Abstract
Objective:
To examine the nutritional implications of the interactions taking place between patients and care providers during mealtimes in hospital settings. Specifically, we tested research propositions that the amount and nature of interpersonal behaviours exchanged between patients and providers impact patients' food intake. These propositions were derived from prior evidence of social influences on eating behaviour and a well-established framework that identifies two fundamental modalities of human interaction: striving for mastery and power (agency) and efforts to promote union with others (communion).
Design:
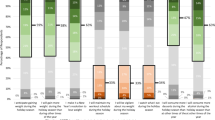
In a within-subject naturalistic study, participants were observed on multiple meals (n=1477, 46.2 meals/participant on average), during which participants' and providers' agency- and communion-related behaviours and patients' protein and energy intake were recorded. Meal-level frequency and complementarity of patients' and providers' behaviours were computed to test research propositions.
Setting:
Dining room of a geriatric rehabilitation unit.
Subjects:
Thirty-two elderly patients (21 females, mean age:78.8, 95% CI: 76.4, 81.1).
Results:
Meal-level frequency of patient–provider exchanges (P=0.016) and patients' agency-related behaviours (P=0.029), as well as mutual reciprocation of patients' and providers' communion-related behaviours (P=0.015) on a given meal were positively linked to protein intake. Higher energy intake was found during meals where patients expressed more agency-related behaviours (P=0.029).
Conclusion:
Results present evidence that the amount and nature of patient–provider interpersonal exchanges on a given meal influence the nutritional quality of food intake in hospitalized elderly. They provide insights into how to improve the design and delivery of routine care to this malnutrition-prone population.
Sponsorship:
This study was supported by the Canadian Institutes of Health Research (Operating grant to Laurette Dubé, Doctoral Fellowship to Catherine Paquet) the Fonds de la Recherche en santé du Québec and by the Danone Institute (Doctoral fellowship to Danielle St-Arnaud McKenzie).
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
References
Andersen PA, Guerrero LK (1998). The bright side of relational communication: Interpersonal warmth as a social emotion. In: Andersen PA, Guerrero LK (eds) Handbook of Communication and Emotion: Research applications, and contexts. Academic Press: San Diego.
Barton AD, Beigg CL, Macdonald IA, Allison SP (2000). High food wastage and low nutritional intakes in hospital patients. Clin Nutr 19, 445–449.
Berrut G, Favreau AM, Dizo E, Tharreau B, Poupin C, Gueringuili M et al. (2002). Estimation of calorie and protein intake in aged patients: validation of a method based on meal portions consumed. J Gerontol A Biol Sci Med Sci 57, M52–M56.
Braddom R. (2001). Physical Medicine and Rehabilitation. 2nd edn. Saunders: Philadelphia.
Cartensen LL, Isaacowitz DM, Charles ST (1999). Taking time seriously: a theory of socioemotional selectivity. Am Psychol 54, 165–181.
Chima CS, Barco K, Dewitt ML, Maeda M, Teran JC, Mullen KD (1997). Relationship of nutritional status to length of stay, hospital costs, and discharge status of patients hospitalized in the medicine service. J Am Diet Assoc 97, 975–980.
Clenenden VI, Herman CP, Polivy J (1994). Social facilitation of eating among friends and strangers. Appetite 43, 1–13.
Compan B, di Castri A, Plaze JM, Arnaud-Battandier F (1999). Epidemiological study of malnutrition in elderly patients in acute, sub-acute and long-term care using the MNA. J Nutr Health Aging 3, 146–151.
Comstock EM, St Pierre RG, Mackiernan YD (1981). Measuring individual plate waste in school lunches. Visual estimation and children's ratings vs. actual weighing of plate waste. J Am Diet Assoc 79, 290–296.
Crogan NL, Pasvogel A (2003). The influence of protein–calorie malnutrition on quality of life in nursing homes. J Gerontol A Biol Sci Med Sci 58, 159–164.
de Castro JM (1990). Social facilitation of duration and size but not rate of the spontaneous meal intake in humans. Physiol Behav 47, 1129–1135.
de Castro JM (1994). Family and friends produce greater social facilitation of food intake than other companions. Physiol Behav 56, 445–455.
de Castro JM (2002). Age-related changes in the social, psychological, and temporal influences on food intake in free-living, healthy, adult humans. J Gerontol A Biol Sci Med Sci 57, M368–M377.
de Castro JM, Brewer E (1992). The amount eaten in meals by humans is a power function of the number of people present. Physiol Behav 51, 121–125.
de Castro JM, de Castro ES (1989). Spontaneous meal patterns of humans: influence of the presence of other people. Am J Clin Nutr 50, 237–247.
Dubois S (1990). Accuracy of visual estimates of plate waste in determination of food consumption. J Am Diet Assoc 90, 382–387.
Edwards JS, Hartwell HJ (2004). A comparison of energy intake between eating positions in a NHS hospital – a pilot study. Appetite 43, 323–325.
Feunekes GI, de Graaf C, van Staveren WA (1995). Social facilitation of food intake is mediated by meal duration. Physiol Behav 58, 551–558.
Folstein MF, Folstein SE, McHugh PR (1975). Mini-mental state: a practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res 12, 189–198.
French SJ (1999). The effects of specific nutrients on the regulation of feeding behaviour in human subjects. Proc Nutr Soc 58, 533–539.
Grandey AA, Fisk GM, Mattila AS, Jansen KJ, Sideman LA (2005). Is ‘service with a smile’ enough? Authenticity of positive displays during service encounters. Organ Behav Hum Decis Process 96, 38.
Hochschild AR (2003). Behind Every Great Caregiver: The Emotional Labor in Health Care. In: Dubé L, Ferland G and Moskowitz DS (eds.) Enriching the Art of Care with the Science of Care: Emotional and Interpersonal Dimensions of Health Service. McGill Queen's Academic Press: Montreal, pp 67–73.
Incalzi RA, Gemma A, Capparella O, Cipriani L, Landi F, Carbonin P (1996). Energy intake and in-hospital starvation. A clinically relevant relationship. Arch Intern Med 156, 425–429.
Kiesler DJ (1983). The 1982 Interpersonal Circle: a taxonomy for complementarity in human transactions. Psychol Rev 90, 185–214.
Kondrup J, Johansen N, Plum LM, Bak L, Larsen IH, Martinsen A et al. (2002). Incidence of nutritional risk and causes of inadequate nutritional care in hospitals. Clin Nutr 21, 461–468.
Morley JE, Silver AJ (1995). Nutritional issues in nursing home care. Ann Intern Med 123, 850–859.
Moskowitz DS (1990). Convergence of self-reports and independent observers: dominance and friendliness. J Pers Soc Psychol 58, 1096–1106.
Moskowitz DS (1994). Cross-situational generality and the interpersonal circumplex. J Pers Soc Psychol 66, 921–933.
Moskowitz DS, Côté S (1995). Do interpersonal traits predict affect? A comparison of three models. J Pers Soc Psychol 69, 915–924.
Moskowitz DS, Pinard G, Zuroff DC, Annable L, Young SN (2001). The effect of tryptophan on social interaction in everyday life: a placebo-controlled study. Neuropsychopharmacology 25, 277–289.
Moskowitz DS, Suh EJ, Desaulniers J (1994). Situational influences on gender differences in agency and communion. J Pers Soc Psychol 66, 733–761.
Paquet C, St-Arnaud-McKenzie D, Ferland G, Dubé L (2003). A blueprint-based case study analysis of nutrition services provided in a midterm care facility for the elderly. J Am Diet Assoc 103, 363–368.
Pliner P, Bell R, Hirsch ES, Kinchla M (2006). Meal duration mediates the effect of ‘social facilitation’ on eating in humans. Appetite 46, 189–198.
Potter J, Klipstein K, Reilly JJ, Roberts M (1995). The nutritional status and clinical course of acute admissions to a geriatric unit. Age Ageing 24, 131–136.
Ryan RM, Deci EL (2000). Self-determination theory and the facilitation of intrinsic motivation, social development, and well-being. Am Psychol 55, 68–78.
Singer JD (1998). Using SAS PROC MIXED to fit multilevel models, hierarchical models, and individual growth models. J Educ Behav Stat 24, 323–355.
Sullivan DH, Sun S, Walls RC (1999). Protein-energy undernutrition among elderly hospitalized patients: a prospective study. JAMA 281, 2013–2019.
Thomas DR, Zdrowski CD, Wilson MM, Conright KC, Lewis C, Tariq S et al. (2002). Malnutrition in subacute care. Am J Clin Nutr 75, 308–313.
Visvanathan R, Penhall R, Chapman I (2004). Nutritional screening of older people in a sub-acute care facility in Australia and its relation to discharge outcomes. Age Ageing 33, 260–265.
Wagner CC, Kiesler DJ, Schmidt JA (1995). Assessing the interpersonal transaction cycle: convergence of action and reaction interpersonal circumplex measures. J Pers Soc Psychol 69, 938–949.
Wiggins JS (1991). Agency and communion as conceptual coordinates for the understanding and measurement of interpersonal behaviour. In: Grove W and Cicchetti D (eds.) Thinking clearly about psychology: Essays in honor of Paul Everett Meehl. University of Minnesota Press: Minneapolis. pp 89–113.
Williamson DA, Allen HR, Martin PD, Alfonso AJ, Gerald B, Hunt A (2003). Comparison of digital photography to weighed and visual estimation of portion sizes. J Am Diet Assoc 103, 1139–1145.
Woodward VM (1998). Caring, patient autonomy and the stigma of paternalism. J Adv Nurs 28, 1046–1052.
Yesavage JA, Brink TL, Rose TL, Lum O, Huang V, Adey MB et al. (1983). Development and validation of a geriatric depression screening scale: A preliminary report. J Psychiatr Res 17, 37–49.
Acknowledgements
We are indebted to health professionals and the staff of the dietetics and food services of the Institut Universitaire de Gériatrie de Montréal for their help and collaboration during the conduction of the study.
Author information
Authors and Affiliations
Corresponding author
Additional information
Guarantors: L Dubé and C Paquet.
Contributors: LD, CP, DSM, MJK and GF were responsible for the study concept and research design. CP and ZM performed data analysis. LD and CP drafted and edited the manuscript. All authors critically revised the article for important intellectual content.
Rights and permissions
About this article
Cite this article
Dubé, L., Paquet, C., Ma, Z. et al. Nutritional implications of patient–provider interactions in hospital settings: evidence from a within-subject assessment of mealtime exchanges and food intake in elderly patients. Eur J Clin Nutr 61, 664–672 (2007). https://doi.org/10.1038/sj.ejcn.1602559
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.ejcn.1602559
Keywords
This article is cited by
-
Effects of food neophobia and oral health on the nutritional status of community-dwelling older adults
BMC Geriatrics (2022)
-
Resident interactions at mealtime: an exploratory study
European Journal of Ageing (2010)
-
The evolution of nutritional status of geriatric patients without cachexia is associated with food intake in sub-acute care
The Journal of nutrition, health and aging (2009)