Abstract
Depression and anxiety often coexist with rheumatoid arthritis (RA) and affect the course of the disease. These mental health conditions can be overlooked or underdiagnosed in people with RA. There is conflicting evidence in previous studies regarding this topic, indicating that further research is necessary to provide a thorough understanding of the relationship between anxiety, depression, and RA. This study aims to determine the factors correlated with depression and anxiety symptoms in RA patients by evaluating disease activity at the same time. This cross-sectional study was conducted at four outpatient rehabilitation centers in four Syrian provinces: Damascus, Homs, Hama, and Latakia. The study included RA patients who attended the RA department of rehabilitation centers from January 1 to June 31, 2023. RA patients who presented at a rheumatology clinic were selected consecutively. RA patients were included in the study in accordance with the ACR/EULAR classification criteria, disease activity was assessed by disease activity score based on the 28-joint count (DAS28), and patients with DAS28 > 2.6 were considered to have active RA. The demographic data, as well as disease duration, educational status, Disease Activity Score with 28-joint counts (DAS28), health assessment questionnaire (HAQ) score, and the hospital anxiety and depression scale (HADS), were the parameters used in the analysis. Two hundred and twelve patients (female, 75%) with a mean age of 49.3 ± 13.1 years and a mean disease duration of 8.3 ± 6.9 years were studied. Depression was diagnosed in 79 (37.3%) patients and anxiety in 36 (16.9%) patients. Patients with depression and/or anxiety had higher HAQ and DAS28 scores compared to other RA patients. Blue-collar workers exhibited a higher prevalence of anxiety, whereas females, housewives, and individuals with lower educational attainment demonstrated a higher prevalence of depression. The current study found high rates of anxiety and depression in RA patients, highlighting the significant burden of these mental health conditions compared to the general population. It is essential for healthcare providers not to overlook the importance of psychiatric evaluations, mental health assessments, and physical examinations of RA patients.
Similar content being viewed by others
Introduction
Rheumatoid arthritis (RA) is a chronic autoimmune disease primarily characterized by joint inflammation and damage. While its primary symptoms are related to joint pain, swelling, and stiffness, RA can also have systemic effects that extend beyond the joints. These systemic effects can include fatigue, sleep disturbances, and mood changes. This overlap can result in RA patients experiencing symptoms similar to those observed in individuals with depression1. Anxiety is also prevalent among individuals with RA, with approximately 20% of patients undergoing anxiety2. Another study has indicated that nearly 30% of RA patients experienced symptoms of depression during developing the disease3.
Patients diagnosed with RA who present with comorbid anxiety and depression symptoms tend to exhibit worse health outcomes, including poor medication adherence4, suboptimal response to treatment4, elevated medical costs5, increased mortality6, and diminished quality of life7. As a result, it is critical to investigate the risk factors for anxiety and depression symptoms in RA patients and to incorporate psychological management into their medical care. Several research studies have been carried out to improve RA control and prevention8,9,10,11.
According to a meta-analysis, depression was present in 17% of RA patients8. Additionally, another meta-analysis that included 10 cohort studies revealed that RA patients are at a significantly higher risk for anxiety than individuals without RA, with an odds ratio of 1.20 (95% confidence interval: 1.03–1.39)9. Another study of RA patients revealed a prevalence of 38.4% for patient-reported depression or anxiety, but only 17.7% of patients were diagnosed with depression or depression by their physicians. According to the same study10, patients with anxiety or depression had significantly higher levels of treatment dissatisfaction and impaired job and everyday activity.
The incidence of anxiety and depression in RA patients and their relationship with disease severity has varied among researchers. These inconsistencies could be related to differences in study populations, diagnostic criteria applied, the severity of depression or anxiety evaluated, and the distribution of associated factors in the general population. Furthermore, disease activity in RA patients, which reflects the aforementioned conditions, may contribute to developing depression and anxiety symptoms. However, study findings on the correlation between disease activity and anxiety and depression are inconsistent. Some studies have suggested a positive association between RA disease activity and anxiety and depression symptoms12,13, whereas others have not identified an association14.
Depression and rheumatoid arthritis (RA) demonstrate an interconnected relationship, as both conditions are linked to inflammation. Numerous studies have explored the impact of depression and inflammation on pain perception in RA12. These studies highlight that depression is frequently associated with more severe RA and unfavorable outcomes6. Additionally, symptoms of depression and anxiety correlate with subjective aspects of disease activity, reducing the likelihood of RA remission and influencing treatment decisions.
Research has shown that individuals with RA may experience higher rates of anxiety and depression compared to the general population. The chronic pain, physical limitations, and unpredictable nature of the disease can contribute to increased psychological distress. Additionally, the inflammatory processes involved in RA can have an impact on the central nervous system and neurotransmitter function, potentially contributing to the development or exacerbation of anxiety and depression15,16. It's important to note that anxiety and depression in RA can be influenced by various factors, including disease activity, pain levels, functional limitations, and socioeconomic factors. Therefore, it is crucial to address both the physical and psychological aspects of RA to provide comprehensive care for individuals with the condition17,18.
However, the prevalence of depression and anxiety among RA patients and their association with RA severity exhibit variability across different studies. This variability can be attributed to various factors, including the characteristics of the study population, criteria used for diagnosing and assessing the severity of depression or anxiety, methods employed for measuring RA activity, and the distribution of factors associated with depression or anxiety within the general population. Moreover, the coexistence of depression and anxiety with RA often goes undiagnosed or unrecognized due to the overlap in symptoms between these conditions and RA itself. In light of these challenges, the current study aims to determine the factors associated with depression and anxiety symptoms in RA patients by evaluating disease activity at the same time.
Methods
Patients and setting
This cross-sectional study was conducted at four outpatient rehabilitation centers in four Syrian provinces: Damascus, Homs, Hama, and Latakia. The study included RA patients who attended the RA department of rehabilitation centers from January 1 to June 31, 2023. This study included all the patients who met the 2010 American College of Rheumatology/European League Against Rheumatism classification criteria19,while depression and anxiety were diagnosed using the hospital anxiety and depression scale (HADS)20, a 14-item questionnaire with seven subscales for anxiety and depression symptoms. Each item is scored on a scale of 0–3, the total score range for each condition is 0–21. Scores of 0–7 indicate no or few anxiety or depression symptoms, 8–10 indicate mild anxiety or depression, and ≥ 11 indicate severe anxiety or depression. The Arabic version of the HADS has been widely used to screen patients with a variety of diseases and has been previously validated for use with the Arabic population21. In this study, we defined anxiety and depression as a HADS anxiety score ≥ 8 and a HADS depression score ≥ 8, respectively21.
Patient data has been obtained, including age, gender, marital status, employment position, BMI, disease duration, comorbidities, and medication use. The DAS28-ESR was used to assess disease activity, which is based on a 28-joint assessment; 28 tender joint counts (TJC), 28 swollen joint counts (SJC); and the patient global assessment (PtGA)22. [R1] The HAQ score was used to evaluate functional status23. Pain was evaluated using either the visual analogue scale (VAS), on which items were scored from 0 (no pain) to 100 (maximum pain)24.
This study included all patients who met the ACR/EULAR classification criteria, aged between 18 and 85 years and were willing to participate and provide informed consent. Any patient has a history of other autoimmune or inflammatory conditions (e.g. systemic lupus erythematosus, psoriatic arthritis), severe cognitive impairment or neurological disorders that may hinder accurate reporting of depression and anxiety symptoms, pregnant or lactating women, as hormonal changes during these periods can affect mood and anxiety levels, in addition to any patients has a history of psychological disorders (e.g. bipolar disorder, schizophrenia) or had coexisting chronic conditions such as chronic low back pain, chronic non-RA musculoskeletal diseases, cardiovascular disease, cerebrovascular diseases, and gastrointestinal diseases, were excluded from the study.
The Ethical Committee approved this study in the Al Baath University Institutional Review Board Consent Letter – IRB 2023168-S and all procedures were conducted under the ethical principles outlined in the 1964 Declaration of Helsinki and its subsequent revisions. Patients were informed of the study's purpose and procedures. In addition, written informed consent to participate in this study was provided by the participants.
Statistical analysis
The statistical analyses were performed with the assistance of version 23.0 of the SPSS for Windows software package. The data was evaluated using descriptive statistics such as means, standard deviations, and frequencies. Categorical data was measured using the chi-square test, while continuous variables were computed using Student’s t-test or the Mann–Whitney U test. Multivariate logistic regression analyses were used to determine the relationship between clinical and demographic factors and anxiety depression or anxiety among rheumatoid arthritis patients. The results were presented as odds ratios with 95% confidence intervals. A p-value less than 0.05 was considered statistically significant.
Ethics approval and consent to participate
The Ethical Committee approved this study in the Al Baath University Institutional Review Board Consent Letter – IRB 2023168-S and all procedures were conducted under the ethical principles outlined in the 1964 Declaration of Helsinki and its subsequent revisions. Patients were informed of the study's purpose and procedures. In addition, written informed consent to participate in this study was provided by the participants.
Results
This study included a cohort of 212 patients diagnosed with RA. The patients had a mean age (SD) of 49.3 ± 13.1 years (ranging from 20 to 73 years), and the average duration of the disease was 8.3 ± 6.9 years (ranging from 2 to 46 years). Among the participants, 70% were female. The mean DAS28 (SD) was 2.6 ± 1.2, and the mean HAQ score was 1.08 ± 1.2.
Tables 1 and 2 provides an overview of the descriptive statistics for various variables, including age, BMI, disease duration, DAS28, HAQ, and HADS scores, as well as information on gender, marital and working status, education level, comorbidities, and medications utilized. Based on the Arabic validation scores of the hospital anxiety and depression scale (HADS), anxiety symptoms were present in 16.9% of the patients, while depression symptoms were detected in 37.3% of the participants.
Tables 2 comprehensively compare various factors, including gender, marital and employment status, education level, comorbidities, and medication usage, among patients with and without anxiety and depression. The results revealed statistically significant differences in the working status between patients with and without anxiety and depression (p = 0.033, p = 0.042), respectively. Additionally, significant differences were observed in terms of sex and working status between patients with depression and those without depression (p < 0.05). Of particular note, it was found that anxiety levels were considerably higher in individuals employed in blue-collar occupations compared to retired patients. The prevalence of depression was significantly higher in women compared to men. Additionally, it was found to be more prevalent among patients with lower levels of education (uneducated) compared to those with a high school or university education. Furthermore, housewives had a higher prevalence of depression compared to retired patients.
Regarding medication usage, a comparison was made between users of bDMARD and csDMARD. The analysis revealed no statistically significant difference in the levels of anxiety and depression between these two groups of medication users. This information is detailed in Table 2.
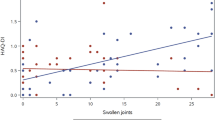
Table 3 presents the comparisons of BMI, age, duration of disease, HAQ, and DAS28 scores between different groups. It was observed that patients with both anxiety and depression had significantly higher DAS28 and HAQ scores compared to patients without depression and anxiety (p < 0.05), indicating higher disease activity and worse functional status.
Table 4 shows the multivariate logistic regression analysis results with anxiety and depression as dependent variables. The HAQ score and DAS28 were both significantly associated with anxiety (OR = 1.09, 95% CI 0.94–1.05, p = 0.012) (OR = 1.44, 95% CI 0.95–1.87, p = 0.041) and depression (OR = 1.23, 95% CI 1.25–2.87, p = 0.032) (OR = 1.43, 95% CI 1.03–1.67).
Discussion
RA is a chronic autoimmune disease that primarily affects the joints. It is characterized by inflammation of the synovial lining in multiple joints, leading to joint pain, swelling, stiffness, and progressive joint damage. RA is classified as an inflammatory type of arthritis. RA can also present with extra-articular manifestations, meaning it can affect other organs and systems in the body. These extra-articular manifestations can include symptoms such as depression, fatigue, and sleep disturbance25,26. This study aimed to determine the frequency and the factors affecting depression and anxiety in patients with RA.
In this study, depression was determined in 37.3% of the patients, and anxiety in 16.9%. Patients with depression and anxiety had significantly higher DAS28-ESR and HAQ scores than those without depression and anxiety. Depression was determined at a higher rate in females, patients with a low level of education, and housewives, while a university education level was associated with a reduced risk of depression. Anxiety was determined at higher rates in blue-collar workers. Our results are consistent with a study conducted by Altan et al.27 reported a depression rate of 44% and an anxiety rate of 38% in patients with RA, and a study conducted by Isık et al.28 that used the HADS-A and HADS-D scales and found anxiety and depression rates of 41.5% and 13.4% in patients with RA, On contract, in a systematic review of 21 studies that included 4,447 RA patients, found a prevalence of depression of 48%among RA patients29.
Different rates of depression and anxiety have been recorded in various research, and these disparities have been associated with factors such as study design, scales employed, and a probable relationship with geography and social and economic status29. In a study of Brazilian patients with RA, depression was more prevalent among Brazilians and high disease activity is associated with depression30. In another study conducted in Italy among RA patients, depression was detected in 14.3%. and it found a substantial rise in the risk of depression with male sex, a high HAQ score, patient global evaluation, and the use of antidepressants31. The results of this study are not consistent with previous studies, where sex, a high HAQ score, age, BMI, and disease duration do not show the risk of depression and anxiety, in return, it found that the work status has a significant increase in the risk of depression and anxiety among RA patients.
It is accepted that there is a two-way relationship between RA and depression20,29. Depression is seen more in RA patients, and there has been found to be an increased risk of RA development in individuals with depression. There are increased proinflammatory cytokines in depression similar to in RA, and these cytokines are reduced with antidepressant treatment8. In patients with severe depressive disorder, the risk of developing RA is increased by 38% compared to the normal population and the risk of RA development has been reported to be reduced in those using antidepressants compared to non-users32, some anti-cytokine treatments used in RA have been found to affect depression positively33.
In a study by Ng et al.34, anxiety and depression were strongly associated with DAS28-ESR. The study also found that depression was significantly lower in patients using etanercept, and these results are consistent with our study where anxiety and depression were associated with DAS28-ESR (p = 0.032, p = 0.021), respectively.
It is necessary to highlight the importance of the impact of depression and anxiety on the management and outcomes of rheumatoid arthritis. Understanding the association between mental health conditions and disease activity can aid in developing comprehensive treatment approaches for individuals with rheumatoid arthritis, wherein a study conducted by Matcham et al.35 on 18,421 RA patients receiving biological treatment revealed that the response to treatment in the first year was reduced by 20–40% when depression was present at the beginning of the treatment. These results suggest that depression can have a negative impact on the effectiveness of biological treatment in RA patients. In another study by Fragoulis et al.36, which involved 848 early RA patients, anxiety was reported to be 19.0%, while depression was 12.2%. The study also identified a relationship between depression and anxiety, disease activity, and poor functional outcomes in patients with early rheumatoid arthritis.
A low socioeconomic status, female sex, young age, and functional limitations have been reported to be factors associated with depression in RA patients34. Depression is generally associated with the severe form of RA35. In a meta-analysis, Zhang et al.33 determined higher disease activity and lower quality of life in RA patients with depression compared to those without depression37. In addition, Watad et al.38 found higher levels of anxiety in RA patients compared to a control group, and low socioeconomic status was reported to be an independent factor associated with anxiety. In another study, low socioeconomic status and high DAS28 scores were determined to be associated with anxiety36. Our results are in line with previous studies which showed that individuals diagnosed with RA who also experienced depression and anxiety displayed higher levels of disease activity and lower quality of life compared to RA patients without, but no difference was determined concerning pain.
In our study, when bDMARD and csDMARD users were compared, no statistically significant difference was found in terms of anxiety and depression. However, we noticed a substantial variation in patients' DAS28 and HAQ scores and the presence of depression and anxiety. Similarly, in another study, bDMARDs and csDMARDs were not superior in depression36. More research is needed to investigate the impact of bDMARDs on anxiety and depression. A study of 464 RA patients found that depression was associated with the global health score, while anxiety was associated with being married and having a functional disability39. In another study, it was reported that the presence of anxiety and depression in patients with RA can cause suicide and diminished quality of life and can worsen the prognosis of RA40. The study had some limitations, including a relatively small sample size, and a cross-sectional design. Additionally, there was no control group in the study, and the patients' social and economic situation was not investigated. Since in just four rehabilitation centers, the results may not be generalizable to all RA patients.
Conclusion
Anxiety and depression are highly prevalent among (RA) patients, and it is important to consider that this may impact the patients’ response to treatment, prognosis, and even mortality. Therefore, it is recommended to collaborate with the psychiatry department in managing these cases.
Data availability
The original contributions presented in the study are included in the article, further inquiries can be directed to the corresponding author.
References
Bruce, T. O. Comorbid depression in rheumatoid arthritis: Pathophysiology and clinical implications. Curr. Psychiatry Rep. 10(3), 258–264. https://doi.org/10.1007/s11920-008-0042-1 (2008).
Machin, A., Hider, S., Dale, N. & Chew-Graham, C. Improving recognition of anxiety and depression in rheumatoid arthritis: A qualitative study in a community clinic. Br. J. Gen. Pract. J. R. Coll. Gen. Pract. 67(661), e531–e537. https://doi.org/10.3399/bjgp17X691877 (2017).
Jacob, L., Rockel, T. & Kostev, K. Depression risk in patients with rheumatoid arthritis in the United Kingdom. Rheumatol. Ther. 4(1), 195–200. https://doi.org/10.1007/s40744-017-0058-2 (2017).
Mattey, D. L., Dawes, P. T., Hassell, A. B., Brownfield, A. & Packham, J. C. Effect of psychological distress on continuation of anti-tumor necrosis factor therapy in patients with rheumatoid arthritis. J. Rheumatol. 37(10), 2021–2024. https://doi.org/10.3899/jrheum.100050 (2010).
Li, X., Gignac, M. A. M. & Anis, A. H. The indirect costs of arthritis resulting from unemployment, reduced performance, and occupational changes while at work. Med. Care 44(4), 304–310. https://doi.org/10.1097/01.mlr.0000204257.25875.04 (2006).
Ang, D. C., Choi, H., Kroenke, K. & Wolfe, F. Comorbid depression is an independent risk factor for mortality in patients with rheumatoid arthritis. J. Rheumatol. 32(6), 1013–1019 (2005).
Ho, R. C. M., Fu, E. H. Y., Chua, A. N. C., Cheak, A. A. C. & Mak, A. Clinical and psychosocial factors associated with depression and anxiety in Singaporean patients with rheumatoid arthritis. Int. J. Rheum. Dis. 14(1), 37–47. https://doi.org/10.1111/j.1756-185X.2010.01591.x (2011).
Więdłocha, M. et al. Effect of antidepressant treatment on peripheral inflammation markers—A meta-analysis. Prog. Neuropsychopharmacol. Biol. Psychiatry 80(Pt C), 217–226. https://doi.org/10.1016/j.pnpbp.2017.04.026 (2018).
Chaichian, Y., Genovese, M. C. & Weisman, M. H. The road to rheumatoid arthritis prevention: Challenges and opportunities. Clin. Rheumatol. 39(5), 1379–1381. https://doi.org/10.1007/s10067-020-05016-4 (2020).
O’Neil, L. J. & Deane, K. D. Striking a balance in rheumatoid arthritis prevention trials. Nat. Rev. Rheumatol. 17(7), 385–386. https://doi.org/10.1038/s41584-021-00627-w (2021).
Van der Helm-van Mil, A. H. M. Preventive interventions in individuals at risk for rheumatoid arthritis: State of the art and perspectives. Jt. Bone Spine 90(4), 105543. https://doi.org/10.1016/j.jbspin.2023.105543 (2023).
Kojima, M. et al. Depression, inflammation, and pain in patients with rheumatoid arthritis. Arthritis Rheum. 61(8), 1018–1024. https://doi.org/10.1002/art.24647 (2009).
Kekow, J. et al. Improvements in patient-reported outcomes, symptoms of depression and anxiety, and their association with clinical remission among patients with moderate-to-severe active early rheumatoid arthritis. Rheumatology (Oxford) 50(2), 401–409. https://doi.org/10.1093/rheumatology/keq327 (2011).
DiMatteo, M. R., Lepper, H. S. & Croghan, T. W. Depression is a risk factor for noncompliance with medical treatment: Meta-analysis of the effects of anxiety and depression on patient adherence. Arch. Intern. Med. 160(14), 2101–2107. https://doi.org/10.1001/archinte.160.14.2101 (2000).
Matcham, F., Rayner, L., Steer, S. & Hotopf, M. The prevalence of depression in rheumatoid arthritis: A systematic review and meta-analysis. Rheumatology (Oxford) 52(12), 2136–2148. https://doi.org/10.1093/rheumatology/ket169 (2013).
Marrie, R. A. et al. Increased burden of psychiatric disorders in rheumatoid arthritis. Arthritis Care Res. (Hoboken) 70(7), 970–978. https://doi.org/10.1002/acr.23539 (2018).
Matcham, F. et al. The impact of rheumatoid arthritis on quality-of-life assessed using the SF-36: A systematic review and meta-analysis. Semin. Arthritis Rheum. 44(2), 123–130. https://doi.org/10.1016/j.semarthrit.2014.05.001 (2014).
Evers, A. W. M. et al. Does stress affect the joints? Daily stressors, stress vulnerability, immune and HPA axis activity, and short-term disease and symptom fluctuations in rheumatoid arthritis. Ann. Rheum. Dis. 73(9), 1683–1688. https://doi.org/10.1136/annrheumdis-2012-203143 (2014).
Kay, J. & Upchurch, K. S. ACR/EULAR 2010 rheumatoid arthritis classification criteria. Rheumatology (Oxford) 51(Suppl 6), vi5-9. https://doi.org/10.1093/rheumatology/kes279 (2012).
Zigmond, A. S. & Snaith, R. P. The hospital anxiety and depression scale. Acta Psychiatr. Scand. 67(6), 361–370. https://doi.org/10.1111/j.1600-0447.1983.tb09716.x (1983).
Terkawi, A. S. et al. Development and validation of Arabic version of the hospital anxiety and depression scale. Saudi J. Anaesth. 11(Suppl 1), S11–S18. https://doi.org/10.4103/sja.SJA_43_17 (2017).
Wells, G. et al. Validation of the 28-joint disease activity score (DAS28) and European league against rheumatism response criteria based on C-reactive protein against disease progression in patients with rheumatoid arthritis, and comparison with the DAS28 based on erythrocyte sedimentation rate. Ann. Rheum. Dis. 68(6), 954–960. https://doi.org/10.1136/ard.2007.084459 (2009).
Shehab, D., Al-Jarallah, K. & Moussa, M. A. Validation of the Arabic version of the health assessment questionnaire (HAQ) in patients with rheumatoid arthritis. Rev. Rhum. Engl. Ed. 65(6), 387–392 (1998).
Naaman, R., El-Housseiny, A., Alamoudi, N., Helal, N. & Sahhaf, R. Reliability and validity of the Arabic version of a questionnaire assessing pain, discomfort and related jaw function impairment after extraction of primary teeth in children. Dent. J. https://doi.org/10.3390/dj8040120 (2020).
Wolfe, F., Michaud, K. & Li, T. Sleep disturbance in patients with rheumatoid arthritis: Evaluation by medical outcomes study and visual analog sleep scales. J. Rheumatol. 33(10), 1942–1951 (2006).
Katz, P. Fatigue in rheumatoid arthritis. Curr. Rheumatol. Rep. 19(5), 25. https://doi.org/10.1007/s11926-017-0649-5 (2017).
Inceoğlu, L. A., Bingöl, Ü., Sağirkaya, Z., Sarandöl, A. and Yurtkuran, D. Romatoid artritli hastalarda anksiyete ve depresyon. https://api.semanticscholar.org/CorpusID:78523446 (2004).
Isik, A., Koca, S. S., Ozturk, A. & Mermi, O. Anxiety and depression in patients with rheumatoid arthritis. Clin. Rheumatol. 26(6), 872–878. https://doi.org/10.1007/s10067-006-0407-y (2007).
Fu, X. et al. The prevalence of depression in rheumatoid arthritis in China: A systematic review. Oncotarget 8(32), 53623–53630. https://doi.org/10.18632/oncotarget.17323 (2017).
Morf, H., da Rocha Castelar-Pinheiro, G., Vargas-Santos, A. B., Baerwald, C. & Seifert, O. Impact of clinical and psychological factors associated with depression in patients with rheumatoid arthritis: Comparative study between Germany and Brazil. Clin. Rheumatol. 40(5), 1779–1787. https://doi.org/10.1007/s10067-020-05470-0 (2021).
Pezzato, S. et al. Depression is associated with increased disease activity and higher disability in a large Italian cohort of patients with rheumatoid arthritis. Adv. Rheumatol. (Lond., Engl.) 61(1), 57. https://doi.org/10.1186/s42358-021-00214-3 (2021).
Vallerand, I. A. et al. Depression as a risk factor for the development of rheumatoid arthritis: A population-based cohort study. RMD Open 4(2), e000670. https://doi.org/10.1136/rmdopen-2018-000670 (2018).
Fakra, E. & Marotte, H. Rheumatoid arthritis and depression. Jt. Bone Spine 88(5), 105200. https://doi.org/10.1016/j.jbspin.2021.105200 (2021).
Ng, K.-J. et al. Risk factors, including different biologics, associated with depression and anxiety in patients with rheumatoid arthritis: A cross-sectional observational study. Clin. Rheumatol. 39(3), 737–746. https://doi.org/10.1007/s10067-019-04820-x (2020).
Matcham, F. et al. The relationship between depression and biologic treatment response in rheumatoid arthritis: An analysis of the British Society for Rheumatology Biologics Register. Rheumatology (Oxford) 57(5), 835–843. https://doi.org/10.1093/rheumatology/kex528 (2018).
Fragoulis, G. E. et al. Depression and anxiety in an early rheumatoid arthritis inception cohort. Associations with demographic, socioeconomic and disease features. RMD Open https://doi.org/10.1136/rmdopen-2020-001376 (2020).
Zhang, L., Cai, P. & Zhu, W. Depression has an impact on disease activity and health-related quality of life in rheumatoid arthritis: A systematic review and meta-analysis. Int. J. Rheum. Dis. 23(3), 285–293. https://doi.org/10.1111/1756-185X.13774 (2020).
Watad, A. et al. Anxiety disorder among rheumatoid arthritis patients: Insights from real-life data. J. Affect. Disord. 213, 30–34. https://doi.org/10.1016/j.jad.2017.02.007 (2017).
Katchamart, W., Narongroeknawin, P., Chanapai, W., Thaweeratthakul, P. & Srisomnuek, A. Prevalence of and factors associated with depression and anxiety in patients with rheumatoid arthritis: A multicenter prospective cross-sectional study. Int. J. Rheum. Dis. 23(3), 302–308. https://doi.org/10.1111/1756-185X.13781 (2020).
Godha, D., Shi, L. & Mavronicolas, H. Association between tendency towards depression and severity of rheumatoid arthritis from a national representative sample: The Medical Expenditure Panel Survey. Curr. Med. Res. Opin. 26(7), 1685–1690. https://doi.org/10.1185/03007991003795808 (2010).
Author information
Authors and Affiliations
Contributions
FAK critically revised the manuscript and supervised all the course of the study; YAK wrote the initial draft of the manuscript provided language help, and critically revised the manuscript; BME co-initiated the study and critically revised the manuscript providing language help and proofreading the article.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Khadour, F.A., Khadour, Y.A. & Ebrahem, B.M. A qualitative survey on factors affecting depression and anxiety in patients with rheumatoid arthritis: a cross-sectional study in Syria. Sci Rep 14, 11513 (2024). https://doi.org/10.1038/s41598-024-61523-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-61523-3
Keywords
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.