Abstract
The aim of this meta-analysis was to answer the following question: “Are there any differences in opiorphin biomarker concentrations between different orofacial conditions and controls?”. Two reviewers searched for observational studies that evaluated the levels of opiorphin in orofacial conditions, annotated in seven main databases and three that compile gray literature. Of the 443 articles obtained initially, 8 met the inclusion criteria for quantitative analyses. Relative percentages showed a mean 24.1% higher opiorphin concentration in chronic conditions (Burning Mouth Syndrome, Oral Potentially Malignant Diseases and Temporomandibular Disorder) compared to controls; 33.2% higher opiorphin in sustained pain (Symptomatic Irreversible Pulpitis, Symptomatic Apical Periodontitis, Painful Oral Soft-tissue conditions); and 21.7% higher opiorphin after stimuli (Corneal Foreign Body, Capsaicin). Meta-analysis revealed a standardized mean difference of 0.62 [0.02, 1.22] in the absolute concentration of opiorphin in saliva for the chronic group compared to the control. The analogous values for the sustained group and the stimulated group were 2.24 [0.34, 4.14] and 0.43 [0.00, 0.85], respectively. No differences in opiorphin levels were found for ‘after Local Anesthesia before Tooth Extraction’ or for apicoectomy. Based on the available evidence, in general, a statistically higher level of opiorphin is found in orofacial conditions. Salivary opiorphin levels are elevated in chronic, persisted and acute pain conditions, presumably reflecting a physiological homeostatic adaptative response to different conditions such as stress or pain. Salivary opiorphin might therefore be used as a valuable biomarker in several oral disorders.
Similar content being viewed by others
Introduction
Orofacial pain (OP) defined as pain perceived in the face and/or oral cavity is caused by diseases or disorders of regional structures, by dysfunction of the nervous system, or through referral from distant sources1. This prevalent condition affects approximatively 20% of the population2, and encompasses a range of diagnoses3. These include acute and chronic pain, with the most prevalent being dental, periodontal and mucosal pain, temporo-mandibular disorders, primary or secondary burning mouth, painful trigeminal neuropathies. Similar to spinal pain, but with specificities related to the trigeminal system, OFP can be inflammatory, neuropathic or nociplastic in nature. OFP diagnosis is difficult, involving many health care specialists and often necessitating additional diagnosis tools like imaging and biological tests. Difficult also is its management, especially for chronic pain. As a consequence, OFP is a burden impacting quality of life of individuals and entailing considerable societal financial costs. Oral diseases affect more than 3.5 billion people worldwide with dental caries, frequently associated with pain, being the most prevalent disease4,5. Direct treatments for oral diseases account for approximatively 4.6% of global health expenditures6. Regarding persistent orofacial pain only, Breckons et al.7 estimated that mean out-of-pocket costs per person over a 6-month period were £333, with indirect costs reaching £1242.
Efforts to diagnose and treat OFP would benefit from the development of biomarkers in the context of the various inflammatory, infectious, autoimmune, and premalignant/malignant conditions that can affect the orofacial region. Saliva offers numerous advantages as a source of biomarkers of orofacial (and other) abnormalities, including pain8,9,10. For example, saliva and its constituents have been under investigation for more than a century, and collecting saliva samples is non-invasive and convenient11,12,13.
Opiorphin, a newly discovered pentapeptide (Gln–Arg–Phe–Ser–Arg) present in human saliva, exhibits analgesic and anxiolytic effects14 with promising therapeutic applications. It was first isolated by a dual biochemical and functional approach14, based on two related peptides, spinorphin and sialorphin, isolated from bovine spinal cord15 and rat saliva, respectively16,17. Opiorphin acts as an inhibitor of zinc metalloectopeptidases (MZPs), a class of proteases including neutral endopeptidase and aminopeptidase-N14. These membrane-anchored enzymes degrade circulating peptides such as enkephalins and substance P to limit their physiological roles. Therefore, MZP inhibition prolongs the physiological effects of natural peptides and, interestingly in therapeutics, it avoids the side effects observed with drugs acting as receptor agonists. For example, in vitro, opiorphin completely protects Met-enkephalin from degradation without directly interacting with opioid receptors. Opiorphin produces antinociceptive and anxiolytic/antidepressant effects with no associated tolerance (or morphine cross-tolerance)18,19,20 and displays analgesic properties similar to those of morphine in an acute mechanical pain model in rats14. Recent translational studies have shown that a synthetic analog of opiorphin suppresses mechanical hypersensitivity in a rat model of neuropathic pain21. Opiorphin’s effects are suppressed by the opioid receptor antagonist naloxone, evidencing its action through endogenous opioid-dependent pathways20. Taken together, these data suggest a promising role for opiorphin as a biomarker as well as a therapeutic agent.
While the physiological cycle of opiorphin remains unclear, the rat analog sialorphin is secreted in salivary mandibular glands in response to diverse conditions like fear, stress, or pain, serving as a molecular effector within the cervical sympathetic trunk submandibular gland (CST-SMG) axis22. This axis modulates homeostatic processes and underscores salivary glands as a source of locally and systemically active immunoregulatory and anti-inflammatory factors22. Given that many OFP conditions are influenced by inflammatory factors23,24,25,26 exploring the CST-SMG axis through opiorphin release could enhance the understanding and management of OFP conditions.
In humans, several studies have assessed variations of salivary opiorphin levels under different conditions including pain and stress27,28. Opiorphin's potential as a biomarker has been explored in various pathologies such as Temporomandibular Disorder (TMD)27, Burning Mouth Syndrome (BMS)29,30, Oral Potentially Malignant Disorders (OPMD)8, dental pain as Symptomatic Irreversible Pulpitis (SIP)31 and Symptomatic Apical Periodontitis (SAP)31, anorexia nervosa32,33, ocular pain with Corneal Foreign Body (CFB)34, and depressive19 and erectile disorders35,36,37. However, the medical literature's results are yet to be fully integrated, sometimes showing apparent contradictions across conditions. For instance, opiorphin levels have been reported to increase in dental inflammatory pain31, decrease after oral local anesthesia38. In BMS, perhaps the most emblematic conditions for looking a link between opiorphin and oral pain, several measurements have shown conflicting results. For example Ruangsri et al.39 report a decrease of opiorphin levels in BMS patients compared to control subjects when Salaric et al.29,30 report an increase and Boucher et al.29,30 a statistically non-significant decrease. Heterogeneity in methodology and study quality might contribute to these discrepancies, highlighting the need for a comprehensive review of available evidence concerning OFP and opiorphin release.
To our knowledge, there is no systematic review or meta-analysis aimed at measuring salivary opiorphin levels in orofacial conditions. Therefore, based on these premises, the aim of this meta-analysis was to answer the following question: “Are there any differences in opiorphin biomarker concentrations between different orofacial conditions and controls?”. Our hypothesis was that higher levels of opiorphin are founded in pain conditions than controls In case of differences, the surrogate questions are “can methodological differences account for discrepancies in the studies?”, “are there any differences in salivary opiorphin levels according to OFP subtypes?”. “is there any correlation between opiorphin salivary levels and intensity of OFP”, and “what is the time course of opiorphin release in OFP?”.
Materials and methods
Protocol and registration
This systematic review conforms to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) Checklist40. The protocol is registered in the International Prospective Register of Systematic Reviews (PROSPERO) under number CRD42021269661.
Eligibility criteria
We included observational studies (case–control, cross-sectional and cohort studies) and case series (> 10 cases) that evaluated opiorphin in orofacial conditions, but included only adults (18–65 years old). The included studies evaluated opiorphin extracted from blood (including plasma), saliva (different preparations), urine, or tears, assessed by ELISA or chromatography.
Overall, the inclusion criteria were based on the PECOS question41:
Population (P): Humans; Exposure (E): Opiorphin; Comparison (C): Controls; Outcome (O): Different concentrations; Study design (S): observational studies and case series. No data, sex or language restrictions were applied to the search strategy.
The exclusion criteria were as follows:
(1) Studies in animals; (2) studies where no orofacial condition was evaluated; (3) studies where opiorphin was not evaluated through saliva, blood, urine or tears; and (4) literature reviews, intervention studies, books, letters, case reports (< 10 cases) and personal opinions.
Information sources and search strategy
Detailed individual search strategies were developed for each bibliographic electronic database: Cochrane, EMBASE, Latin American and Caribbean Health Sciences (LILACS), LIVIVO, PubMed (including Medline), Scopus and Web of Science. A gray literature search was performed on Google Scholar, Open Grey and ProQuest. All database searches were conducted from the starting coverage date through October 28, 2022. More information on the search strategies is provided in Appendix 1 (which can be found online). Furthermore, the authors hand-searched the reference lists of the selected articles for any additional references that might have been missed in the database searches. We also sought out articles by contacting relevant experts. These individuals were contacted if they had published 2 or more papers about the same systematic review topic. All references were managed and the duplicated hits were removed by using reference manager software (EndNote X7® Basic-Thomson Reuters, New York, EUA).
Selection process and data collection process
This part followed a two-phase process. In phase-one, two authors (A.L.P. and C.A.O.M) independently evaluated the titles and abstracts of all identified electronic database citations. In phase-two, the same authors evaluated full-text data. They independently screened papers at phase-one and -two, applied the eligibility criteria, collected key information from the selected studies, and crosschecked the information. The final selection was based solely on full-text assessment of the studies. When disagreement arose, a third author (Y.B.) was involved to make a final decision about whether to include or exclude a study.
Data items
For each of the included studies, the following items were recorded: author(s), year of publication, country, sample size, demographic features of the sample (n, mean age and standard deviation, percentage of women), method of collection, information about this method, results, and main conclusions. When the required data were not complete, the reviewers (A.L.P. and C.A.O.M) attempted to contact the study authors to retrieve any unpublished information. Three attempts were made in a 30-day period, by email for the first, second and last author.
Study risk of bias assessment
The methodological quality of each included observational study was evaluated through Joanna Briggs Institute (JBI) Critical Appraisal Tools to assess risk of bias42,43,44. The answers could be “yes”, “unclear”, “no”, or “not applicable”. Decisions about scoring were agreed upon by all reviewers before critical appraisal commenced. The same two reviewers (A.L.P. and C.A.O.M) worked out any initial differences regarding data analysis. A third author (Y.B.) was involved to reach a decision in case of uncertainty. After these ratings, the risk of bias was categorized according to: (1) low risk of bias, if all criteria were met, (2) unclear risk of bias, if one or more criteria were not described exactly how they were met, and (3) high risk of bias, if one or more criteria were not met44. Figures of the quality assessment of all included studies were generated with Review Manager 5.3 (RevMan 5.3, The Nordic Cochrane Centre, Copenhagen, Denmark)45.
Effect measures
We considered the results in terms of both absolute and relative differences in fluid opiorphin concentrations. The standardized mean difference was used as an effect measure for continuous outcomes. To standardize the results of the studies to a uniform scale, we transformed all measures to ng/ml values. Any type of outcome measurement was considered. We attempted to standardize the measurements as mean and standard deviation (SD).
Synthesis methods
Statistical pooling of data using meta-analysis was carried out where studies were considered combinable and relatively homogeneous in relation to design, interventions, and outcomes. Heterogeneity within studies was evaluated either by considering clinical (differences about participants, type of interventions and results), methodological (design, and risk of bias) and statistical characteristics (effect of studies) or by using the inconsistency index (I2) statistical test45.
If quantitative synthesis was appropriate, analysis of the standardized mean difference was performed using RevMan 5.3, and heterogeneity was assessed using the Cochran Q test and I2 statistics. For the analysis model, a fixed or random effect was based on an expectation of whether the intervention effects were truly identical, preferring the fixed-effect model if this was likely and a random-effects model if this was unlikely. Heterogeneity was calculated by I2, and a value greater than 50% was considered an indicator of substantial heterogeneity between studies. The significance level was set at 5%. The meta-analysis was performed with the aid of Review Manager software version 5.3.5 (Nordic Cochrane Center, Copenhagen, Denmark) for continuous data following the appropriate Cochrane Guidelines45.
We also considered generating a funnel plot as a graphic to address reporting biases, but in the end our sample size was too small (< 10 articles) for that method of analysis.
Risk of bias across studies and reporting bias assessment
The risk of bias across studies was considered in terms of an overall risk the study results may present, which could influence meta-analysis data. Methodological and statistical heterogeneity was evaluated by comparing the variability in study designs and the risk of bias. Furthermore, we also assessed the risk of bias due to missing results.
Certainty assessment
A summary of the overall strength of evidence available was presented using "Grading of Recommendations Assessment, Development and Evaluation" (GRADE) Summary of Findings (SoF) tables, using GRADEpro software45.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Informed consent
For this type of study, formal consent is not required.
Results
Study selection
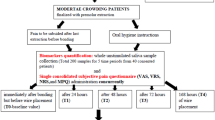
Our initial database searches up to June 2021, identified 443 studies. After eliminating duplicated hits, 133 studies remained of which 115 were excluded after title and abstract review, resulting in 18 articles. In addition, 71 studies were found with Google Scholar, 1 with OpenGrey, and 37 with ProQuest. Of these latter 109 studies, 3 from Google Scholar were selected for full-text reading. No additional study was selected following hand-searching of the reference lists of the included studies, although 1 further study was included based on suggestion by an expert. Thus, 22 studies became part of phase-2. The search was updated on October 28, 2022. We found a total of 103 more papers (9 in PubMed, 12 in Scopus, 1 in Cochrane, 43 in Web of Science, 0 in LILACS, 13 in EMBASE, 12 in LIVIVO, and 13 in Google Scholar); however, all 103 were excluded because “no orofacial condition was evaluated” (exclusion criterion #2). During phase-2, 14 of the 22 studies were excluded (reasons for exclusion are given in Appendix 2), leaving 8 studies for qualitative and quantitative synthesis. A flowchart of the process of identification, inclusion and exclusion of studies is shown in Fig. 1.
Study characteristics and results of individual studies
In the 8 studies evaluated, mean sample size ranged from 2238 to 14446, with a total of 338 subjects with one orofacial condition, and 118 healthy controls. The proportion of women in the studies ranged from 4031 to 90.4%30. Studies were conducted in Croatia27,29, France30, India8,46, Iraq38, and Turkey31,34. All studies were published in English. The study by Alajbeg et al.27 was part of a clinical trials protocol, and the data were obtained by contacting the authors by e-mail.
Studies encompassed different orofacial conditions: Chronic Temporomandibular Disorder (TMD)27, Burning Mouth Syndrome (BMS)29,30, Painful Oral Soft-tissue Conditions (POSC)8, Oral Potentially Malignant Disorders (OPMD)8, Symptomatic Irreversible Pulpitis (SIP)31, Symptomatic Apical Periodontitis (SAP)31, Corneal Foreign Body (CFB)34, Local Anesthesia before Tooth Extraction (LA)46 and Apicoectomy38.
Study designs included 5 case–control studies8,27,29,30,34, 1 randomized clinical trial46 and 2 quasi-randomized studies31,38. Opiorphin levels were measured in saliva in 7 studies, except Boucher et al.30 also tested blood and urine; Ozdogan et al.34 measured opiorphin in tears. A human opiorphin ELISA kit was used in all but 2 studies; the exceptions were Alajbeg et al.27 and Saláric et al.29 who performed electrospray positive ionization-mass spectrometric multiple reaction monitoring (ESI+/MRM). Table 1 and Appendix 6 (descriptive methods for opiorphin collection) summarize the descriptive characteristics of the included studies.
Risk of bias in studies
Risk of bias was heterogeneous among the 8 studies. Using JBI Critical Appraisal Tools, 2 studies were classified as having low risk of bias29,30, 3 as unclear8,27,46, and 3 as high risk of bias31,34,38. The higher risk of bias related to strategies to deal with confounding factors. The complete item list is presented in Fig. 2 and Appendix 3.
Results of syntheses
Individually, TMD, SIP, SAP and CFB were associated with higher concentrations of opiorphin than the control, whereas BMS, POSC, OPMD and LA showed no difference. We further divided the conditions into 4 groups: chronic orofacial group (TMD, BMS and OPMD); sustained pain group (SIP, SAP and POSC); acute pain after local anesthesia group (tooth extraction and apicoectomy); and stimulated group (after CFB, and capsaicin), according to the physio-pathological processes underlying these heterogenous conditions. TMD, BMS and OPMD are chronic conditions (> 3 months) with peripheral and central involvement. SIP and SAP are similar conditions involving long-term alterations in nerve pathways (bacterial inflammation and sensitization) which peak in acute pain, but are not considered as chronic pain conditions. Regarding the others, we thought of merging the acute pain and stimulated groups but the studies are fundamentally different in nature. CFB and capsaicin provoke pain on a short-term basis (minutes or hours), whereas the anesthesia study aimed to suppress pain with an anesthetic.
Based on the data presented in the included studies, we calculated the relative percentage of opiorphin change versus the control group. In the chronic group, patients with TMD exhibited a 65.8% (SD 68.7%) higher opiorphin concentration than controls. An increase was also found for BMS, with 38.3% (SD 79.3%), and OPMDs, with 24.5% (SD 25.2%). In the sustained group, SIP exhibited 50.2% (SD 16.3%) and SAP 35.4% (SD 20.2%) higher opiorphin concentrations before endodontic treatment; and POSC was 14.0% higher (SD 29.2%). After anesthesia, opiorphin levels were 143.1% (SD 90.27%) higher in apicoectomy subjects, and 4.2% lower in tooth extraction subjects. After stimulation, opiorphin was 22.9% (SD 27.6%) and 20.5% (SD 68.7%) higher in cases of CFB and after capsaicin, respectively (Appendix 4). Overall, the relative opiorphin concentration was 24.1% (SD 60.9%) higher in chronic conditions compared to controls; 33.2% (SD 21.9%) higher in persisted pain, and 21.7% (SD 56.7%) higher after stimuli. No differences were found after local anesthesia.
In addition, we conducted a meta-analysis of the 8 selected studies (Fig. 3). To minimize bias, we used the standardized mean difference as a measure of effect size, because the studies all assess the same outcome but measure it in a variety of ways. The heterogeneity between the studies was high on this meta-analysis (I2: 70–90%) because the results were derived from different types of orofacial conditions, and a random effect was considered. Meta-analysis of the chronic group (TMD, BMS, OPMDs) showed a 0.62 [0.02, 1.22] standardized mean difference in the absolute concentration of opiorphin in saliva compared to controls. The sustained group (painful oral soft-tissue conditions vs. controls; and SAP and SIP, before vs. after treatment) showed a 2.24 [0.34, 4.14] standardized mean difference. The stimulated group (capsaicin, CFB) showed a 0.43 [0.00, 0.85] standardized mean difference in the absolute concentration of opiorphin ‘after stimulus’ when compared to ‘before stimulus’. No meta-analysis was feasible for the acute pain after local anesthesia group, owing to a lack of SD data. In general, a statistically higher level of opiorphin was observed in orofacial conditions compared to controls.
Forest plots indicating different concentration of opiorphins in saliva on orofacial pain conditions compared to controls. Graphs generated with Review Manager 5.3 (RevMan 5.3, The Nordic Cochrane Centre, Copenhagen, Denmark). (A) Chronic orofacial group (TMD, BMS and OPMD); (B) sustained pain group (SIP, SAP and POSC); (C) stimulated group (after CFB, and capsaicin). CI confidence interval, OPMDs oral potentially malignant disorders, POSC painful oral soft-tissue conditions, SAP symptomatic apical periodontitis, SIP symptomatic irreversible pulpitis, SD standard deviation, TTM treatment.
Risk of bias across studies and reporting biases
The 8 selected studies had case–control, randomized and quasi-randomized designs. The main methodological problem concerned assessment of outcomes in a healthy control group. Moreover, strategies to deal with confounding factors such as age, sex and psychosocial status were not always addressed. The main problem related to reporting biases was a lack of standardization of units of measure; for example, in some studies the values were only presented in figures and not as precise numerical values in tables.
Certainty of evidence
The overall quality of evidence identified using GRADE’s SoF tables was assessed as very low (Appendix 5), because of high risk of bias, inconsistency (I2) greater than 70%, outcomes not related to the review question, and small pooled sample size.
Discussion
To our knowledge, this study is the first to systematically review the available evidence related to the concentration of opiorphin in patients with orofacial conditions compared to control subjects. Opiorphin levels were overall increased in OFP conditions. Relative percentages showed 24.1%, 33.2% and 21.7% higher opiorphin levels in chronic pain (TMD, BMS, and OPMDs), sustained pain (SAP, SIP, POSC), and after painful stimulus (CFB, capsaicin), respectively. Meta-analysis found significant standardized mean differences in the absolute concentration in all pain groups compared to controls. While interesting, these findings should be interpreted with caution since several factors may limit their value, as discussed below.
Technical issues
Opiorphin levels were not assessed by the same method in all 8 studies, potentially leading to differences in absolute values. Two studies used HPLC coupled to ionization27,29 to measure opiorphin and 6 used ELISA8,31,34,38,46,47, with 4 different analysis kits. This might explain some discrepancy in the results. ELISA is easy to perform and relatively inexpensive but has a relatively high Limit of Detection (LOD), i.e., the smallest amount of the analyte that can be detected in the test sample. Electrospray positive ionization-mass spectrometric multiple reaction monitoring (ESI+/MRM)29,48,49 provides much higher sensitivity and specificity but requires highly specialized equipment and software, which limits its usefullness.
OFP subtypes
The studies included in this review encompass different orofacial conditions. Individually, TMD, SIP, SAP and CFB were reported to have higher concentrations of opiorphin than controls; however, no differences were noted for BMS, POSC, OPMD and LA. When considering the subcategories i.e. chronic pain, sustained pain, acute pain after local anesthesia, and stimulated acute pain, comparative analysis suggest that chronic pain conditions result in higher opiorphin levels, although not for all conditions since BMS data do not support this finding. Indeed two studies report contradictory results29,30. The study of Boucher et al.29,30 reported non-significant differences in the concentration of opiorphin in controls compared to patients with BMS, whereas Salaric et al.29,30 found a higher concentration in the BMS group. In addition, the results of these studies slightly differed when the saliva collected for analysis was stimulated saliva or non-stimulated saliva. Furthermore another study, not included in this meta-analysis39 because only published in an abstract form, reported lower levels of salivary opiorphin in BMS patients. Overall, these discrepancies do not provide strong evidence for a link between opiorphin and BMS which might be related to the complex physiopathology of BMS. This condition is understood as a nociplastic condition including hormonal and neuropathic alterations, possibly related to stress50 when the other OFP included in this review display stronger nociceptive/inflammatory components. Besides chronic conditions, sustained pain conditions also produced an increase of opiorphin, reinforcing the hypothesis that opiorphin is produced as a long-term adaptive response. However; it must be emphasized that some studies are characterized by a high risk of bias owing to lack of clinical information. For example, in the OPMD study8 it is not clear whether BMS subjects were included.
Ozdogan et al.31 measured opiorphin levels in pain-free patients 30 days after endodontic treatment, effectively a control group; the opiorphin levels returned to normal after a sustained rise elicited by pain of pulpitis or periapical periodontitis. This likely reflects a long term process even if the pain peaks for just one or a few years. Indeed, studies with local anesthesia, including subjects before tooth extraction46 and apicoectomy38, showed no decrease of opiorphin after a few minutes or after one week, suggesting again sustained, long-term opiorphin production. For acute pain, measurements of opiorphin a few minutes after local anesthesia gave contradictory results: one study showed an increase in opiorphin levels of 143.1%38, whereas a second study reported a decrease of 4.1%46.
Intensity of pain and opiorphin levels
A correlation between pain intensity on a visual analog scale (VAS) and opiorphin level was supported in only one study. Ozdogan et al.31 observed a positive correlation in the painful SIP and SAP pre-treatment group. Other studies did not find or did not report this parameter. However, it must be emphasized that these data are at high risk of bias. For instance, Al-Saffar et al.38 claimed an inverse correlation between opiorphin levels and VAS post-LA but provided no numeric pain evaluation before anesthesia, reporting only “painful patients” in need of apicoectomy. The same flaw in study design was found in the study of Parida et al.46 where no pain scores were measured in patients needing tooth extraction. Based on this literature, we could not find an association between local anesthesia and changes in opiorphin levels, and we could not extrapolate the results for direct association between VAS scores and opiorphin level. Further studies are necessary to document this association.
Time course of opiorphin release
Alajbeg et al.27 stimulated the oral mucosa of subjects with capsaicin, and detected no opiorphin release in control subjects but in TMD patients. Although not yet published, this is the first study to document acute release of opiorphin in response to a painful stimulus in humans which seems to occur only in certain conditions. The study of Ozdogan et al.34 also supports the release of opiorphin after a CFB painful stimulus, although with a different time course (hours vs. minutes). It must also be mentioned that local anesthesia, before silencing peripheral nerves, is often accompanied by a pricking pain due to the needle insertion which may also generate stress, and could explain contradictory results. Therefore, more studies related to the time course of opiorphin release after nociceptive stimulation are needed.
Taken together, as the conditions reviewed here include mainly painful and stressful conditions, the data suggest that opiorphin is released in response to pain and/or stressful situations; interestingly, the only study to report a pathological non-painful condition, i.e. oral potentially/malignant conditions8, reported no significant increase of salivary opiorphin levels, thus supporting this assertion.
As a consequence, administration of opiorphin or its analogs might be useful in therapeutics. Indeed, studies suggest an analgesic effect of administration of a dual enkephalinase inhibitors, in animals’ models of ocular pain51 and migraine52.
Influence of different factors on opiorphin release
Various factors have been described that can influence opiorphin levels, such as age and sex30,53, systemic health, use of medications, the most stimulated salivary gland29, the body fluid from which opiorphin is collected30 and psychosocial profile16.
Evidence is already available for higher concentrations of opiorphin in males compared to females53; in younger healthy adults (mean age 26 ± 6 years)53 compared to older ones with BMS (59 ± 12 years)30; in non-pregnant volunteers compared to sixth-month pregnant53; in unstimulated saliva secreted mainly by the submandibular glands compared to stimulated saliva, which is secreted mainly by the parotid glands29; and in serum compared to saliva30. In addition, one study found no correlation between the levels of opiorphin and systemic conditions or drug consumption29. Another important point concerns whether and how the psychosocial status of the patient may alter the salivary opiorphin levels. Patients with anxiety may experience a more negative emotional response to pain and increased susceptibility to stress54. Furthermore, sialorphin increases under acute stress conditions in rats, suggesting that psychosocial status may influence opiorphin levels in human subjects; therefore, studies related to this topic, i.e., different stressful conditions, should be encouraged16,55.
Future directions
The present review emphasizes the need for better study designs and improved clinical information. Multicentric designs should be favored to control for cultural differences. Confounding factors such as age, sex, systemic health, use of medications, the body fluid sampled and the psychosocial profile of patients should all be analyzed, as well as pain levels in control groups, and tests conducted before and after intervention. Initiative on Methods, Measurement, and Pain Assessment in Clinical Trials (IMMPACT) recommendations can provide supportive guidelines56.
This review highlights the lack of knowledge related to physiologic conditions of opiorphin release. Experimental studies in both acute and chronic conditions should be encouraged, as well as dissociating pain and stress effects on opiorphin release. Finally, trials with different types of nociceptive stimulations such as capsaicin can be considered in future studies in order to decipher the mechanisms of opiorphin release in acute and chronic pain.
Conclusions
The results of the present review may not be generalized due to the aforementioned limitations of the included studies, the higher risk of bias in some studies regarding strategies to deal with confounding factors, and very low GRADE level of evidence. Based on the available evidence, this meta-analysis suggests that salivary opiorphin levels are elevated in chronic, sustained and acute pain conditions, reflecting a physiological homeostatic adaptative response to different conditions such as pain and psychic stress. Salivary opiorphin might therefore be used as a valuable biomarker in oral inflammation.
Data availability
All of the data, material and methods which support the results can be found in the article.
References
Williams, A. C. C. & Craig, K. D. Updating the definition of pain. Pain 157(11), 2420–2423 (2016).
Porporatti, A., et al., Prevalence of Orofacial Pain Conditions: An Umbrella Review of Systematic Reviews. PROSPERO 2022 CRD42022377910. https://www.crd.york.ac.uk/prospero/display_record.php?ID=CRD42022377910.
International Classification of Orofacial Pain, 1st edition (ICOP). Cephalalgia, 2020. 40(2): 129–221.
World Health Organization. Global Oral Health Status Report: Towards Universal Health Coverage for Oral Health by 2030 (World Health Organization, 2022).
Peres, M. A. et al. Oral diseases: A global public health challenge. Lancet 394(10194), 249–260 (2019).
Listl, S. et al. Global economic impact of dental diseases. J. Dent. Res. 94(10), 1355–1361 (2015).
Breckons, M. et al. DEEP study: Indirect and out-of-pocket costs of persistent orofacial pain. J. Dent. Res. 97(11), 1200–1206 (2018).
Nejad, N. K. & R.P., Kar A, Sujatha S.,. Quantitative analysis and expression of salivary opiorphin in painful oral soft-tissue conditions: A descriptive study. J. Glob. Oral Health 20, 123–127 (2020).
Fischer, H. P., Eich, W. & Russell, I. J. A possible role for saliva as a diagnostic fluid in patients with chronic pain. Semin. Arthritis Rheum. 27(6), 348–359 (1998).
Jang, M. U. et al. Plasma and saliva levels of nerve growth factor and neuropeptides in chronic migraine patients. Oral Dis. 17(2), 187–193 (2011).
Michela, B. Liquid biopsy: A family of possible diagnostic tools. Diagnostics (Basel) 11, 8 (2021).
Khurshid, Z. et al. Biochemical analysis of oral fluids for disease detection. Adv. Clin. Chem. 100, 205–253 (2021).
Chojnowska, S. et al. Salivary biomarkers of stress, anxiety and depression. J. Clin. Med. 10, 3 (2021).
Wisner, A. et al. Human Opiorphin, a natural antinociceptive modulator of opioid-dependent pathways. Proc. Natl. Acad. Sci. USA 103(47), 17979–17984 (2006).
Nishimura, K. & Hazato, T. Isolation and identification of an endogenous inhibitor of enkephalin-degrading enzymes from bovine spinal cord. Biochem. Biophys. Res. Commun. 194(2), 713–719 (1993).
Rougeot, C. et al. Selective processing of submandibular rat 1 protein at dibasic cleavage sites. Salivary and bloodstream secretion products. Eur. J. Biochem. 219(3), 765–773 (1994).
Rougeot, C. et al. Sialorphin, a natural inhibitor of rat membrane-bound neutral endopeptidase that displays analgesic activity. Proc. Natl. Acad. Sci. USA 100(14), 8549–8554 (2003).
Popik, P. et al. Human opiorphin: The lack of physiological dependence, tolerance to antinociceptive effects and abuse liability in laboratory mice. Behav. Brain Res. 213(1), 88–93 (2010).
Javelot, H. et al. Human opiorphin is a naturally occurring antidepressant acting selectively on enkephalin-dependent delta-opioid pathways. J. Physiol. Pharmacol. 61(3), 355–362 (2010).
Rougeot, C. et al. Systemically active human opiorphin is a potent yet non-addictive analgesic without drug tolerance effects. J. Physiol. Pharmacol. 61(4), 483–490 (2010).
Van Elstraete, A. et al. The opiorphin analog STR-324 decreases sensory hypersensitivity in a rat model of neuropathic pain. Anesth. Analg. 126(6), 2102–2111 (2018).
Mathison, R. D. et al. Autonomic regulation of anti-inflammatory activities from salivary glands. Chem. Immunol. Allergy 98, 176–195 (2012).
Sessle, B. J. Peripheral and central mechanisms of orofacial inflammatory pain. Int. Rev. Neurobiol. 97, 179–206 (2011).
Shrivastava, M., Battaglino, R. & Ye, L. A comprehensive review on biomarkers associated with painful temporomandibular disorders. Int. J. Oral Sci. 13(1), 23 (2021).
Liu, Q. et al. Transcriptional alterations of mouse trigeminal ganglion neurons following orofacial inflammation revealed by single-cell analysis. Front. Cell Neurosci. 16, 885569 (2022).
Korczeniewska, O. A. et al. Pathophysiology of post-traumatic trigeminal neuropathic pain. Biomolecules 12, 12 (2022).
Alajbeg, I., Oxidative stress and opiorphin in temporomandibular disorders (ROStrO-TMD). 2017: ClinicalTrials.gov Identifier: NCT03029494.
Orabović, I. et al. Salivary Opiorphins as a response to Capsaicin stimulation: A comparison of Temporomandibular Disorder patients and healthy controls. Acta Stomatol. Croat. 55(2), 213–236 (2021).
Salarić, I., Sabalić, M. & Alajbeg, I. Opiorphin in burning mouth syndrome patients: A case–control study. Clin. Oral Investig. 21(7), 2363–2370 (2017).
Boucher, Y. et al. Opiorphin levels in fluids of burning mouth syndrome patients: A case–control study. Clin. Oral Investig. 21(7), 2157–2164 (2017).
Ozdogan, M. S. et al. Salivary opiorphin in dental pain: A potential biomarker for dental disease. Arch. Oral Biol. 99, 15–21 (2019).
Paszynska, E. et al. Is there a link between stress and immune biomarkers and salivary opiorphin in patients with a restrictive-type of anorexia nervosa?. World J. Biol. Psychiatry 21(3), 220–229 (2020).
Paszynska, E. et al. Salivary opiorphin levels in anorexia nervosa: A case–control study. World J. Biol. Psychiatry 21(3), 212–219 (2020).
Ozdogan, S. et al. Tear opiorphin levels in ocular pain caused by corneal foreign body. Cornea 39(11), 1377–1380 (2020).
Davies, K. P. The role of opiorphins (endogenous neutral endopeptidase inhibitors) in urogenital smooth muscle biology. J. Sex Med. 6(Suppl 3), 286–291 (2009).
Kanika, N. D., Melman, A. & Davies, K. P. Experimental priapism is associated with increased oxidative stress and activation of protein degradation pathways in corporal tissue. Int. J. Impot. Res. 22(6), 363–373 (2010).
Tong, Y. et al. The opiorphin gene (ProL1) and its homologues function in erectile physiology. BJU Int. 102(6), 736–740 (2008).
Al-Saffar, M. T., Al-Sandook, T. A. & M. Y-Taha,. A possible new concept in the mechanism of action of local anesthesia. Am. J. Med. Biol. Res. 1(4), 134–137. https://doi.org/10.12691/ajmbr-1-4-5 (2013).
Ruangri, S., Jorns, T. P. & Chaiyarit, P. Opiorphin level in unstimulated whole saliva of burning mouth syndrome patients. J. Med. Assoc. Thailand 102(4), 63 (2019).
Page, M. J. et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 372, 71. https://doi.org/10.1136/bmj.n71 (2021).
Needleman, I. G. A guide to systematic reviews. J. Clin. Periodontol. 29(Suppl 3), 6–9 (2002) (discussion 37–8).
Tufanaru, C. M. Z., Aromataris, E., Campbell, J., & Hopp, L. Chapter 3: Systematic reviews of effectiveness. In JBI Manual for Evidence Synthesis (Aromataris, E., Munn, Z., ed) (JBI, 2020). https://synthesismanual.jbi.global.
Moola, S. M. Z., et al. Chapter 7: Systematic reviews of etiology and risk . In JBI Manual for Evidence Synthesis (Aromataris, E., & Munn, Z. eds.) (JBI, 2020). https://synthesismanual.jbi.global.
Briggs, I. J. JBI Critical Appraisal Checklist for Analytical Prevalence Studies (The Joanna Briggs Institute, 2016).
Higgins, J., Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0. http://handbook.cochrane.org/ (The Cochrane Collaboration, 2011).
Parida, S. K. et al. A study of salivary opiorphin levels using different anesthetic drugs and techniques—a randomized controlled clinical study. J. Stomatol. Oral Maxillofac. Surg. 119(3), 169–171 (2018).
Boucher, Y. et al. Opiorphin levels in fluids of burning mouth syndrome patients: A case–control study. Clin. Oral Invest. 21(7), 2157–2164 (2016).
Brkljačić, L. et al. Development and validation of a liquid chromatography-tandem mass spectrometry method for the quantification of opiorphin in human saliva. J. Chromatogr. B Analyt. Technol. Biomed. Life Sci. 879(32), 3920–3926 (2011).
Accioni, F., García-Gómez, D. & Rubio, S. Exploring polar hydrophobicity in organized media for extracting oligopeptides: Application to the extraction of opiorphin in human saliva. J. Chromatogr. A 1635, 461777 (2021).
Porporatti, A. L. et al. Is burning mouth syndrome associated with stress? A meta-analysis. J. Oral. Rehabil. 20, 23 (2023).
Reaux-Le Goazigo, A. et al. Dual enkephalinase inhibitor PL265: A novel topical treatment to alleviate corneal pain and inflammation. Pain 160(2), 307–321 (2019).
Mei, H. R. et al. Efficacy of dual enkephalinase inhibition in a preclinical migraine model is mediated by activation of peripheral delta opioid receptors. Headache 63(5), 621–633 (2023).
Dufour, E. et al. Opiorphin secretion pattern in healthy volunteers: Gender difference and organ specificity. Biochem. Anal. Biochem. 2, 136. https://doi.org/10.4172/2161-1009.1000136 (2013).
Asmundson, G. J. & Katz, J. Understanding the co-occurrence of anxiety disorders and chronic pain: State-of-the-art. Depress Anxiety 26(10), 888–901 (2009).
Anna, K. et al. Salivary biomarkers (opiorphin, cortisol, amylase, and IgA) related to age, sex, and stress perception in a prospective cohort of healthy schoolchildren. Mediat. Inflamm. 20, 20 (2021).
Turk, D. C. et al. Identifying important outcome domains for chronic pain clinical trials: An IMMPACT survey of people with pain. Pain 137(2), 276–285 (2008).
Acknowledgements
The authors declare they received no funding for this research.
Author information
Authors and Affiliations
Contributions
A.L.P. worked on study conceptualization, design, data collection, data analysis, drafted the initial manuscript, and approved the final manuscript as submitted. He was the first reviewer. C.A.O.M. worked on study conceptualization, design, data collection, data analysis, and approved the final manuscript as submitted. She was the second reviewer. I.A. worked on study conceptualization, design, data collection, data analysis, and approved the final manuscript as submitted. I.A. worked on study conceptualization, design, data collection, data analysis, and approved the final manuscript as submitted. E.P. worked on study conceptualization, data analysis and critically reviewed the manuscript, and approved the final manuscript as submitted. M.D.-W. worked on study conceptualization, data analysis and critically reviewed the manuscript, and approved the final manuscript as submitted. A.B. worked on study conceptualization, data analysis and critically reviewed the manuscript, and approved the final manuscript as submitted. Y.B. worked on study conceptualization, design, data analysis, drafted the initial manuscript, and approved the final manuscript as submitted.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Porporatti, A.L., de Oliveira Machado, C.A., Alajbeg, I. et al. Opiorphin as a biomarker of orofacial conditions: a meta-analysis. Sci Rep 13, 15533 (2023). https://doi.org/10.1038/s41598-023-42051-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-023-42051-y
This article is cited by
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.