Abstract
To determine the readmissions trends and the comorbidities of patients with heart failure that most influence hospital readmission rates. Heart failure (HF) is one of the most prevalent health problems as it causes loss of quality of life and increased health-care costs. Its prevalence increases with age and is a major cause of re-hospitalisation within 30 days after discharge. INCA study had observational and ambispective design, including 4,959 patients from 2000 to 2019, with main diagnosis of HF in Extremadura (Spain). The variables examined were collected from discharge reports. To develop the readmission index, capable of discriminating the population with higher probability of re-hospitalisation, a Competing-risk model was generated. Readmission rate have increased over the period under investigation. The main predictors of readmission were: age, diabetes mellitus, presence of neoplasia, HF without previous hospitalisation, atrial fibrillation, anaemia, previous myocardial infarction, obstructive pulmonary disease (COPD) and chronic kidney disease (CKD). These variables were assigned values with balanced weights, our INCA index showed that the population with values greater than 2 for men and women were more likely to be re-admitted. Previous HF without hospital admission, CKD, and COPD appear to have the greatest effect on readmission. Our index allowed us to identify patients with different risks of readmission.
Similar content being viewed by others
Introduction
Heart failure (HF) is one of the most prevalent health problems in developed countries. Worldwide, it is estimated that 64.3 million people suffer from HF1, with an approximate prevalence between 1 and 2% of the adult population2,3. Despite improvements in the management and treatment of HF in recent years, the percentage of readmissions continues to be high. Currently, HF remains the disease with the highest 30-day readmission rate4.
The prevalence of HF increases with age5. Taking into account that the life expectancy of the global population is increasing and that patients with HF are more susceptible to recurrent hospitalization due to decompensation of their chronic pathologies, the increase in the number of readmissions in recent years6,7 takes on special importance. In a public health context, in addition to the associated reduced quality of life8, it is essential to consider the costs generated by hospital readmissions9,10. Focusing on economic terms, HF generates a considerable burden to the health care system through the combined costs of admission, readmission, nursing staff, and medications. According to a study based in Spain11, the average total annual cost of HF ranges from 12,995 euros to 18,220 euros, depending on the level of severity of the disease and the comorbidities present.
Considering this, methodologically comprehensive studies that can describe the readmission phenomenon as a whole, including an analysis of the presence of comorbidities, are needed. To respond to this need, we aimed to determine the readmissions trends over the years and the comorbidities of patients with HF that most influence hospital readmission rates within one year of discharge by means of an indicator capable of analysing specific factors.
Materials and methods
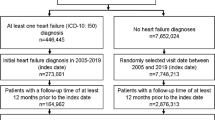
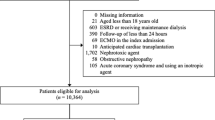
The INCA study12 has an observational and ambispective design. A total of 4,959 individuals, representing all patients with a primary diagnosis of HF at discharge (428 International Classification of Diseases 9th Revision [ICD-9] codes for the period 2000–2015 along with i50.0, i50.1, and i50.9 from the 10th Revision [ICD-10]) during the period 2000–2019 admitted consecutively to the hospital complex of the Don Benito-Villanueva de la Serena Health Area (which initially consisted only of the Don Benito-Villanueva Hospital and, since 2008, also the Siberia-Serena Hospital in Talarrubias), were included. This Health Area has a population of 141,337 inhabitants.
The data were obtained through the Coding and Computing Service of the Hospital Don Benito-Villanueva and the Subdirectorate of Information of the Extremadura Health Service. The information on mortality was obtained by contrasting the hospital base with the National Death Index (INDeF). The ethics committee of the University Hospital of Badajoz approved this study, that was conducted in accordance with the relevant guidelines and regulations.
Variables
The following variables were collected from each of the discharge reports: sex; age; length of stay; presence of peripheral arterial disease (PAD); previous stroke; previous myocardial infarction(MIp); history of HF without hospital admission; comorbidities (neoplasms and chronic obstructive pulmonary disease [COPD] defined as the presence of COPD and/or obstructive sleep apnoea [OSA]); and cardiovascular risk factors (arterial hypertension, diabetes mellitus [DM], and atrial fibrillation [AF]).
Laboratory test results were also consulted. To screen for chronic kidney disease (CKD), the glomerular filtration rate was obtained using the CKD-EPI formula13 with a cut-off of < 45 ml/min/m3. Anaemia14 was screened for using the following haemoglobin cut-offs: < 13 g/dL for men and < 12 g/dL for women.
Hospital readmissions for HF in the first year after discharge were then analysed.
All investigators who participated in the study were trained at the study coordinating centre to ensure the quality of the data.
Statistical analysis
Continuous variables are presented as the mean and standard deviation or median and interquartile range, while categorical variables are presented as the absolute and relative frequency. Differences between the living and the dead were compared using the chi-square test. To construct the hospital readmission, index a Cox proportional hazards model, and then, a competing-risk model15,16 (special type of survival analysis that aims to correctly estimate the marginal probability of an event—readmission- in the presence of competing events—death during the 1 years after discharge) were generated. The patients who died during hospital admission were excluded and only patients discharged alive were assessed.
Although our primary hypotheses concern non-fatal endpoints, mortality is a competing risk in this population. Therefore, significant variables were selected for the composite endpoint of death or readmission in the 1-year post-discharge period.
The model was adjusted for age and only those variables that had an unadjusted association with the occurrence of hospital readmission for HF and a p value < 0.05 were considered for inclusion (i.e., length of hospital stay, DM, neoplasia, MIp, previous HF, moderate valvulopathy, anaemia, COPD, OSAS, CKD).
All analyses were bilateral, and 95% confidence intervals (CIs) were calculated using the bootstrapping analysis with 1,000 replications to ensure model robustness, with IBM SPSS and STATA version 17.
Construction of the indicator
To construct a score and an indicator capable of predicting the risk of readmission due to HF separated by sex, the variables were weighted differently according to the value of the hazard ratio (hazard ratio up to 0.50: 0.5 points, hazard ratio between 0.51 and 1: 1 point). Presence of DM, neoplasia, AF, anaemia and MIp score 0.5 points, while previous HP, CKD and COPD/OSAS score 1 point.
The model was then adjusted for age (> 75 years: 0.5 points, < 75 years: 0 points.
Ethics approval
Approval was obtained from the ethics committee of University Hospital of Badajoz.
Consent to participate
Informed consent was obtained from legal guardians.
Results
A total of 4,959 patients admitted between January 1, 2000 and December 31, 2019 were included in the INCA study. Those who died in hospital readmissions (n = 473) were excluded, leaving 4,486 patients who were followed up. The average age was 77.21 (± 10.40), and 53.8% (n = 2,414) were women.
The overall readmission rate of patients with a diagnosis of HF in the first year after discharge was 27.3%. Table 1 shows the increase in the readmission rate over the 20-year follow-up period grouped into 5-year periods. An upward trend in the rate of readmissions, especially 30-day readmissions, were seen. During the period from 2015 to 2019, the rate of readmissions had doubled the initial percentage.
The results of the Competing-risk model are presented in Table 2. The following variables were predictors of readmission in the first year: age, DM, presence of neoplasms, HF without hospital admission, AF, anaemia, MIp, COPD, CKD.
Then, was constructed the INCA score using the values and procedures specified in the methodology section. Based on the scores of these 4,486 study participants (Table 3), the threshold represented by 2 points in men and women appears to be where the percentage of participants readmitted is consistently higher than that of participants who are not readmitted, thus creating two distinct populations with a different probability of readmission. Pearson’s chi-square significance was determined to be 0.001.
Discussion
Main findings
Our study shows that the readmission rate of patients with HF increased steadily over this 20-year period, with the greatest burden in the first 30 days after discharge.
Predictors of readmission for both sexes were as follows: a history of CKD, COPD, and previous HF without hospitalization. We propose a risk score that can facilitate the identification of patients who are likely to suffer from it.
Since our study consecutively included patients with a diagnosis of decompensated HF over a 20-year period, the results are considered representative of the study area. The INCA study is comparable with other international “real world” studies17,18 that differ from clinical trials19,20 and exclusive registries from cardiology services21,22 in that they register at least 50% women, include populations that are older, and those with a high rate of comorbidity.
Analysis of the population and readmissions at one month, six months, and one year
Table 4 shows the percentage of readmissions at 30 days, six months, and one year reported in the INCA study and other international studies. To date, the need for a clear separation by risk of readmissions, according to these three periods, has not been addressed. The information provided in this study suggests that readmissions at one month and one year may be motivated by different causes. While the former is usually related to treatment imbalances or early discharge, readmission after six months or one year are usually due to poor adherence to treatment19, lack of follow-up after discharge, or the natural progression and severity of the disease.
The results of our study are consistent with other previous studies, most notably the study by Martinez-Santos23, which analysed all admissions of patients with a diagnosis of HF at discharge registered in Spain between January 1, 2012 and December 31, 2012. The differences found could be attributed to an older population.
The readmission rates presented in the INCA study are lower than those reported in the Omersa study24. This could be explained by a difference in the inclusion criteria and creation of the sample since the INCA study considered only some of the ICD-10 codes that were used in the Omersa study.
What is already known
INCA score and analysis of other indicators
Several studies25,26,27 have reported predictive models for HF readmissions. Detecting patients at discharge that are most likely to be readmitted would allow for specific attention and resources to be offered that could help prevent readmission. Despite this, these predictive models are rarely used in clinical practice.
Our literature review suggests that, besides the few existing indicators, the field remains open, with no univocal process capable of stratifying patients according to risk28.
One of the criticisms of the studies underlying the creation of indicators is that the data often come from clinical trials, which do not represent the HF population as a whole29. However, for the INCA score, patients admitted for HF were included consecutively (excluding none) and thus, real-life data was provided.
The INCA score allows for an analysis of the comorbidities that most influence hospital readmission within one year in an attempt to distinguish patients who are at high risk. The expectation is that one-month readmissions can be reduced through the early implementation of appropriate follow-up approaches, both from a medical and nursing point of view30.
In our study, the relevant variables were the presence of previous HF without hospital admission, CKD, and COPD. These findings are consistent with previous studies31,32,33,34 that found an association between these comorbidities and an increased risk of readmission, suggesting that they may be reliable markers of a worse prognosis.
The predictor variables of the INCA score are consistent with the results of a recent literature review35 and other studies, such as the Omersa study24, which found that presence of MIp, neoplasia, DM, and renal failure increase the probability of hospital readmission. The Optimize-HF registry19 also describes a strong association between these comorbidities and a worse prognosis (though it also includes AF, worsening renal function, deterioration of respiratory function, and poor adherence to treatment and diet as precipitating factors).
The value of HF scores
In 2015, Spanish researchers developed the REDIN score25 with specific models designed to predict 30-day and 1-year readmissions. While this score includes typical HF variables, the study population was mostly men (69%) and the mean age was 66.7 years, which differs from real-world values and could negatively influence the correct application of the score.
Other scores, such as the HFPI26, developed by the University of Michigan, and the RR27, developed by the Yale New Haven Health Services Corporation/Center for Outcomes Research and Evaluation (YNHHSC/CORE), include analyses of readmissions. The former analyses readmissions over six months, while the latter analyses readmissions within one month of discharge. However, both scores analyse all-cause readmissions, whereas the INCA score only records readmissions for HF, and thus offers the opportunity to analyse a specific population.
What this study adds
The INCA score is a simple-to-use indicator that offers healthcare personnel the opportunity to separate patients into two populations with different levels of risk, and to offer differentiated follow-up plans tailored to the control of HF and comorbidities in an attempt to reduce readmissions for HF. The most effective measures to prevent hospital readmissions will likely result from personalized follow-up based on multidisciplinary management programs, education on self-care strategies, and systematic periodic follow-ups in consultation and at home36.
In short, the INCA score is an indicator built on "real world" data that takes into account an elderly population with many comorbidities and adequately represents the female gender.
Limitations and strengths
This study has the typical limitations of a retrospective study. We attempted to control for variability between the different variables through employing appropriately trained qualified personnel. The moderate number of echocardiograms and the information provided by hospital discharges led us to reject the inclusion of left ventricular systolic function in the analysis, as well as the lack of routine determination of BNP or data on the physical or cognitive abilities of the patients. which would have been of prognostic interest. Another limitation is the lack of follow-up on medication adherence, which may have contributed to patient readmission, and the lack of information on major psychiatric disorders or inflammatory diseases (in both cases, frequency or consistency of clinical history was very low).
The strengths of this study include the large number of included patients, the consecutive nature of inclusion, the ease of use of the indicator and the use of “real world” data to construct the indicator.
Conclusion
In the first two decades of the twenty-first century, readmissions for HF have increased significantly. Among all the variables assessed, a history of HF without hospital admission, CKD, and COPD appear to have the greatest effect on readmission. Using the INCA score, comorbidities can be assessed, and patients can be separated into two groups based on readmission risk, allowing for those who require more careful assessment and follow-up to be identified.
Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Collaborators, G. B. Global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories, 1990–2017: a systematic analysis for the global burden of disease study. Lancet 392, 1789–1858 (2018).
Loehr, L. R., Rosamond, W. D., Chang, P. P., Folsom, A. R. & Chambless, L. E. Heart failure incidence and survival (from the atherosclerosis risk in communities study). Am. J. Cardiol. 101, 1016–1022 (2008).
Groenewegen, A., Rutten, F. H., Mosterd, A. & Hoes, A. W. Epidemiology of heart failure. Eur. J. Heart Fail. 22(8), 1342–1356 (2020).
Jencks, S. F., Williams, M. V. & Coleman, E. A. Rehospitalizations among patients in the Medicare fee-for-service program. N. Eng. J. Med. 360, 1418–1428 (2009).
Conrad, N. et al. Temporal trends and patterns in heart failure incidence: a population-based study of 4 million individuals. Lancet. 391(10120), 572–580. https://doi.org/10.1016/S0140-6736(17)32520-5 (2018).
Fernandez-Gasso, L., Hernando-Arizaleta, L., Palomar-Rodríguez, J. A., Abellán-Pérez, M. V. & Pascual-Figal, D. A. Trends, causes and timing of 30-day readmissions after hospitalization for heart failure: 11-year population-based analysis with linked data. Int. J. Cardiol. 1(248), 246–251. https://doi.org/10.1016/j.ijcard.2017.07.094 (2017) (Epub 2017 Aug 4 PMID: 28801153).
Méndez-Bailón, M. et al. Significant and constant increase in hospitalization due to heart failure in Spain over 15 year period. Eur. J. Intern. Med. 64, 48–56. https://doi.org/10.1016/j.ejim.2019.02.019 (2019) (Epub 2019 Feb 28 PMID: 30827807).
Biagi P, Gussoni G, Iori I, Nardi R, Mathieu G, Mazzone A, Panuccio D, Scanelli G, Cicatello C, Rinollo C, Muriago M, Galasso D, Bonizzoni E, Vescovo G; CONFINE Study Group. Clinical profile and predictors of in-hospital outcome in patients with heart failure: the FADOI "CONFINE" Study. Int J Cardiol. 2011 Oct 6;152(1):88-94. doi: https://doi.org/10.1016/j.ijcard.2011.02.025
Platz, E. et al. Prevalence and prognostic importance of precipitating factors leading to heart failure hospitalization: Recurrent hospitalizations and mortality. Eur. J. Heart Fail. 20(2), 295–303. https://doi.org/10.1002/ejhf.901 (2018).
Berry, C., Murdoch, D. R. & McMurray, J. J. Economics of chronic heart failure. Eur. J. Heart Fail. 3(3), 283–291. https://doi.org/10.1016/s1388-9842(01)00123-4 (2001) (PMID: 11377998).
Delgado, J. F. et al. Costes sanitarios y no sanitarios de personas que padecen insuficiencia cardiaca crónica sintomática en España. Rev. Esp. Cardiol. 67(8), 643–650 (2014).
Fernández-Bergés, D. et al. Evolución del perfil clínico y pronóstico de pacientes con alta hospitalaria por insuficiencia cardíaca en las dos primeras décadas del siglo xxi. El Regist. INCA-Ex. Aten. Primaria. 54(7), 102357 (2022).
Levey, A. S. et al. CKD-EPI (Chronic kidney disease epidemiology collaboration) a new equation to estimate glomerular filtration rate. Ann. Intern. Med. 150(9), 604–612. https://doi.org/10.7326/0003-4819-150-9-200905050-00006 (2009).
Cappellini, M. D. & Motta, I. Anemia in clinical practice-definition and classification: Does hemoglobin change with aging?. Semin. Hematol. 52(4), 261–269. https://doi.org/10.1053/j.seminhematol.2015.07.006 (2015) (Epub 2015 Jul 17 PMID: 26404438).
Pintilie, M. Análisis de riesgos competitivos [An introduction to competing risks analysis]. Rev. Esp. Cardiol. 64(7), 599–605. https://doi.org/10.1016/j.recesp.2011.03.017 (2011).
Kociol, R. D. et al. International variation in and factors associated with hospital readmission after myocardial infarction. JAMA. 307(1), 66–74. https://doi.org/10.1001/jama.2011.1926 (2012) (PMID: 22215167).
Farré, N. et al. Real world heart failure epidemiology and outcome: A population-based analysis of 88,195 patients. PloS One. 12(2), e0172745 (2017).
Maggioni, A. P. et al. The real-world evidence of heart failure: findings from 41 413 patients of the ARNO database. Eur. J. Heart Fail. 18, 402–410. https://doi.org/10.1002/ejhf.471 (2016).
Fonarow, G. C. et al. Factors identified as precipitating hospital admissions for heart failure and clinical outcomes: Findings from OPTIMIZE-HF. Arch. Intern. Med. 168(8), 847–854. https://doi.org/10.1001/archinte.168.8.847 (2008).
Packer, M. et al. Cardiovascular and renal outcomes with empagliflozin in heart failure. New Engl. J. Med. 383(15), 1413–1424 (2020).
Maggioni, A. P., Dahlström, U., Filippatos, G. & and,. EURObservational research programme: Regional differences and 1-year follow-up results of the heart failure pilot survey (ESC-HF Pilot). Eur. J. Heart Fail 15, 808–817. https://doi.org/10.1093/eurjhf/hft050 (2013).
Van Deursen, V. M. et al. Co-morbidities in patients with heart failure: An analysis of the European heart failure pilot survey. Eur. J. Heart Fail. 16, 103–111 (2014).
Santos, P. M. et al. Mortalidad hospitalaria y reingresos por insuficiencia cardiaca en España. Un estudio de los episodios índice y los reingresos por causas cardiacas a los 30 días y al año. Rev. Española de Cardiol. 72(12), 998–1004 (2019).
Omersa, D., Farkas, J., Erzen, I. & Lainscak, M. National trends in heart failure hospitalization rates in Slovenia 2004–2012. Eur J Heart Fail. 18(11), 1321–1328. https://doi.org/10.1002/ejhf.617 (2016) (Epub 2016 Sep 9 PMID: 27611905).
Álvarez-García, J. et al. investigators of the Spanish heart failure network (REDINSCOR) a simple validated method for predicting the risk of hospitalization for worsening of heart failure in ambulatory patients: the Redin-SCORE. Eur. J. Heart Fail. 17(8), 818–827. https://doi.org/10.1002/ejhf.287 (2015).
Hummel, S. L., Ghalib, H. H., Ratz, D. & Koelling, T. M. Risk stratification for death and all-cause hospitalization in heart failure clinic outpatients. Am. Heart J. 166(5), 895-903.e1. https://doi.org/10.1016/j.ahj.2013.09.002 (2013).
Keenan, P. S. et al. An administrative claims measure suitable for profiling hospital performance on the basis of 30-day all-cause readmission rates among patients with heart failure. Circ. Cardiovasc. Qual. Outcomes. 1(1), 29–37. https://doi.org/10.1161/CIRCOUTCOMES.108.802686 (2008) (PMID: 20031785).
Ouwerkerk, W., Voors, A. A. & Zwinderman, A. H. Factors influencing the predictive power of models for predicting mortality and/or heart failure hospitalization in patients with heart failure. JACC Heart Fail. 2(5), 429–436. https://doi.org/10.1016/j.jchf.2014.04.006 (2014) (Epub 2014 Sep 3 PMID: 25194294).
Berg, D. D. et al. A biomarker-based score for risk of hospitalization for heart failure in patients with diabetes. Diabetes Care. 44(11), 2573–2581. https://doi.org/10.2337/dc21-1170 (2021).
Pacho, C. et al. Early postdischarge STOP-HF-clinic reduces 30-day readmissions in old and frail patients with heart failure. Rev. Esp. Cardiol. Engl. Ed. 70(8), 631–638. https://doi.org/10.1016/j.rec.2017.01.003 (2017).
Axson, E. L. et al. Hospitalisation and mortality in patients with comorbid COPD and heart failure: A systematic review and meta-analysis. Respir. Res. 21, 54. https://doi.org/10.1186/s12931-020-1312-7 (2020).
Gulea, C., Zekeri, R. & Quint, J. K. Impact of chronic obstructive pulmonary disease on readmission after hospitalization for acute heart failure: A nationally representative US cohort study. Int. J. Card. https://doi.org/10.1016/j.ijcard.2019.04.087 (2019).
Vindhyal, M. R., Khayyat, S., Shaaban, A., Duran, B. A. & Kallail, K. J. Decreased renal function is associated with heart failure readmissions. Cureus. 10(8), e3122. https://doi.org/10.7759/cureus.3122 (2018).
Beldhuis, I. E. et al. Renin-angiotensin system inhibition, worsening renal function, and outcome in heart failure patients with reduced and preserved ejection fraction: a meta-analysis of published study data. Circ. Heart Fail. 10(2), e003588. https://doi.org/10.1161/CIRCHEARTFAILURE.116.003588 (2017) (PMID: 28209765).
Su, A., Al’Aref, S. J., Beecy, A. N., Min, J. K. & Karas, M. G. Clinical and Socioeconomic predictors of heart failure readmissions: A review of contemporary literature. Mayo Clin Proc. 94(7), 1304–1320. https://doi.org/10.1016/j.mayocp.2019.01.017 (2019) (PMID: 31272573).
McDonagh, T. A. et al. ESC Scientific document group 2021 ESC guidelines for the diagnosis and treatment of acute and chronic heart failure. Eur Heart J. 42(36), 3599–3726. https://doi.org/10.1093/eurheartj/ehab368 (2021).
Giakoumis, M. et al. Myocardial infarction data acquisition system (MIDAS 36) study group. Readmission and mortality among heart failure patients with history of hypertension in a statewide database. J. Clin. Hypertens. Greenwich. 7, 1263–1274. https://doi.org/10.1111/jch.13918 (2020).
Wideqvist, M., Cui, X., Magnusson, C., Schaufelberger, M. & Fu, M. Hospital readmissions of patients with heart failure from real world: timing and associated risk factors. ESC Heart Fail. 8(2), 1388–1397. https://doi.org/10.1002/ehf2.13221 (2021).
Funding
This work was supported by Junta of Extremadura, co-financed by the European Union (European Regional Development Fund "A way to do Europe"; GR21015). This work was supported by Spain’s Ministry of Science, Innovation and Universities (MICINN) (ERDF; ECO2017-83668-R, PID2020-114231RB-I00, RTI2018-095256-BI00).
Author information
Authors and Affiliations
Contributions
All authors had been involved in drafting of the article or revising it critically for important intellectual content and must have read and approved the final version of the manuscript. Authors are responsible for correctness of the statements provided in the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Rubini, A., Vilaplana-Prieto, C., Vázquez-Jarén, E. et al. Analysis and prediction of readmissions for heart failure in the first year after discharge with INCA score. Sci Rep 13, 22477 (2023). https://doi.org/10.1038/s41598-023-49390-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-023-49390-w
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.