Abstract
Objective:
To determine if staffing level is associated with poor nutrition in the long-term residential care setting, adjusting for other confounding factors.
Design:
Cross-sectional survey.
Setting:
In total, 14 residential care facilities in Hong Kong, stratified by nature (government subvention or for-profit) to reflect the overall proportion in Hong Kong.
Subjects:
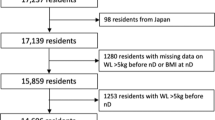
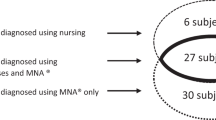
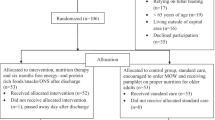
A total of 1914 subjects were assessed, using the Resident Assessment Instrument (RAI) 2.0. The response rate was 95% (1820 subjects), of which 1699 subjects had complete nutritional information.
Intervention:
Body mass index (BMI) was calculated by weighing and height measurement, and arm span was used if the subject could not stand. Subjects who were receiving parenteral or enteral nutrition via nasogastric of enterostomy tubes were excluded. A history of weight loss of 5% in the past month or 10% in the past 6 months, leaving 25% of food uneaten, and BMI <18.5 kg/m2 were examined as nutritional indicators. Association with age, gender, functional disability, oral problems, taste problems, presence of physical diseases and psychological well-being was examined using χ2-test, and multiple logistic regression.
Results:
In all, 26% of residents had a BMI <18.5 kg/m2, with a higher prevalence in the for-profit homes. History of weight loss and the record that 25% of food was left uneaten were poor indicators of low BMI. Multivariate analysis showed that having chronic obstructive airways disease, requiring help with feeding, being female, older age, were factors associated with an increased risk of poor nutrition, while being independent in activities of daily living and higher staff levels were associated with a reduced risk.
Conclusion:
Poor nutrition is a persistent problem in the long-term care setting, and inadequate staffing levels may be a reversible cause. However, resource limitations may render efforts at improvement difficult.
Sponsorship:
SK Yee Memorial Fund.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
References
Abbasi AA & Rudman D (1993): Observations on the prevalence of protein-calorie under nutrition in VA nursing homes. J. Am. Geriatric. Soc. 41, 117–121.
Beck AM, Oversen L & Schroll M (2001): Validation of the Resident Assessment Instrument triggers in the detection of under-nutrition. Age Ageing 30, 161–165.
Braithwaite J (2001): The challenge of regulating care for older people in Australia. BMJ 323, 443–446.
Brown DL (1995): Long term care facility Resident Assessment Instrument (RAI) User's Manual. Natick, MA: Eliot Press.
Chi I, Leung ACT, Cheng YH, Liu BCP & Chou KL (2001): A validation study of the Resident Assessment Instrument 2.0 (RAI 2.0) for the elderly in residential facilities in Hong Kong. University of Hong Kong Press, Hong Kong.
Chou KL, Chi I, Leung ACT, Wu YM & Liu CP (2001): Validation of minimum data set of nursing home for nursing home for Hong Kong Chinese elders. Clin. Gerontologist 23, 43–54.
Harrington C (2001): Regulating nursing homes: residential nursing facilities in the United States. BMJ 323, 507–510.
Hawes C, Mor V, Phillips CD, Fries BE, Morris JN, Steele-Friedlob E, Greene AM & Nennstiel M (1997): The OBRA-87 nursing home regulations and implementation of the resident assessment instrument: effects on process quality. J. Am. Geriatr. Soc. 45, 977–985.
Kane RL (2000): Changing the image of long-term care. Age Ageing 29, 481–483.
Kerrison SH & Pollock AM (2001): Regulating nursing homes: caring for older people in the private sector in England. BMJ 323, 566–569.
Kwok T & Whitelaw MN (1991): The use of armspan in nutritional assessment of the elderly. J. Am. Geriatr. Soc. 39, 492–496.
Lauque S, Arnaud-Battander F & Mansourian R et al (2000): Protein-energy oral supplementation in malnourished nursing home residents. A controlled trial. Age Ageing 29, 51–56.
Morley JE & Kraenzle D (1994): Causes of weight loss in a community nursing home. J. Am. Geriatr. Soc. 42, 583–585.
Morley JE & Silver AJ (1995): Nutritional issues in nursing home care. Ann. Intern. Med. 123, 850–859.
Munci HL & Carbonetto C (1982): Prevalence of protein-calorie malnutrition in an extended care facility. J. Fam. Pract. 14, 1061–1064.
Needleman J, Buerhaus P, Mattke S, Stewart M & Zelevinsky K (2002): Nurse-staffing levels and the quality of care in hospitals. N. Engl. J. Med. 346, 1715–1722.
Pinchcofsky-Devin GD & Kaminski Jr MV (1986): Correlation of pressure sores and nutritional status. J. Am. Geriatr. Soc. 34, 435–440.
Pokrywka HS, Koffler KH, Remsburg R, Bennett RG, Roth J, Tayback M & Wright JE (1997): Accuracy of patient care staff in estimating and documenting meal intake of nursing home residents. J. Am. Geriatr. Soc. 45, 1223–1227.
Richards K & Beck C (2002): Translating nursing home research into practice: how and for whom? J. Am. Geriatr. Soc. 50, 1595–1596.
Rudman D & Feller AG (1989): Protein-calorie undernutrition in the nursing home. J. Am. Geriatr. Soc. 37, 173–183.
Sandman PO, Adolfsson R, Nygren C, Hallmans G & Winblad B (1987): Nutritional status and dietary intake in institutionalized patients with Alzheimer's disease and multi infarct dementia. J. Am. Geriatr. Soc. 35, 31–38.
Schiffman SS & Warwick ZS (1989): Use of flavor-amplified goods to improve nutritional status in elderly persons. Ann. NY Acad. Sci. 561, 267–276.
Schols AM, Soeters PB, Dingemans AM, Mostert R, Frantzen PJ & Wouters EF (1993): Prevalence and characteristics of nutritional depletion in patients with stable COPD eligible for pulmonary rehabilitation. Am. Rev. Respir. Dis. 147, 1151–1156.
Shibata H (2001): Nutritional factors on longevity and quality of life in Japan. J. Nutr. Health Aging 5, 97–102.
Sullivan DH (1995): Impact of nutritional status on health outcomes of nursing home residents. J. Am. Geriatr. 43, 195–196.
Sullivan DH & Walls RC (1994): Impact of nutritional status on morbidity in a population of geriatric rehabilitation patients. J. Am. Geriatr. Soc. 42, 471–477.
Tang NLS, Chung ML, Elia M, Hui E, Lum CM, Luk JKH, Jones MG & Woo J (2002): Total daily energy expenditure in wasted chronic obstructive pulmonary disease patients. Eur. J. Clin. Nutr. 56, 282–287.
Thomas DR, Verdey RB, Gardner L, Kant A & Lindsay J (1991): A prospective study of outcome from protein-energy malnutrition in nursing home residents. J. Parenter. Enteral Nutr. 15, 400–404.
Vellas B, Garry PJ & Guigoz Y (1999): Mini Nutritional Assessment (MNA): Research and Practice in the Elderly. Nestle’ Nutrition Workshop Series, Clinical & Performance Programme Vol. 1, Basel, Switzerland: S Karger.
Woo J, Ho SC, Cheung CK, Mak YT & Swaminathan R (1989a): Protein calorie malnutrition in elderly chronic care institutions in Hong Kong. Nutr. Rep. Int. 40, 1011–1018.
Woo J, Ho SC, Mak YT, MacDonald D & Swaminathan R (1989b): Vitamin nutrition status in elderly Chinese subjects living in chronic care institutions. Nutr. Res. 9, 1071–1080.
Woo J, Ho SC & Sham A et al (1995): Influence of age, disease and disability on anthropometric indices in elderly Chinese aged 70 years and above. Gerontology 41, 173–180.
Acknowledgements
This study is supported by the SK Yee Memorial Fund.
Author information
Authors and Affiliations
Corresponding author
Additional information
Guarantor: J Woo.
Contributors: JW designed the study, organized the execution, arranged data analysis and wrote the paper. IC provided the major input in computerizing the RAI so that data entry could be carried out in the field and arranged data entry. EH and FC arranged and carried out the field study. AS analyzed the data.
Rights and permissions
About this article
Cite this article
Woo, J., Chi, I., Hui, E. et al. Low staffing level is associated with malnutrition in long-term residential care homes. Eur J Clin Nutr 59, 474–479 (2005). https://doi.org/10.1038/sj.ejcn.1602096
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.ejcn.1602096
Keywords
This article is cited by
-
Nutritional status of Chinese oldest-old adults (≥80 years of age): a cross-sectional study in Beijing
European Journal of Clinical Nutrition (2021)
-
Food security: Who is being excluded? A case of older people with dementia in long-term care homes
The Journal of nutrition, health and aging (2014)
-
Meeting the nutritional needs of elderly residents in aged-care: Are we doing enough?
The Journal of nutrition, health and aging (2013)
-
Consuming two additional serves of dairy food a day significantly improves energy and nutrient intakes in ambulatory aged care residents: A feasibility study
The Journal of nutrition, health and aging (2013)
-
Health, wellbeing and nutritional status of older people living in UK care homes: an exploratory evaluation of changes in food and drink provision
BMC Geriatrics (2010)