Abstract
Outcomes of conventional mechanical ventilation (CMV) and high-frequency oscillatory ventilation (HFOV) in patients with congenital diaphragmatic hernia (CDH) were compared through a systematic review and meta-analysis. Outcome measures included mortality and incidence of chronic lung disease (CLD). Odds ratio (OR) and 95% confidence interval (95%CI) were evaluated. Subgroup analyses were performed according to the strategy for applying HFOV in CDH patients. Group A: CMV was initially applied in all CDH patients, and HFOV was applied in unstable patients. Group B: chronologically analyzed. (CMV and HFOV era) Group C: CMV or HFOV was used as the initial MV. Of the 2199 abstracts screened, 15 full-text articles were analyzed. Regarding mortality, 16.7% (365/2180) and 32.8% (456/1389) patients died in CMV and HFOV, respectively (OR, 2.53; 95%CI 2.12–3.01). Subgroup analyses showed significantly worse, better, and equivalent mortality for HFOV than that for CMV in group A, B, and C, respectively. CLD occurred in 32.4% (399/1230) and 49.3% (369/749) patients in CMV and HFOV, respectively (OR, 2.37; 95%CI 1.93–2.90). The evidence from the literature is poor. Mortality and the incidence of CLD appear worse after HFOV in children with CDH. Cautious interpretation is needed due to the heterogeneity of each study.
Similar content being viewed by others
Introduction
Congenital diaphragmatic hernia (CDH) is a rare, life-threatening malformation characterized by diaphragmatic defect and herniation of abdominal organs into the thoracic cavity with its estimated prevalence of 2.3 per 10,000 live births1,2. Causes of mortality for CDH are mainly pulmonary hypoplasia and pulmonary hypertension. Endeavors to improve its mortality include immediate resuscitation, adequate mechanical ventilation, and cardiac support in case of severe cardiac dysfunction2. High-frequency oscillatory ventilation (HFOV) can be an elective rescue mode of ventilation as indicated by the APSA outcomes and evidence-based practice committee3. Therefore, the VICI-trial was conducted to determine the optimal initial ventilation mode in congenital diaphragmatic hernia4. Yet there is lack of evidence regarding the comparison of incidence and mortality for chronic lung disease (CLD) between conventional mechanical ventilation (CMV) and HFOV in CDH patients. Hence, we performed this systematic review and meta-analysis to compare these outcomes in CDH.
Materials and methods
Protocol and registration
This systematic review and meta-analysis adhered to the Preferred Reported Items for Systematic Reviews and Meta-Analysis (PRISMA) guidelines. The protocol was registered in PROSPERO (registration number: CRD42022325445).
Literature search
The literature search was performed using PubMed, EMBASE (Ovid), Cochrane library, Web of Science, and Cumulative Index to Nursing and Allied Health Literature (CINAHL) databases. The following keywords were used: congenital diaphragmatic hernia, mechanical ventilation, and high-frequency ventilation. The detailed search strategy is presented in the supplemental material. The search was conducted in April 2022.
Eligibility criteria
Any study reporting comparison of mortality and the incidence of CLD between CMV versus HFOV in CDH was considered eligible. Language was restricted to English. Case reports, review articles, letters, and congress abstracts were excluded. Inclusion criteria were studies which reported the outcome (incidence and mortality of CLD) after comparing CMV and HFOV in infants with CDH. Studies without this comparison were excluded.
Study selection and methodological quality assessment
Two reviewers (H.-B. Y. and H.-Y. K.) independently screened title and abstract of the studies according to the criteria listed above, among the studies retrieved using the search strategy. After first screening, full text was reviewed for final inclusion. These two investigators independently assessed the quality and came to a consensus of all papers that met our inclusion criteria using the Newcastle–Ottawa Scale for comparative studies. Joint review was performed in case of inconsistency.
Data extraction
Systematical extraction of the data was performed regarding study design, study period, mortality, subgroup, and the incidence of CLD from the included studies. A data extraction form was used to record the results.
Subgroup analysis
All studies included in this meta-analysis compared the outcomes of CMV and HFOV. However, heterogeneity was observed regarding the strategy for applying HFOV. Some studies applied HFOV in selected patients who showed persistent unstable vital signs after being initially ventilated with CMV. Others applied HFOV at the first timing of MV and selected either CMV or HFOV. In these studies, CMV was not routinely used as the initial MV strategy. The others compared the historical outcomes of CMV and HFOV. The outcomes of CMV before introducing HFOV were compared with the outcomes of HFOV. Herein, subgroup analyses were performed according to the strategy for applying HFOV in CDH patients. In group A, CMV was initially applied in all CDH patients, and HFOV was applied in unstable patients showing poor outcomes in CMV. In group B, the results of CMV and HFOV were chronologically analyzed. The use of HFOV was more recent than the use of CMV in all studies in group B. In group C, either CMV or HFOV was used as the initial MV, which is different from group A, which used CMV as the routine initial MV strategy.
Statistical analysis
Statistical analysis was performed using R × 64 4.1.2. Pooled estimates of odds ratios (ORs) with 95% confidence intervals (95%CIs) were evaluated using standard methods. Both fixed and random-effects models were used. Heterogeneity between studies was assessed using the I2 statistic. The forest plot and funnel plot were used to estimate the overall result and publication bias, respectively.
Results
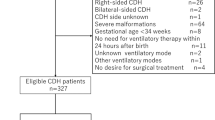
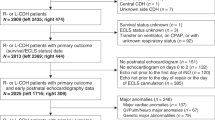
Of 2199 studies found by defined search strategy, 1636 abstracts were reviewed, and 88 full-text articles were examined. Of these, 15 studies were included in this study4,5,6,7,8,9,10,11,12,13,14,15,16,17,18 (Fig. 1). There was one prospective randomized clinical trial. Table 1 summarizes the presentation center, patient enroll timing, and main results of the study. Mortality rate were reported in all studies and the incidence of CLD was reported in 6 papers among the 15 included studies. Various countries, including the United Kingdom, the United States, France, and Canada conducted the studies. Patients were included from 1981 to 2017. Most of them were retrospective studies and one paper was prospective RCT.
Mortality
The pooled result of all enrolled studies for mortality showed significantly higher mortality in HFOV (Fig. 2). In total, there were 456 deaths in HFOV (n = 1389) and 365 deaths in CMV (n = 2180). The ORs were 2.53 for the fixed model and 2.16 for the random-effect model, respectively; 95%CIs did not contain the value 1. In I2 statistics, heterogeneity was observed to be 86%, higher than the 50% cut-off, indicating high heterogeneity between studies.
In subgroup analysis, Group A had statistically significantly higher mortality in HFOV group with OR 3.18 in fixed model. (Fig. 3) Group B had significantly lower mortality in the HFOV group with OR 0.22 in fixed model. In group C, OR was 1.69 in fixed model, but it was not statistically significant. The funnel plot for overall mortality is reported in Fig. 4.
The funnel plots for overall mortality are shown in Fig. 4.
The incidence of CLD
Regarding the incidence of CLD, the OR and 95%CI were 2.37 and 1.93–2.90, respectively, for the fixed model. In other words, the incidence of CLD was significantly higher in HFOV (Fig. 5).
The funnel plots for the incidence of CLD are presented in the supplemental materials.
Discussion
CDH that needs not only various medical supports according to the underlying condition of the patients but also requires surgical treatment of diaphragmatic defect is a complex disease that shows high mortality rate even with modern developed perinatal care. The mortality rate is known to reach 40–100% in low-, middle-income countries whereas reported as 30% in developed countries2,19. Careful perinatal management is required, especially for respiratory system, pulmonary HTN, and cardiac dysfunction, which are critical for the patient's survival. The most important point of the respiratory management is to use management that can prevent ventilator-induced lung injury20. The introduction of gentle ventilation contributed to the improvement of survival rate. Delayed repair and extracorporeal membrane oxygenation contributed to increase the survival rate by 50% until the early 1990s, and permissive hypercapnia improved the survival rate by an additional 10%19. Mechanical ventilation strategies such as HFOV and HFJV have been introduced in clinical practice and are being applied for the unstable CDH patients21,22.
This meta-analysis compares the outcome of CMV and HFOV of CDH in over three thousand new-born children with CDH. This study shows that the evidence for the comparison of HFOV and CMV for CDH is scarce. In subgroup analysis, the patients with HFOV showed better survival in group B in which showed chronological analysis of the outcomes of CMV and HFOV.
A pooled result of all enrolled studies for mortality is higher in HFOV than in CMV. (OR: 2.53, 95%CI 2.12–3.01) Since there are heterogeneities regarding the application of HFOV all through the enrolled studies, subgroup analysis was performed. Group A in which applied HFOV in the unstable patients who were initially applied CMV showed statistically significant higher mortality in HFOV (OR: 3.18, 95%CI 2.63–3.84). Group B in which analyzed the outcomes of CMV before the introduction of HFOV and of HFOV after the introduction of HFOV showed statistically significant better survival in HFOV. Group C in which applied either of CMV or HFOV at the timing of the application of MV did not show statistically significant result. The outcome of HFOV could be explained with the characteristics of subgroups. The mortality of group A might be higher in HFOV because the HFOV was selectively applied in poor patients with the use of CMV. More accurate results could be elicited if a randomized controlled study was completed comparing the effectiveness of HFOV and CMV in unstable patients with CDH. Further, those patients in group A where CMV did not treat respiratory acidosis properly may have a benefit from ECMO. HFOV often delays ECMO and therefore survival rate could drop. Early ECMO may have better results23. Since group B is a comparison of different periods before and after the introduction of HFOV, other advanced perinatal care other than HFOV may have affected the outcome, resulting in a low mortality rate in HFOV. There are many developments in the care of CDH not only in the area of mechanical ventilation strategy. Surfactant use, fraction of inspired oxygen, the concept of gentle ventilation, the importance of the management of pulmonary hypertension24. The improvement in mortality of CDH could also be related improving prenatal care. Also, in the younger era without protocols concerning to standard of care and ventilator settings, cares were not limited as recommended in a standardized protocol25. Group C showed no significant difference, which can be explained as follows. The use of HFOV may have no additional benefit compared to CMV in patients who are stable with CMV alone. Unstable patients could benefit with HFOV whereas either HFOV or CMV could offer similar results in relatively stable patients. Of interest a study published in 2016 by Snoek (Group C in this analysis), suggests that HFOV caused overinflation and had a longer ventilation period, which may have caused ventilator-induced lung injury by more tracheal suction. HFOV could have limitations than CMV, which can cause deterioration in vulnerable patients26. In the VICI Trial high initial ventilator settings were allowed and there was also a trend to a later initiation of rescue ECMO after initial application of HFOV.4 A future study concerning to HFOV should be done with lower settings of HFOV and early ECMO as a rescue treatment.
Chronic lung disease is known to occur in 30–50% of CDH survivors20. It is known that the incidence of CLD is higher when ECMO is used and patch repair is performed27, but there is insufficient evidence that HFOV reduces CLD incidence28. In this meta-analysis, the incidence of CLD was higher in HFOV. Because the number of the enroll studies was small, subgroup analysis like mortality could not be performed. As in mortality, it may have occurred more in HFOV due to baseline characteristic differences between groups more than the difference of the MV modality. Therefore, it seems difficult to reach a clear conclusion.
This study is limited by the heterogeneity of indications for using HFOV or CMV. The evidence from the systematic review is poor due to low level of evidence (a single randomized controlled trial). Also, in further studies risk stratifications should be done by some prenatal information like lung volumes or liver position, or analysis should be done in only isolated CDH patients without other major malformations or syndromes. One study suggested to make a distinction between mild moderate and severe CDH29.
On the basis of the poor existing evidence, mortality and the incidence of CLD appear worse after HFOV compared to CMV. Cautious interpretation of this result is needed and only a well-designed prospective study involving large number of patients could address this issue.
Data availability
The data generated during this study are available from the corresponding author on reasonable request.
References
Paoletti, M. et al. Prevalence and risk factors for congenital diaphragmatic hernia: A global view. J. Pediatr. Surg. 55, 2297–2307 (2020).
Zani, A. et al. Congenital diaphragmatic hernia. Nat. Rev. Dis. Primers. 8, 37 (2022).
Puligandla, P. S. et al. Management of congenital diaphragmatic hernia: A systematic review from the APSA outcomes and evidence based practice committee. J. Pediatr. Surg. 50, 1958–1970 (2015).
Snoek, K. G. et al. Conventional mechanical ventilation versus high-frequency oscillatory ventilation for congenital diaphragmatic hernia: A randomized clinical trial (The VICI-trial). Ann. Surg. 263, 867–874 (2016).
Aihole, J. S. et al. A clinical study on congenital diaphragmatic hernia in neonates: Our institutional experience. J. Indian Assoc. Pediatr. Surg. 23, 131–139 (2018).
Azarow, K. et al. Congenital diaphragmatic hernia–a tale of two cities: The Toronto experience. J. Pediatr. Surg. 32, 395–400 (1997).
Beres, A. L., Puligandla, P. S., Brindle, M. E. & Capsnet,. Stability prior to surgery in Congenital Diaphragmatic Hernia: Is it necessary?. J Pediatr Surg 48, 919–923 (2013).
Cacciari, A. et al. High-frequency oscillatory ventilation versus conventional mechanical ventilation in congenital diaphragmatic hernia. Eur. J. Pediatr. Surg. 11, 3–7 (2001).
Derraugh, G. et al. High-frequency vs. conventional ventilation at the time of CDH repair is not associated with higher mortality and oxygen dependency: A retrospective cohort study. Pediatr. Surg. Int. 36, 1275–1280 (2020).
Desfrere, L. et al. Impact of delayed repair and elective high-frequency oscillatory ventilation on survival of antenatally diagnosed congenital diaphragmatic hernia: First application of these strategies in the more “severe” subgroup of antenatally diagnosed newborns. Intensive Care Med 26, 934–941 (2000).
Fuyuki, M. et al. Prognosis of conventional vs. high-frequency ventilation for congenital diaphragmatic hernia: A retrospective cohort study. J. Perinatol. 41(4), 814–823 (2021).
Khachane, Y., Halliday, R., Thomas, G., Maheshwari, R. & Browning Carmo, K. Outcomes for infants with congenital diaphragmatic hernia: A single campus review with low extracorporeal membrane oxygenation utilisation. J. Paediatr. Child Health 58, 90–96 (2022).
Ng, G. Y. et al. Reduction in ventilator-induced lung injury improves outcome in congenital diaphragmatic hernia?. Pediatr. Surg. Int. 24, 145–150 (2008).
O’Rourke-Potocki, A., Ali, K., Murthy, V., Milner, A. & Greenough, A. Resuscitation of infants with congenital diaphragmatic hernia. Arch. Dis. Child Fetal Neonatal. Ed. 102, F320–F323 (2017).
Reyes, C. et al. Delayed repair of congenital diaphragmatic hernia with early high-frequency oscillatory ventilation during preoperative stabilization. J Pediatr Surg 33, 1010–1014 (1998).
Sahoo, T. et al. Predictors of mortality among neonates with congenital diaphragmatic hernia: Experience from an inborn unselected cohort in India. Indian Pediatr. 56, 1037–1040 (2019).
Takayasu, H. et al. Analysis of risk factors of long-term complications in congenital diaphragmatic hernia: A single institution’s experience. Asian J Surg 40, 1–5 (2017).
van den Hout, L. et al. Risk factors for chronic lung disease and mortality in newborns with congenital diaphragmatic hernia. Neonatology 98(4), 370–380 (2010).
Vitali, S. H. & Arnold, J. H. Bench-to-bedside review: Ventilator strategies to reduce lung injury—lessons from pediatric and neonatal intensive care. Crit. Care 9, 177–183 (2005).
van den Hout, L. et al. Can we improve outcome of congenital diaphragmatic hernia?. Pediatr. Surg. Int. 25, 733–743 (2009).
Kuluz, M. A. et al. Preliminary observations of the use of high-frequency jet ventilation as rescue therapy in infants with congenital diaphragmatic hernia. J. Pediatr. Surg. 45, 698–702 (2010).
Logan, J. W., Cotten, C. M., Goldberg, R. N. & Clark, R. H. Mechanical ventilation strategies in the management of congenital diaphragmatic hernia. Semin. Pediatr. Surg. 16, 115–125 (2007).
Wegele, C. et al. Impact of time point of extracorporeal membrane oxygenation on mortality and morbidity in congenital diaphragmatic hernia: A single-center case series. Children 9, 986 (2022).
Yang, M. J., Russell, K. W., Yoder, B. A. & Fenton, S. J. Congenital diaphragmatic hernia: A narrative review of controversies in neonatal management. Transl. Pediatr. 10, 1432–1447 (2021).
Snoek, K. G. et al. Neurodevelopmental outcome in high-risk congenital diaphragmatic hernia patients: An appeal for international standardization. Neonatology 109, 14–21 (2016).
Meyers, M., Rodrigues, N. & Ari, A. High-frequency oscillatory ventilation: A narrative review. Can J Respir Ther 55, 40–46 (2019).
Muratore, C. S. et al. Pulmonary morbidity in 100 survivors of congenital diaphragmatic hernia monitored in a multidisciplinary clinic. J. Pediatr. Surg. 36, 133–140 (2001).
Cools F, Offringa M, Askie LM. Elective high frequency oscillatory ventilation versus conventional ventilation for acute pulmonary dysfunction in preterm infants. Cochrane Database Syst. Rev. CD000104 (2015)
Deprest, J. A. et al. Randomized trial of fetal surgery for moderate left diaphragmatic hernia. N. Engl. J. Med. 385(2), 119–129 (2021).
Author information
Authors and Affiliations
Contributions
H.Y. K. and A. P. conceptualized the study. H.B. Y. wrote the main manuscript text. H.Y. K. and H.B Y. contributed to data acquisition, data analysis. H.B. Y prepared all figures. All authors contributed to critical revision and reviewed the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Yang, HB., Pierro, A. & Kim, HY. Comparison of conventional mechanical ventilation and high-frequency oscillatory ventilation in congenital diaphragmatic hernias: a systematic review and meta-analysis. Sci Rep 13, 16136 (2023). https://doi.org/10.1038/s41598-023-42344-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-023-42344-2
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.