Abstract
Aim:
To evaluate resistance index (RI) changes in renal artery after N-acetylcysteine infusion in patients with systemic sclerosis.
Methods:
In an open-label study 40 patients with systemic sclerosis (SSc) were treated with N-acetylcysteine (NAC) iv infusion over 5 consecutive hours, at a dose of 0.015 g·kg−1·h−1. Renal haemodynamic effects were evaluated by color Doppler examination before and after NAC infusion.
Results:
NAC infusion significantly reduced RI in a group of sclerodermic patients with early/active capillaroscopic pattern, modified Rodnan Total Skin Score (mRTSS) <14 and mild-moderate score to the vascular domain of Medsger Scleroderma Disease Severity Scale (DSS). RI increased after NAC infusion in patients with late capillaroscopic pattern, mTRSS>14 and severe-end stage score to the vascular domain of DSS. In patients with reduction of RI after NAC infusion, diffusion capacity for carbon monoxide mean value was significantly higher than in those patients with an increase of RI. No significant differences in renal blood flow were found between patients with different subsets of SSc.
Conclusion:
In patients with low disease severity NAC ameliorates vascular renal function.
Similar content being viewed by others
Introduction
Systemic sclerosis (SSc) is a connective tissue disease characterized by fibrosis affecting the skin and the internal organs. Mortality and morbidity mostly depend on the involvement of lungs, heart, kidneys, and gastrointestinal tract1.
Renal complications are common in SSc although they are not always clinically significant. Scleroderma renal crisis is the most important renal complication and occurs in 10%−15% of the patients with diffuse cutaneous SSc and seldom if ever in patients with limited cutaneous SSc2. In the early 1980s the use of angiotensin-converting enzyme inhibitors dramatically decreased the incidence of SSc renal crisis, which until then significantly contributed to disease's mortality. Other patterns of renal involvement can be found in patients with SSc and in all of them vascular abnormalities are documented. Apart from scleroderma renal crisis, the majority of patients show less severe renal complications, more likely associated with reduced renal blood flow and consequent reduction in glomerular filtration rate3. Colour-flow Doppler ultrasonography is employed to evaluate renal vascular damage in SSc patients4. Doppler evaluation after prostacyclin infusion shows improved renal blood flow with a reduction of resistance index5.
N-acetylcysteine (NAC), a sulfhydryl substance with a powerful antioxidant and cellular detoxifying action, is a precursor of the major antioxidant glutathione. This medical compound has been proposed about 50 years ago as a mucolytic agent for chronic pulmonary diseases and it is now used for the treatment of fibrotic lung disease, since it restores pulmonary glutathione's depleted levels, thus improving lung function6. It is also used in the treatment of Raynaud's phenomenon (RP) and SSc because of its oxygen free radicals scavenging and vasodilative properties7, 8, 9.
NAC is particularly useful in improving myocardial function following an acute myocardial infarction10, 11. The prominent features of NAC are the enhancement of the glutathione system, elimination of peroxides and maintenance of ascorbate and α-tocopherol in their reduced states12. In patients with hypertension the glutathione system may be an effective way to decrease arterial pressure and to protect the kidney from damage. NAC treatment enhances the renal glutathione system, ameliorates renal function, markedly decreases arterial pressure and renal injury in salt-sensitive hypertension, and improves endothelial dysfunction by preventing the reduction of flow-mediated dilatation in dialysis patients13, 14.
This drug also has a relevant action on radiocontrast-induced nephropathy, which includes vasodilation, enhancement of renal medullary blood flow and antioxidant properties15.
The aim of our study was to evaluate the renal haemodynamic effects of NAC in different stages of SSc.
Materials and methods
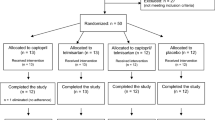
We studied 40 patients (3 males and 37 females; mean age 49±15 years) who fulfilled the American Rheumatism Association (ACR) criteria for SSc16. All SSc patients were subsequently divided into limited (lcSSc) and diffuse (dcSSc) cutaneous SSc groups according to LeRoy1. Table 1 lists epidemiological and clinical features of the study population.
The subjects' written consent was obtained according to the Declaration of Helsinki and the design of the work conforms to standards currently applied in the country of origin.
Exclusion criteria were: previous intravenous NAC infusion, arterial hypertension, pulmonary arterial hypertension, diabetes, liver or renal failure, therapy with dual or selective endothelin inhibitors and treatment with anti-hypertensive agents within 3 months before enrollment.
Clinical assessment
Patients underwent clinical assessment and the organs involvement was exhaustively investigated in each patient. Currently, modified Rodnan Total Skin Score (mRTSS) is the most used method to asses skin induration in SSc. It is determined at a standardized location of 17 different sites of the body with a standardized pinching method and it is scored from 0 to 317. Therefore mRTSS value significantly correlates with disease activity index in univariate analysis18. Valentini et al have proposed to modify the original activity index by changing the method used to assess the TSS and using a value of mRTSS >14. Disease activity in SSc was measured using Valentini's Scleroderma Disease Activity Score (SDAS), which consists of 10 weighted variables: total skin score >14, scleroderma, digital necrosis, arthritis, total lung capacity <80%, erythrocyte sedimentation rate (ESR) >30, hypocomplementemia and change in cardiopulmonary, skin and vascular symptoms in the past month19.
Disease severity was measured using Medsger Scleroderma Disease Severity Scale (DSS). The original scale assessed disease severity in 9 organs or systems, namely general health, peripheral vascular, skin, joint/tendon, muscle and gastrointestinal tract, lungs, heart and kidneys. Each organ/system is scored separately from 0 to 4 depending on whether there is no, mild, moderate, severe or end-stage involvement20. Our patients were divided on the basis of vascular domain: history of Raynaud's scored 1 (mild), digital pitting scars scored 2 (moderate), digital ulcerations scored 3 (severe) and digital gangrene scored 4 (end-stage).
Pulmonary function was tested by vital capacity (VC) and diffusion capacity for carbon monoxide (DLCO).
Renal evaluation
All patients were free of clinical symptoms of renal damage. Urinalysis, 24-h protein excretion, serum creatinine concentration and Glomerular Filtration Rate (GFR) were within normal limits.
GFR was calculated using both equation 7 developed in the Modification of Diet in Renal Disease (MDRD) study and Cockroft-Gault formula21.
MDRD formula does not require urine collection, using demographic and serum variables: GFR=170×[serum creatinine concentration (mg/dL)]−0.999×(age)−0.176×[serum urea nitrogen concentration (mg/dL)]−0.17×[albumin concentration (g/dL)]0.318×(0.762 if the patient is female)×(1.18 if the patient is black)22.
Creatinine clearance was also calculated using the Cockcroft and Gault formula: creatinine clearance=(140–age in yr)×weight (kg)×0.85 (if female) divided by serum creatinine concentration (mg/dL).
Medical treatment
NAC was administered as an iv infusion over 5 consecutive hours, at a dose of 0.015 g·kg−1·h-1 according to our previous studies8, 9.
Color Doppler examination
All patients underwent renal artery sonography before and after the 5-h treatment with NAC. Patients were examined in a supine position and studied by the same operator using a Toshiba Aplio equipment and a convex 3.5 MHz probe. All scans were initially performed in a gray-scale and then using a color Doppler module. After renal artery insonation the size of sample volume was optimised in each patient on the basis of the vessel's diameter.
Renal artery measurements
Renal artery measurements were: diameter expressed in cm, cross-sectional area in cm2, time-averaged mean velocity in cm/s and renal flow volume (RFV) in mL/min. Resistance index (RI) measures the intrarenal arterial elasticity and compliance rate. Determining the peak systolic velocity (Vmax) and the minimal diastolic velocity (Vmin) during intrarenal Doppler scan, RI is calculated as [1–(Vmin÷Vmax)×100]. Resistance index was calculated as the average of 2 to 3 measurements in proximal segmental arteries (the first vessels branching off the main renal artery).
Nailfold videocapillaroscopy (NVC)
NVC was performed by the same operator in each patient before NAC infusion using an optical probe videocapillaroscopy equipped with magnification 100×contact lens and connected to an image analysis software (Studio Version 8, Pinnacle System, Milan, Italy).
Each subject underwent acclimation for a minimum of 15 min before the nailfold was examined and the room temperature was 20–22 °C. The nailfold (distal row) of the second, third, fourth and fifth finger was examined in each patient. Microvascular alterations, as detected by NVC in patients with SSc, have been re-classified in three different patterns according to Cutolo et al. The patterns identified within the “SSc pattern” include Early NVC pattern: few enlarged/giant capillaries, few capillary haemorrhages, relatively well-preserved capillary distribution and no evident loss of capillaries; Active NVC pattern: frequent giant capillaries, frequent capillary haemorrhages, moderate loss of capillaries, mild disorganization of the capillary architecture and absent or mild ramified capillaries; Late NVC pattern: irregular enlargement of the capillaries, few or absent giant capillaries and haemorrhages, severe loss of capillaries with extensive avascular areas, disorganization of the normal capillary array and ramified/bushy capillaries23.
Statistical methods
The statistical significance of the differences between the data was tested using SPSS statistical software (version 15). The coefficient of skewness and coefficient of kurtosis are used to evaluate normal distribution of data. Paired two tailed Student's t-test was performed to compare differences in observation pre and post-infusion. Non-paired Student's test was performed for other numerical variables. P value less than 0.05 was considered significant.
Results
All data are normally distributed. Correlation before N-acetylcysteine treatment between epidemiological and clinical features (RP duration, disease duration, DSS, DLCO) and variables used for division into groups (capillaroscopic pattern, mRTTS, vascular score of DSS) have been shown in Table 2. RP duration mean was significantly (P<0.005) lower in patients with an early/active capillaroscopic pattern and with mild-moderate score than in those with a late capillaroscopic pattern and with severe-end stage vascular score (Table 2). Disease duration mean was significantly (P<0.005) lower in patients with an early/active capillaroscopic pattern and mild-moderate vascular score than in those with a late capillaroscopic pattern and severe-end stage vascular score (Table 2). Patients with an early/active capillaroscopic pattern and mild-moderate score showed a significantly lower global DSS score when compared to those with a late capillaroscopic pattern and severe-end stage score (Table 2). Mean DLCO did not show significant differences in two groups of patients with different capillaroscopic pattern and mRTSS (Table 2). Besides, mean DLCO (Table 2) was significantly (P<0.05) higher in patients with mild-moderate vascular score when compared to those patients with severe-end stage vascular score (70.6±12.9 vs 57.9±20). No significant differences (Table 2) are shown before NAC treatment in patients with mRTSS<14 when compared to those with mRTSS>14.
RFV mean values after a five-hour infusion with NAC did not decrease significantly in all patients. A non-significant association between RFV and capillaroscopic pattern, mRTSS, vascular domain of DSS and DLCO was found. Therefore RFV increased not significantly in patients with early/active capillaroscopic pattern, mRTSS<14, mild-moderate score to vascular domain of DSS. Conversely RFV decreased not significantly in patients with late capillaroscopic pattern, mRTSS>14 and severe-end stage score (Table 3).
RI is significantly (P=0.002) higher before NAC treatment in patients with mild-moderate score to vascular domain of DSS when compared to patients with severe-end stage score (0.734±0.074 vs 0.667±0.047). In all 40 patients RI mean values after a five-hour infusion with NAC did not decrease significantly (Table 3). Nevertheless, mean RI was significantly (P<0.01) reduced (0.723±0.0730 versus 0.678±0.0695) in patients with an early/active capillaroscopic pattern when compared to patients with a late pattern, in whom it was found a statistically significant increase of mean RI (Table 4).
RI is significantly (P=0.03) higher before NAC treatment in patients with an early/active capillaroscopic pattern when compared to patients with a late pattern (0.723±0.073 vs0.677±0.059). After NAC treatment no RI significant differences are present in patients with an early/active capillaroscopic pattern or mild-moderate score to vascular domain of DSS or with mRTSS<14 when compared to those with a late capillaroscopic pattern or severe-end stage score to vascular domain of DSS or mRTSS>14.
After NAC treatment mean RI was significantly (P<0.005) reduced (0.713±0.079 vs 0.678±0.072) in patients with mRTSS<14 when compared to those with mRTSS>14, whose mean RI was significantly increased (Table 4). Besides, patients with an mRTSS<14 showed a significantly (P<0.001) lower SDAS when compared to those with mRTSS>14 (0.78±0.49 vs3.13±0.48).
Mean RI was significantly decreased (P<<0.0001) in patients with mild-moderate score to vascular domain of DSS (0.734±0.074 vs 0.676±0.069), while it increased significantly in patients with severe-end stage score (Table 3).
DLCO mean (Figure 1) was significantly (P<0.005) lower in patients with RI increase than in those with reduction of RI (76.8±17.6 vs 60.6±18.1).
In all patients we did not find any correlation between haemodynamic parameters (RFV, RI) and SSc subset or E/A ratio evaluated to conventional transthoracic doppler echocardiographic examination. No change of blood pressure during NAC infusion was observed.
Discussion
NAC is a sulfhydryl substance with a powerful antioxidant, precursor of glutathione and donor of nitric oxide. Free radicals scavenger activity and support of gluthatione synthesis are probably two principles of its anti-oxidant function.
In SSc patients NAC treatment ameliorates the ROS-induced damage and reduces peroxynitrite production by lung macrophages9, 24. Threrefore, up to the present there are no clinical studies that investigate the effects of NAC infusion on renal blood flow in patients with SSc or primary RP. Scorza et al have shown that prostacyclin infusion ameliorates renal blood flow and reduces the RI in SSc patients5.
In our study we have evaluated renal haemodynamic effects before and after 5 h from a single NAC infusion with color Doppler examination. NAC infusion significantly reduced RI in a group of patients with early/active capillaroscopic pattern, mRTSS<14 and mild-moderate score to vascular domain of DSS. Conversely, RI was increased after NAC infusion in patients with late capillaroscopic pattern, mTRSS>14 and severe-end stage score to vascular domain of DSS. In addition, in patients with reduction of RI after NAC infusion, mean value of DLCO was significantly higher than in patients with an increase of RI.
RI measures the intrarenal arterial elasticity and compliance rate. It deteriorates more in vascular and interstitial nephropathies than in glomerular diseases, because glomeruli are only responsible for 10% of intraparenchimal flow resistances, whose control is mainly under the action of efferent and afferent arteries25, 26. The increase of total peripheral resistance of the kidney, determined by release of vasoconstrictive substances and remodeling of the microcirculation in course of vascular and interstitial nephropathies could explain the higher RI found in these diseases27.
In patients with Lupus nephritis, RI may be considered a significant predictor of poor renal outcome, correlating with a chronicity index on the basis of sclerosis, atrophy and fibrosis of Bowman capsule, glomeruli and the tubulointerstitium. When a parenchimal or interstitial damage occurs the renal vascular bed is reduced because of lacking in arteriolar elasticity and compliance with increased RI28. Although the pathogenesis of scleroderma renal crisis is unknown, endothelial cell injury, leading to narrowing and obliteration of the lumen of the vessels, is the primary pathogenetic mechanism. Vascular damage with arteries wall thickening is present in SSc patients without scleroderma renal crisis29. Renal vascular resistance was increased in main, interlobar and cortical vessels of SSc patients with normal renal function when compared with normal controls30. RI and pulsatility index are increased in SSc patients with signs of renal involvement when compared to those without renal manifestations and healthy controls. Doppler indices of renal vascular resistance were closely related to disease duration, age and plasma renin activity31. In SSc patients elevated pulsatility index correlates with digital pitting scar, contracture of the phalanges, pulmonary fibrosis, DLCO's percentage and heart involvement4.
RI was significantly improved by angiotensin II receptor blockers (ARBs). The reduction of RI after ARBs treatment was most evident in patients with hypertensive nephrosclerosis and/or with microalbuminuria or proteinuria32.
NAC improves renal vasoconstriction induced by radiocontrast, angiotensin II, indomethacin and Nω-nitro-L-arginine-methyl ester (L-NAME) in rats. NAC-induced renal vasodilation is greater after the most intense vasoconstrictive maneuvers33.
NAC-related RI reduction may be mediated in part by vasodilation of the small and medium arteries not involved in the thickening process. RI may increase because of the involvement of endothelial cells, which release vasoconstrictive and vasodilator factors, such as angiotensin II, endothelin and NO, as a physiological answer to the friction of hematic flow on vascular wall (shear stress)34, 35. During endothelial dysfunction reduced responsitivity to vasodilator impulses in small and medium size arteries is mediated by NO and acetylcholine, leading to the development of intimal hyperplasia, vascular lumen reduction, increase of vascular contractility and, in the end, ischemic and glomerular sclerosis, resulting in a RI increase. Similar vascular effects can be experimentally reproduced in rats by giving them NO inhibitors, such as L-NAME36.
Rajkumar et al reported a link between vascular damage (an essential requirement in any scheme of SSc pathogenesis) and the formation of myofibroblasts from pericytes. As primitive mesenchymal cells, pericytes can give origin to several tissues, including cartilage and bone. Thus, both tissue fibrosis and ectopic calcification could be attributed to pericytes37.
In SSc patients NAC induced renal arterial vasodilation only in early stage of disease when arteries are not involved by fibrosis. Vasodilative effects of NAC on renal artery are not present in late stage of SSc when arterial fibrosis, intimal hyperplasia, vascular lumen reduction are evident. For this reason NAC treatment should be started in early stage of disease, in association with other vasodilator drugs, because it may prevents progression of arterial renal fibrosis. The NAC as a vasodilator agent is effective only if introduced early, while the use in the late stage of the disease is restricted to its antioxidant effect. In late stage of disease NAC treatment for its negative effects in RI could be used only in combination with classic vasodilator drugs (prostacyclin analogues and ACE inhibitors). The indices of renal function (urinalysis, 24-h protein excretion, serum creatinine concentration and GFR) should be closely monitored if NAC therapy is started or continued in late stage of disease.
In conclusion, NAC is able to reduce RI after a single infusion in SSc patients with early/active capillaroscopic pattern, mRTSS<14 and mild-moderate score to vascular domain of DSS.
Author contribution
Felice SALSANO designed research; Edoardo ROSATO, Rosario CIANCI, Biagio BARBANO, Ginevra MENGHI, Antonietta GIGANTE, Carmelina ROSSI, Enrico M ZARDI, Antonio AMOROSO, and Simonetta PISARRI performed research; Edoardo ROSATO, Rosario CIANCI, and Biagio BARBANO analyzed data; Felice SALSANO and Edoardo ROSATO wrote the paper.
References
LeRoy EC, Black C, Fleischmajer R, Jablonska S, Krieg T, Medsger TA Jr, et al. Scleroderma (systemic sclerosis): classification, subsets and pathogenesis. J Rheumatol 1988; 15: 202–5.
Belch JJF . The clinical assessment of scleroderma spectrum disorders. Br J Rheumatol 1993; 32: 353–6.
Denton CP . Renal manifestations of systemic sclerosis-clinical features and outcome assessment. Rheumatology 2008; 47 Suppl 5: 54–6.
Nishijima C, Sato S, Hasegawa M, Nagaoka T, Hirata A, Komatsu K, et al. Renal vascular damage in Japanese patients with systemic sclerosis. Rheumatology (Oxford) 2001; 40: 406–9.
Scorza R, Rivolta R, Mascagni B, Berruti V, Bazzi S, Castagnone D, et al. Effect of iloprost infusion in the resistance index of renal vessels of patients with systemic sclerosis. J Rheumatol 1997; 24: 1944–8.
Behr J, Maier K, Degenkolb B, Krombach F, Vogelmeier C . Antioxidative and clinical effects of high-dose N-acetylcysteine in fibrosing alveolitis: adjunctive therapy to maintenance immunosuppression. Am J Respir Crit Care Med 1997; 156: 1897–901.
Merla A, Romani GL, Di Luzio S, Di Donato L, Farina G, Proietti M, et al. Raynaud's phenomenon: Infrared functional imaging applied to diagnosis and drug effects. Int J Immunopathol Pharmacol 2002; 15: 41–52.
Sambo P, Amico D, Giacomelli R, Matucci-Cerinic M, Salsano F, Valentini G, et al. Intravenous N-acetylcysteine for treatment of Raynaud's phenomenon secondary to systemic sclerosis: a pilot study. J Rheumatol 2001; 28: 2257–62.
Salsano F, Letizia C, Proietti M, Rossi C, Proietti AR, Rosato E, et al. Significant changes of peripheral perfusion and plasma adrenomedullin levels in N-acetylcysteine long term treatment of patients with sclerodermic Raynaud's phenomenon. Int J Immunopathol Pharmacol 2005; 18: 761–70.
Sochman J, Peregrin JH . Total recovery of left ventricular function after acute myocardial infarction: comprehensive therapy with streptokinase, N-acetylcysteine and percutaneous transluminal coronary angioplasty. Int J Cardiol 1992; 35: 116–8.
Sochman J, Vrbska J, Musilova B, Rocek M . Infarct size limitation: acute N-acetylcysteine defense (ISLAND) trial. Start of the study. Int J Cardiol 1995; 49: 181–2.
Jones DP . Redox potential of GSH/GSSG couple: assay and biological significance. Methods Enzymol 2002; 348: 93–112.
Tian N, Rose RA, Jordan S, Dwyer TM, Hughson MD, Manning RD Jr . N-Acetylcysteine improves renal dysfunction, ameliorates kidney damage and decreases blood pressure in salt-sensitive hypertension. J Hypertens 2006, 24: 2263–70.
Sahin G, Yalcin AU, Akcar N . Effect of N-acetylcysteine on endothelial dysfunction in dialysis patients. Blood Purif 2007; 25: 309–15.
Fishbane S, Durham JH, Marzo K, Rudnick M . N-Acetylcysteine in the prevention of radiocontrast-induced nephropathy. J Am Soc Nephrol 2004; 15: 251–60.
Subcommittee for Scleroderma Criteria of the American Rheumatism Association Dignostic and Therapeutic Criteria Committee. Preliminary criteria for classification of systemic sclerosis (scleroderma). Arthritis Rheum 1980; 23: 581–90.
Clements P, Lachenbruch P, Seibold J, Zee B, Steen VD, Brennan P, et al. Inter- and intraobserver variability of the total thickness score (modified Rodnan TSS) in systemic sclerosis. J Rheumatol 1995; 22: 1281–5.
Valentini G, D'Angelo S, Della Rossa A, Bencivelli W, Bombardieri S . European Scleroderma Study Group to define disease activity criteria for systemic sclerosis. IV. Assessment of skin thickening by modified Rodnan skin score. Ann Rheum Dis 2003; 62: 904–5.
Valentini G, Della Rossa A, Bombardieri S, Bencivelli W, Silman AJ, D'Angelo S, et al. European multicentre study to define disease activity criteria for systemic sclerosis. II. Identification of disease activity variables and development of preliminary activity indexes. Ann Rheum Dis 2001; 60: 592–8.
Medsger TA Jr, Silman AJ, Steen VD, Black CM, Akesson A, Bacon PA, et al. A disease severity scale for systemic sclerosis: development and testing. J Rheumatol 1999; 26: 2159–67.
Levey AS, Bosch JP, Lewis JB, Greene T, Rogers N, Roth D . A more accurate method to estimate glomerular filtration rate from serum creatinine: a new prediction equation. Modification of Diet in Renal Disease Study Group. Ann Intern Med 1999; 130: 461–70.
Kingdon EJ, Knight CJ, Dustan K, Irwin AG, Thomas M, Powis SH, et al. Calculated glomerular filtration rate is a useful screening tool to identify scleroderma patients with renal impairment. Rheumatology 2003; 42: 26–33.
Cutolo M, Sulli A, Pizzorni C, Accardo S . Nailfold videocapillaroscopy assessment of microvascular damage in systemic sclerosis. J Rheumatol 2000; 27: 155–60.
Failli P, Palmieri L, D'Alfonso C, Black CM, Akesson A, Bacon PA, et al. Effect of N-acetyl-L-cysteine on peroxynitrite and superosside anion production of lung alveolar macrophages in systemic sclerosis. Nitric Oxide 2002; 7: 277–82.
Platt JF . Duplex Doppler evaluation of native kidney dysfunction: obstructive and nonobstructive disease. Am J Roentgenol 1992; 158: 1035–42.
FitzGerald GA, Murray R, Price P, Catella F . The molecular, biochemical and human pharmacology of thromboxane A2 in renal disease. Adv Exp Med Biol 1989; 259: 325–60.
Pape L, Offner G, Ehrich JH . Renal arterial resistance index. N Engl J Med 2003; 349: 1573–4.
Platt JK, Ruin JM, Ellis JH . Lupus nephritis: predictive value of conventional and Doppler US and comparison with serologic and biopsy parameters. Radiology 1997; 203: 82–6.
Trostle DC, Bedetti CD, Steen VD, Al-Sabbagh MR, Zee B, Medsger TA Jr . Renal vascular histology and morphometry in systemic sclerosis. Arthritis Rheum 1988; 31: 393–400.
Rivolta R, Mascagni B, Berruti V, Quarto Di Palo F, Elli A, Scorza R, et al. Renal vascular damage in systemic sclerosis patients without clinical evidence of nepropathy. Arthritis Rheum 1996; 39: 1030–4.
Aikimbaev KS, Canataroğlu A, Ozbek S, Usal A . Renal vascular resistance in progressive systemic sclerosis: evaluation with duplex Doppler ultrasound. Angiology 2001; 52: 697–701.
Ogata C, Kamide K, Suzuki Y, Sasaki O, Kubota Y, Sato H, et al. Evaluation of intrarenal hemodynamics by Doppler ultrasonography for renoprotective effect of angiotensin receptor blockade. Clin Nephrol 2005; 64: 352–7.
Heyman SN, Goldfarb M, Shina A, Karmeli F, Rosen S . N-acetylcysteine ameliorates renal microcirculation: studies in rats. Kidney Int 2003; 63: 634–41.
Chien, S, Li S, Shyy YJ . Effects of mechanical forces on signal transduction and gene expression in endothelial cells. Hypertension 1998; 31: 162–9.
Houston P, Dickson MC, Ludbrook V, White B, Schwachtgen JL, McVey JH, et al. Fluid shear stress induction of the tissue factor promoter in vitro and in vivo is mediated by Egr-1. Arterioscler Thromb Vasc Biol 1999; 19: 281–9.
Quiroz Y, Pons H, Gordon KL, Rincón J, Chávez M, Parra G, et al. Mycophenolate mofetil prevents salt-sensitive hypertension resulting from nitric oxide synthesis inhibition. Am J Physiol Renal Physiol 2001; 281: F38–47.
Rajkumar VS, Howell K, Csiszar K, Denton CP, Black CM, Abraham DJ . Shared expression of phenotypic markers in systemic sclerosis indicates a convergence of pericytes and fibroblasts to a myofibroblast lineage in fibrosis. Arthritis Res Ther 2005; 7: 1113–23.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Rosato, E., Cianci, R., Barbano, B. et al. N-acetylcysteine infusion reduces the resistance index of renal artery in the early stage of systemic sclerosis. Acta Pharmacol Sin 30, 1283–1288 (2009). https://doi.org/10.1038/aps.2009.128
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/aps.2009.128
Keywords
This article is cited by
-
The immunological benefit of higher dose N-acetyl cysteine following mechanical ventilation in critically ill patients
DARU Journal of Pharmaceutical Sciences (2014)
-
Lipoic acid plays a role in scleroderma: insights obtained from scleroderma dermal fibroblasts
Arthritis Research & Therapy (2014)
-
Evaluation of the renal resistive index and pulsatility index in patients with pleural effusion by duplex Doppler ultrasonography
Japanese Journal of Radiology (2013)