronic myelogenous leukemia: phase I dose escalation of busulfan based on targeted plasma levels Bone Marrow Transplant 1996 17: 341–346
Hirabayashi N, Goto S, Ishii M, Yuge M, Mitsuma A, Noda N . Busulfan, cyclophosphamide and total body irradiation as conditioning for allogeneic bone marrow transplantation for acute and chronic myeloid leukemia Bone Marrow Transplant 1998 21: 1079–1083
Przepiorka D, Ippoliti C, Giralt S, Van Beisen K, Mehra R, Deisseroth AB, Andersson B, Luna M, Cork A, Lee M, Estey E, Andreeff M, Champlin R . A phase I–II study of high-dose thiotepa, busulfan and cyclophosphamide as a preparative regimen for allogeneic marrow transplantation Bone Marrow Transplant 1994 14: 449–453
Carpenter PA, Marshall GM, Giri N, Vowels MR, Russell SJ . Allogeneic bone marrow transplantation for children with acute lymphoblastic leukemia conditioned with busulfan, cyclophosphamide and melphalan Bone Marrow Transplant 1996 18: 489–494
Vaughan WP, Dennison JD, Reed EC, Klassen L, McGuire TR, Sanger WG, Kumar PP, Warkentin PI, Gordon BG, Bierman PJ, Coccia PF, Armitage JO . Improved results of allogeneic bone marrow transplantation for advanced hematologic malignancy using busulfan, cyclophosphamide and etoposide as cytoreductive and immunosuppressive therapy Bone Marrow Transplant 1991 8: 489–495
Raemaekers J, De Witte T, Schattenberg A, Van Der Lely N . Prevention of leukemic relapse after transplantation with lymphocyte depleted marrow by intensification of the conditioning regimen with a 6-day continuous infusion of anthracycline Bone Marrow Transplant 1989 4: 167–171
Muus P, De Witte T, Schattenberg A, Donnely P, Hoogenhout J . Intensification of the conditioning regimen for allogeneic bone marrow transplantation in recipients of T-cell depleted graft by the addition of anthracyclines Leuk Lymphoma 1992 7: 1–6
Muus P, Donnelly P, Schattenberg A, Linssen P, Minderman H, Dompeling E, De Witte T . Idarubicin-related side effects in recipients of T-cell depleted allogeneic bone marrow transplants are schedule dependent Semin Oncol 1993 20: 47–52
Schaap N, Schattenberg A, Bar B, Preijers F, Geurts Van Kessel A, Van Der Maazen R, De Boo T, De Witte T . Outcome of transplantation for standard-risk leukaemia with grafts depleted of lymphocytes after conditioning with an intensified regimen Br J Haematol 1997 98: 750–759
Glucksberg H, Storb R, Fefer A, Buckner CD, Neiman PE, Clift RA, Lerner KG, Thomas ED . Clinical manifestations of graft-versus-host disease in human recipients of marrow from HLA-matched sibling donors Transplantation 1974 18: 295–304
Shulman HM, Sullivan KM, Weiden PL, McDonald GB, Striker GE, Sale GE, Hackman R, Tsoi MS, Storb R, Thomas ED . Chronic graft-versus-host syndrome in man: a long-term clinicopathologic study of 20 Seattle patients Am J Med 1980 69: 204–217
Bearman SI, Appelbaum FR, Buckner CD, Petersen FB, Fisher LD, Clift RA, Thomas ED . Regimen-related toxicity in patients undergoing bone marrow transplantation J Clin Oncol 1988 6: 1562–1568
Kaplan EL, Meier P . Non parametric estimation from incomplete observations J Am Stat Assoc 1958 53: 457–481
Jones RJ, Lee KSK, Beschorner WE, Vogel VG, Grochow LB, Braine HG, Vogelsang GB, Sensenbrenner LL, Santos GW, Saral R . Veno-occlusive disease of the liver following bone marrow transplantation Transplantation 1987 44: 778–783
Berman E, McBride M . Comparative cellular pharmacology of daunorubicin and idarubicin in human multidrug resistant leukemia cells Blood 1992 79: 3267–3276
Donnelly JP, Muus P, Schattenberg A, De Witte T, Horrevorts A, DePauw BE . A scheme for daily monitoring of oral mucositis in allogeneic BMT recipients Bone Marrow Transplant 1992 9: 409–413
Sencer SF, Haake RJ, Weisdorf DJ . Hemorrhagic cystitis after bone marrow transplantation Transplantation 1993 56: 875–879
Bensinger WI, Weaver CH, Appelbaum FR, Rowley S, Demirer T, Sanders J, Storb R, Buckner CD . Transplantation of peripheral blood stem cells mobilised by recombinant human granulocyte colony stimulating factor Blood 1995 85: 1655–1658
Bensinger WI, Clift R, Martin P, Appelbaum FR, Demirer T, Gooley T, Lilleby K, Rowley S, Sanders J, Storb R, Buckner CD . Allogeneic peripheral blood stem cell transplantation in patients with advanced hematologic malignancies: a retrospective comparison with marrow transplantation Blood 1996 88: 2794–2800
Dupriez B, Morel P, Demory JL, Lai JL, Simon M, Plantier I, Bauters F . Prognostic factors in agnogenic myeloid metaplasia: a report on 195 cases with a new scoring system Blood 1996 88: 1013–1018
Abraham R, Szer J, Bardy P, Grigg AP . Early cyclosporine taper in high risk sibling allogeneic bone marrow transplants Bone Marrow Transplant 1997 20: 773–777
Ringdèn O, Labopin M, Gluckman E, Reiffers J, Vernant JP, Jouet JP, Harrousseau JL, Fiere D, Bacigalupo A, Frassoni F, Gorin NC for the Acute Leukemia Working Party of the European Group for Blood and Marrow Transplantation . Graft-versus-leukemia effect in allogeneic marrow transplant recipients with acute leukemia is maintained using cyclosporin A combined with methotrexate as prophylaxis Bone Marrow Transplant 1996 18: 921–929
Carella AM, Champlin R, Slavin S, McSweeney P, Storb R . Mini-allografts: ongoing trials in humans Bone Marrow Transplant 2000 25: 345–350
Grigg AP, Szer J, Beresford J, Dodds A, Bradstock K, Durrant S, Schwarer AP, Hughes T, Herrmann R, Gibson J, Arthur C, Matthews J . Factors affecting the outcome of allogeneic bone marrow transplantation for adult patients with refractory or relapsed acute leukemia Br J Haematol 1999 107: 409–418
Acknowledgements
We would like to thank Esterina Livesi for her invaluable support and all the nursing staff. This work was supported in part by grants from the ROMAIL (Associazione Italiana contro le Leucemie-Roma).
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Mengarelli, A., Iori, A., Guglielmi, C. et al. Idarubicin intensified BUCY2 regimen in allogeneic unmanipulated transplant for high-risk hematological malignancies. Leukemia 14, 2052–2058 (2000). https://doi.org/10.1038/sj.leu.2401947
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.leu.2401947
Keywords
This article is cited by
-
Idarubicin-intensified BUCY2 regimens may lower relapse rate and improve survival in patients undergoing allo-SCT for high-risk hematological malignancies: a retrospective analysis
Bone Marrow Transplantation (2012)
-
A comparative study of outcomes of idarubicin- and etoposide-intensified conditioning regimens for allogeneic peripheral blood stem cell transplantation in patients with high-risk acute leukemia
Acta Pharmacologica Sinica (2009)
-
Continuous infusion idarubicin and oral busulfan as conditioning for patients with acute myeloid leukemia aged over 60 years undergoing autologous stem cell transplantation
Bone Marrow Transplantation (2004)