Abstract
This study aimed to reveal the relationship between eating behavior and nonalcoholic fatty liver disease (NAFLD)/metabolic dysfunction-associated steatotic liver disease (MASLD) in young adults and suggest a questionnaire for eating behavior assessment. We included 322 male graduate students at Gifu University. Diagnoses of NAFLD and MASLD were based on the presence of hepatic steatosis on ultrasonography. Eating behavior was assessed using the eating behavior questionnaire (EBQ) recommended by the Japan Society for the Study of Obesity. We assessed the eating behaviors associated with NAFLD and MASLD using logistic regression, decision tree, and random forest analyses. The median age of the participants was 22 years, and 16% and 11% had NAFLD and MASLD, respectively. The EBQ total score was significantly higher in participants with MASLD than in those without MASLD (102 vs. 90 points, P = 0.006) and in those with NAFLD than in those without NAFLD (97 vs. 90 points, P = 0.007). Among eating behavior categories, the decision tree and random forest analyses revealed that “perception of constitution and weight” was the strongest contributor for NAFLD/MASLD. Our study revealed that eating behavior assessed with the EBQ is robustly associated with NAFLD and MASLD in young male adults.
Similar content being viewed by others

Introduction
Owing to the increasing prevalence of obesity, type 2 diabetes, and metabolic syndrome, the causes and burden of liver cirrhosis are dramatically changing1. Viral hepatitis remains an important cause of cirrhosis. However, increasing vaccination coverage and effective antivirals have contributed to improved death rates due to hepatitis B-associated cirrhosis2. Furthermore, effective, directly acting antivirals have revolutionized the treatment of hepatitis C, and the burden in patients with hepatitis C is forecasted to improve3. In contrast, nonalcoholic fatty liver disease (NAFLD) and nonalcoholic steatohepatitis are rapidly growing etiologies of liver cirrhosis, which lead to decompensation, liver cancer, and mortality4. Recently, a panel of international experts proposed metabolic dysfunction-associated steatotic liver disease (MASLD) as a new term for fatty liver disease5,6. The definition of MASLD is based on the risk profiles of NAFLD; accordingly, MASLD is expected to better identify patients at high risk for disease burden of chronic liver disease than NAFLD. Therefore, more efforts are required for the early prevention, detection, and intervention of NAFLD and MASLD to improve outcomes.
Lifestyle modifications consisting of a healthy diet and regular exercise form the foundation for the treatment of patients with NAFLD and MASLD7,8,9,10. However, it is difficult to achieve lifestyle modification in patients with NAFLD because some patients are not in the active phase of lifestyle modification11. Behavioral therapy is an important component of lifestyle modification based on learning theory, which assumes that behaviors that result in obesity have a strong educational component and, therefore, can be modified or relearned12. Given its effect on treatment outcomes, major guidelines recommend behavioral interventions, including motivational interviewing, stimulus control, cognitive restriction, and self-monitoring, for the treatment of obesity13. The Japan Society for the Study of Obesity suggested an eating behavior questionnaire (EBQ) as an initial step in assessing eating behavior and providing effective behavioral therapy for patients with obesity14. However, very few attempts have been made to assess eating behavior and behavioral therapy in patients with NAFLD/MASLD.
The primary aim of this study was to evaluate the association between eating behavior and NAFLD/MASLD among Japanese male young adults. The secondary aim was to develop a useful EBQ to stratify the risk of NAFLD/MASLD among young Japanese male adults.
Methods
Study design and participants
This cross-sectional study included 322 male graduate students who enrolled at Gifu University (Gifu, Japan) and underwent health checkups for new students in April 2022 (Supplementary Fig. S1). The exclusion criteria included severe comorbidities and international students. Given the limit for alcohol consumption in the diagnosis of NAFLD/MASLD, participants with an alcohol intake > 30 g/day were also excluded from the study5,6,7,8,9. The study aims were explained to the candidates and written informed consent was obtained from all participants. The study protocol was reviewed and approved by the Institutional Review Board of the Graduate Medical School, Gifu University (approval no. 2021-B167), and conformed to the provisions of the Declaration of Helsinki (as revised in Fortaleza, Brazil, October 2013).
Clinical and biochemical characteristics
Clinical and biochemical characteristics were assessed using health checkup data. Mild alcohol intake was defined as an alcohol intake permitted within the diagnosis of NAFLD/MASLD (≤ 30 g/day)5,6,7,8,9. Laboratory data assessed included aspartate aminotransferase (AST), alanine aminotransferase (ALT), triglycerides, high-density lipoprotein (HDL) cholesterol, low-density lipoprotein cholesterol, hemoglobin A1c (HbA1c), and fasting or casual glucose levels.
Diagnosis of NAFLD and MASLD
Hepatic steatosis was evaluated using liver ultrasound (CX50; Koninklijke Philips N.V., Amsterdam, Netherlands) performed by a single hepatologist blinded to the laboratory data. Participants with hepatic steatosis without other liver diseases, such as alcohol-related liver disease (alcohol intake > 30 g/day), viral liver disease, or drug-induced liver disease, were diagnosed with NAFLD8,9. MASLD was diagnosed in participants with hepatic steatosis who met at least one of the following cardiometabolic criteria: overweight (body mass index [BMI] ≥ 23 kg/m2 or waist circumference > 94 cm); impaired glucose tolerance (fasting blood glucose ≥ 100 mg/dL, occasional blood glucose ≥ 140 mg/dL, HbA1c ≥ 5.7%, type 2 diabetes mellitus, or treatment with antidiabetic medicine); hypertension (blood pressure ≥ 130/85 mmHg); hypertriglyceridemia (triglyceride level ≥ 150 mg/dL); low HDL cholesterol (< 40 mg/dL); or received any treatment related to these conditions5,6.
Assessment of eating behavior questionnaire
An EBQ recommended by the Japan Society for the Study of Obesity was administered at the time of health checkups14. The questionnaire consisted of 55 items and participants were asked to answer each item with the following scales: “not at all like me” (one point), “sometimes like me” (two points), “tendency like me” (three points), and “extremely like me” (four points) (Supplementary Table S1). Eating behavior was assessed by summarizing the score of each item into seven categories: (1) perception of constitution and weight, (2) motivation for eating, (3) eating as diversion, (4) feeling of fullness and hunger, (5) bad eating habits, (6) contents of meals, and (7) unsteady eating pattern. The subtotal scores of all categories were summarized as total scores (Supplementary Table S2). A higher score in each category and total score indicated worse eating behavior. An octagonal diagram was created using the score for each category as a percentage14.
Objectives
The primary objective of this study was to examine the association between the EBQ total score and presence of NAFLD/MASLD to reveal the relationship between eating behavior and NAFLD/MASLD among Japanese male young adults. The secondary objective was to explore the association between each EBQ category and the presence of NAFLD/MASLD to clarify the characteristics of eating behavior associated with NAFLD/MASLD among young Japanese male adults.
Statistical analyses
Continuous variables are expressed as medians and interquartile ranges. Categorical variables are expressed as numbers and percentages (%). Groups were compared using the Mann–Whitney U test or chi-square test. The association between eating behavior and NAFLD/MASLD was assessed using logistic regression analysis. The results are presented as odds ratios (OR) and 95% confidence intervals (CI). The discriminative ability of the EBQ to identify NAFLD/MASLD was assessed using receiver operating characteristic (ROC) curve analysis, shown as the area under the curve (AUC), and the optimal cutoff value was identified using the Youden’s index. A restricted cubic spline (RCS) model with three knots was evaluated to demonstrate the association between the EBQ scores and NAFLD/MASLD15. The reference point of the EBQ total score was manually adjusted to 90 points considering the median value of the EBQ total score, and the bin width was set to two points. Multivariate analysis, including all categories of the EBQ, was performed to determine the strongest eating behavior category for MASLD and NAFLD. The decision tree analysis was performed to identify eating behavior that classifies MASLD and NAFLD16. Random forest analysis was performed to identify eating behaviors that contributed to MASLD and NAFLD, expressed as variable importance values16. All tests were two-sided, and P < 0.05 was set as the threshold for statistical significance. All statistical analyses were performed using JMP (version 16.2.0, SAS Institute Inc., Cary, NC, USA) and R (version 4.3.1, R Foundation for Statistical Computing, Vienna, Austria).
Results
Characteristics of study participants
The participants’ characteristics are listed in Table 1. Of the 322 participants, the median age was 22 years, and 8%, 36%, and 40% reported current or former smoking habits, mild alcohol consumption, and exercise habits, respectively. The median waist circumference and BMI were 76 cm and 20.7 kg/m2, respectively. Regarding the cardiometabolic criteria, the prevalence of overweight (BMI ≥ 23 kg/m2), impaired glucose tolerance, hypertension, hypertriglyceridemia, and low HDL cholesterol were 22%, 2%, 24%, 16%, and 4%, respectively. Of the 322 participants, 17% (n = 54) were diagnosed with hepatic steatosis by ultrasound. MASLD and NAFLD were diagnosed in 11% (n = 36) and 16% (n = 54) of participants, respectively; of these, 11% (n = 36) had both MASLD and NAFLD (Supplementary Fig. S2).
Impact of eating behavior on MASLD and NAFLD in Japanese male young adults
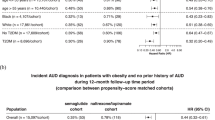
A comparison of eating behavior scores between participants with and without MASLD or NAFLD is shown in Table 2. Participants with MASLD had significantly higher EBQ total scores than those without MASLD (102 vs. 90 points; P = 0.009). The RCS models demonstrated that the risk of MASLD (Fig. 1a) and NAFLD (Fig. 1b) increased as the EBQ total score elevated. The ROC curve analysis identified a EBQ total score > 100 points as an optimal cutoff value to identify MASLD (AUC, 0.63), with sensitivity and specificity of 0.53 and 0.70, respectively. In the same manner, the ROC curve analysis identified a EBQ total score > 82 points as an optimal cutoff value to identify NAFLD (AUC, 0.62), with sensitivity and specificity of 0.83 and 0.34, respectively. In each category, participants with MASLD had significantly higher scores for “perception of constitution and weight” (15 vs. 13 points; P < 0.001) and “bad eating habits” (12 vs. 9 points; P = 0.002) compared to those without MASLD (Fig. 2a). Similarly, participants with NAFLD had significantly higher EBQ total scores than those without NAFLD (97 vs. 90 points; P = 0.007). In each category, participants with NAFLD had significantly higher scores in “perception of constitution and weight” (15 vs. 13 points; P < 0.001), “motivation for eating” (19 vs. 18 points; P = 0.044), and “bad eating habits” (11 vs. 9 points; P = 0.006) compared to those without NAFLD (Fig. 2b). Subgroup analyses revealed that participants with both NAFLD and MASLD had significantly higher EBQ total scores than those without NAFLD/MASLD (102 vs. 90 points; P = 0.022), while there was no statistical difference between participants with only NAFLD and those without NAFLD/MASLD (92 vs. 90 points; P = 0.915) (Supplementary Fig. S3).
Age-adjusted odds ratio for the association between (a) MASLD, (b) NAFLD, and EBQ total score. The analyses were performed using the multivariate logistic regression models with restricted cubic spline with three knots and the reference points were manually adjusted. EBQ eating behavior questionnaire, MASLD metabolic dysfunction-associated steatotic liver disease, NAFLD nonalcoholic fatty liver disease.
Multivariate logistic regression analyses revealed that “perception of constitution and weight” (OR 1.21; 95% CI 1.08–1.35; P = 0.001) and “bad eating habits” (OR 1.18; 95% CI 1.00–1.28; P = 0.045) were independently associated with MASLD, and only “perception of constitution and weight” was associated with NAFLD (OR 1.20; 95% CI 1.09–1.33; P < 0.001) (Table 3).
Data-mining analyses for eating behavior on MASLD and NAFLD
Decision tree and random forest analyses, including all eating behavior categories, were performed to explore the association between eating behavior and MASLD and NAFLD. The decision-tree analysis revealed that the strongest classifier of MASLD and NAFLD was “perception of constitution and weight.” Participants with ≥ 12 points in “perception of constitution and weight” had a higher prevalence of MASLD than those with < 12 points (16 vs. 2%: Fig. 3a). Similarly, participants with ≥ 11 points in “perception of constitution and weight” had higher prevalence of NAFLD than those with < 11 points (21 vs. 4%: Fig. 3b). Random forest analyses demonstrated that “perception of constitution and weight” was the strongest category contributing to MASLD and NAFLD with variable importance of 23.8 and 26.6, respectively (Fig. 3c,d).
Data-mining analyses for eating behavior and MASLD and NAFLD in Japanese male young adults. The decision tree analyses revealed that “perception of constitution and weight” is the strongest classifier for (a) MASLD and (b) NAFLD. The random forest analyses revealed that “perception of constitution and weight” is the most important contributor to (c) MASLD and (d) NAFLD. MASLD metabolic dysfunction-associated steatotic liver disease, NAFLD nonalcoholic fatty liver disease.
Data-mining analyses for eating behavior questionnaire items on MASLD and NAFLD
Decision tree and random forest analyses, including all EBQ items, were performed to explore the association between questionnaire items and MASLD and NAFLD. The decision-tree analysis revealed that the strongest item associated with MASLD and NAFLD was item no. 42; “I believe I easily gain weight than others.” Participants with ≥ 2 points for item 42 had a higher prevalence of MASLD than those with < 2 points (21 vs. 4%). Similarly, participants with ≥ 2 points for item 42 had a higher prevalence of NAFLD than those with < 2 points (30 vs. 7%) (Supplementary Fig. S4). Random forest analyses also confirmed that item 42 was the strongest EBQ item contributing to MASLD and NAFLD, with a variable importance of 18.2 and 21.8, respectively (Supplementary Fig. S5).
Discussion
The present study found that eating behavior is strongly associated with NAFLD/MASLD. Obesity can occur due to a false perception of eating habits, actual dietary consumption, and unfavorable eating habits. For instance, some patients may think that they gain body weight even by drinking water, which is a gap in the recognition of constitution and weight, and some patients may insufficiently chew food, which is a bad eating habit14. The EBQ was originally developed to evaluate unaware gaps and habits in eating behaviors, especially in obese patients14. Since behavior therapy can improve adherence to lifestyle interventions for obesity17, several guidelines for obesity treatment have emphasized the importance of behavior therapy in patients with obesity13. However, few attempts have been made to develop behavioral therapies for the treatment of NAFLD/MASLD. We hypothesized that eating behavior can affect NAFLD/MASLD and that the EBQ can be an effective modality for evaluating eating behavior among those with NAFLD/MASLD. In our study, we assessed both NAFLD and MASLD to strengthen current evidence regarding MASLD, given it is newly defined, and little relevant evidence is available to date. In addition, the association between the EBQ scores and steatotic liver disease has not been well-investigated even in the context of NAFLD.
The first intriguing finding of the present study was that eating behavior was significantly worse in participants with NAFLD/MASLD than in those without NAFLD/MASLD. The second intriguing finding of the present study was that the influence of eating behavior on MASLD was stronger than that on NAFLD. The results of the present study expand our knowledge of the pathophysiology of NAFLD/MASLD and provide an important perspective for the multidisciplinary treatment of patients with NAFLD/MASLD.
Our study showed a significant difference in eating behaviors between participants with and without NAFLD/MASLD. In previous studies, the EBQ total score was higher in obese patients than in non-obese patients and was associated with actual food consumption18,19. Our study revealed that young Japanese male adults with NAFLD/MASLD had significantly higher EBQ total scores than those without NAFLD/MASLD. As for eating behavior category, decision tree and random forest analyses revealed that “perception of constitution and weight” was the strongest contributor for NAFLD/MASLD. The robust association between “perception of constitution and weight” and NAFLD/MASLD can be explained by a prior study that demonstrated that “perception of constitution and weight” was strongly correlated with BMI (r = 0.41)18, which can stratify the risk of NAFLD/MASLD20. In fact, BMI also correlated with the EBQ total score (r = 0.31) and “perception of constitution and weight” (r = 0.47) in our study. The initial approach to behavioral therapy varies according to each patient’s problematic eating behavior; therefore, physicians should evaluate eating behavior and adopt individualized behavior therapy to improve adherence to lifestyle modifications in patients with NAFLD/MASLD12. Since the EBO has good internal reliability (coefficient alpha = 0.81)18, the novelty of our findings should be emphasized in that assessment of eating behavior using the EBQ can be a basic approach to initiating behavior therapy in young adults with NAFLD/MASLD.
The second finding of our study was that the effect of eating behavior on MASLD was stronger than that on NAFLD. Based on the subgroup analyses categorized by NAFLD and MASLD, individuals with both conditions exhibited a higher EBQ total score than those without either condition, while no statistical difference was observed between individuals with only NAFLD and those without either condition. In addition, multivariate logistic regression analysis revealed that two categories of eating behavior, “perception of constitution and weight” and “bad eating habits,” were independently associated with MASLD, whereas only one category, “perception of constitution and weight,” was associated with NAFLD. Since eating behavior can lead to obesity, our results provide a reasonable explanation for the fact that patients with metabolic dysfunction-associated fatty liver disease—the diagnosis of which includes risk factors for NAFLD—have a higher risk of obesity, fibrosis, cardiovascular disease, and mortality than those with NAFLD21,22,23. Therefore, the assessment of eating behavior can be a useful strategy to identify individuals at high risk of MASLD who require early detection and intervention, especially at a younger age.
An additional finding of our study was that we identified an effective question item to stratify the risk of NAFLD/MASLD. Participants who had ≥ 2 points in the question asking that “I believe I easily gain weight than others” had significantly higher prevalence of MASLD and NAFLD than those with < 2 points and the results were confirmed by the data-mining analysis. A recent study has shown that patients with NAFLD have good knowledge of their disease; however, approximately half of patients with NAFLD are not ready for lifestyle modifications, including diet and exercise11. Although participants who had ≥ 2 points in this question may have genetic or constitutional factors that can lead to obesity, our results imply that individuals with NAFLD/MASLD have unfavorable recognition of their constitution, which can limit adherence to lifestyle interventions. Thoughts can influence mood and behavior, and cognitive restructuring can be a useful method to modify an individual’s mindset to promote favorable effects on lifestyle modifications12. In previous studies conducted in Japan, eating behavior, assessed using the EBQ, was robustly associated with obesity and metabolic syndrome24,25. Therefore, recognizing eating behavior in each individual and modifying unfavorable behaviors based on the results of the EBQ can be a useful method to implement effective lifestyle modifications for NAFLD/MASLD prevention or treatment. In addition, since the EBQ has been reported to be useful in monitoring eating behavior26, the questionnaire is also applicable to behavior therapy and monitoring during lifestyle interventions in patients with NAFLD/MASLD.
However, some limitations of this study must be addressed. This was a single-center study that included only young Japanese male adults, and the results may not be applicable to other regions, females, and age groups. Considering the apparent sex differences in obesity, type 2 diabetes mellitus, and other metabolic abnormalities27, we plan to conduct a further investigation including both males and females to extend the findings of our study. Despite these limitations, our study has several strengths, including the use of a young cohort, originality, and application of data mining analysis and has meaningful implications for the association between eating behavior and NAFLD/MASLD among young male adults.
In conclusion, our study adds to the growing evidence that eating behavior is significantly worse in individuals with NAFLD/MASLD than in those without. Eating behavior of those with NAFLD/MASLD is characterized by unfavorable recognition of their constitution and weight. Furthermore, our study provides evidence that the EBQ is useful for behavioral therapy in patients with NAFLD/MASLD. Our study encourages better application of a multidisciplinary approach to maximize the benefit of lifestyle interventions in young adults and reduce the future burden of NAFLD/MASLD.
Data availability
The data analyzed in this study is availabule from the corresponding author on reasonable request.
References
Huang, D. Q. et al. Global epidemiology of cirrhosis: Aetiology, trends and predictions. Nat. Rev. Gastroenterol. Hepatol. 20, 388–398 (2023).
GBD 2019 Hepatitis B Collaborators. Global, regional, and national burden of hepatitis B, 1990–2019: A systematic analysis for the global burden of disease study 2019. Lancet Gastroenterol. Hepatol. 7, 796–829 (2022).
Heffernan, A., Cooke, G. S., Nayagam, S., Thursz, M. & Hallett, T. B. Scaling up prevention and treatment towards the elimination of hepatitis C: A global mathematical model. Lancet 393, 1319–1329 (2019).
Paik, J. M., Golabi, P., Younossi, Y., Mishra, A. & Younossi, Z. M. Changes in the global burden of chronic liver diseases from 2012 to 2017: The growing impact of NAFLD. Hepatology 72, 1605–1616 (2020).
Rinella, M. E. et al. A multi-society Delphi consensus statement on new fatty liver disease nomenclature. J. Hepatol https://doi.org/10.1016/j.jhep.2023.06.003 (2023).
Rinella, M. E. et al. A multi-society Delphi consensus statement on new fatty liver disease nomenclature. Hepatology https://doi.org/10.1097/hep.0000000000000520 (2023).
European Association for the Study of the Liver (EASL), European Association for the Study of Diabetes (EASD) & European Association for the Study of Obesity (EASO). EASL-EASD-EASO clinical practice guidelines for the management of non-alcoholic fatty liver disease. J. Hepatol. 64, 1388–1402 (2016).
Tokushige, K. et al. Evidence-based clinical practice guidelines for nonalcoholic fatty liver disease/nonalcoholic steatohepatitis 2020. Hepatol. Res. 51, 1013–1025 (2021).
Tokushige, K. et al. Evidence-based clinical practice guidelines for nonalcoholic fatty liver disease/nonalcoholic steatohepatitis 2020. J. Gastroenterol. 56, 951–963 (2021).
Rinella, M. E. et al. AASLD practice guidance on the clinical assessment and management of nonalcoholic fatty liver disease. Hepatology 77, 1797–1835 (2023).
Glass, L., Asefa, H., Volk, M., Lok, A. S. & Tincopa, M. A. Disease knowledge, health-related quality of life, and lifestyle behavior change in patients with nonalcoholic fatty liver disease: Impact of an educational intervention. Dig. Dis. Sci. 67, 2123–2133 (2022).
Bellentani, S., Dalle Grave, R., Suppini, A. & Marchesini, G. Behavior therapy for nonalcoholic fatty liver disease: The need for a multidisciplinary approach. Hepatology 47, 746–754 (2008).
Semlitsch, T., Stigler, F. L., Jeitler, K., Horvath, K. & Siebenhofer, A. Management of overweight and obesity in primary care-A systematic overview of international evidence-based guidelines. Obes. Rev. 20, 1218–1230 (2019).
Ohmori, Y. et al. Association of personality (NEO-five factor inventory) with eating behaviors and physical activity levels in obese subjects in the Saku control obesity program (SCOP). Anti-aging Med. 4, 43–50 (2007).
Kwon, Y. J. et al. The association between total protein intake and all-cause mortality in middle aged and older Korean adults with chronic kidney disease. Front. Nutr. 9, 850109 (2022).
Doupe, P., Faghmous, J. & Basu, S. Machine learning for health services researchers. Value Health 22, 808–815 (2019).
Samdal, G. B., Eide, G. E., Barth, T., Williams, G. & Meland, E. Effective behaviour change techniques for physical activity and healthy eating in overweight and obese adults; Systematic review and meta-regression analyses. Int. J. Behav. Nutr. Phys. Act. 14, 42 (2017).
Xia, J., Yang, C., Ge, S., Feng, X. & Sun, W. Eating behavior and hypertension in Chinese. Asia Pac. J. Clin. Nutr. 30, 504–511 (2021).
Takezawa, J. et al. Preproghrelin gene polymorphisms in obese Japanese women. Minor homozygotes are light eaters, do not prefer protein or fat, and apparently have a poor appetite. Appetite. 63, 105–111 (2013).
Tajirika, S. et al. Usefulness of health checkup for screening metabolic dysfunction-associated fatty liver disease and alcohol-related liver disease in Japanese male young adults. Sci. Rep. 13, 7987 (2023).
Miwa, T. et al. Impact of body fat accumulation on metabolic dysfunction-associated fatty liver disease and nonalcoholic fatty liver disease in Japanese male young adults. Hepatol. Res. 53, 691–700 (2023).
Yamamura, S. et al. MAFLD identifies patients with significant hepatic fibrosis better than NAFLD. Liver Int. 40, 3018–3030 (2020).
Nguyen, V. H., Le, M. H., Cheung, R. C. & Nguyen, M. H. Differential clinical characteristics and mortality outcomes in persons with NAFLD and/or MAFLD. Clin. Gastroenterol. Hepatol. 19, 2172-2181.e2176 (2021).
Morita, A., Aiba, N., Miyachi, M. & Watanabe, S. The associations of eating behavior and dietary intake with metabolic syndrome in Japanese: Saku cohort baseline study. J. Physiol. Anthropol. 39, 40 (2020).
Ishida, Y. et al. Influence of the accumulation of unhealthy eating habits on obesity in a general Japanese population: The Hisayama study. Nutrients 12, 3160 (2020).
Miyoshi, R. et al. Weight control in schizophrenic patients through Sakata’s charting of daily weight pattern and its associations with temperament and character. Asian J. Psychiatr. 7, 52–57 (2014).
Cooper, A. J., Gupta, S. R., Moustafa, A. F. & Chao, A. M. Sex/gender differences in obesity prevalence, comorbidities, and treatment. Curr. Obes. Rep. 10, 458–466 (2021).
Acknowledgements
We would like to thank all the medical staff involved in this study.
Funding
This work was supported by the JSPS KAKENHI (grant number JP22K11774) and Taguchi Fukujukai Public Interest Incorporated Foundation.
Author information
Authors and Affiliations
Contributions
The study was concepted and designed by S.T., T.H., M.S., and M.Y.. The data was collected by S.T., T.M., N.I., M.A., R.H., T.F., and M.Y.. The analyses were performed by T.M.. The first draft of the manuscript was written by T.M. and M.Y. critically revised the manuscript. All authors reviewed and approved the final versions of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Miwa, T., Tajirika, S., Hanai, T. et al. Usefulness of a questionnaire for assessing the relationship between eating behavior and steatotic liver disease among Japanese male young adults. Sci Rep 14, 2194 (2024). https://doi.org/10.1038/s41598-024-52797-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-52797-8
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.