Abstract
Medial meniscal extrusion (MME) is a structural abnormality that leads to early knee osteoarthritis; however, its formation remains debated. For anatomical consideration of the mechanism underlying MME formation, we examined the capsular attachment on the posteromedial tibia and its layered association with the semimembranosus. Fourteen knees of eight body donors were analyzed in this study; six knees were grouped for macroscopic analysis, whereas four knees each were grouped for histological and phosphotungstic acid-enhanced micro-computed tomography analyses. The capsular attachment varied in width according to location and was not distant from the articular cartilage and posterior root. A portion of the posteromedial joint capsule formed the semimembranosus tendinous sheath. The dense fibrous membrane superficial to the semimembranosus, which was continuous from its tendinous sheath, existed as one of the layers of the joint capsule. The aforementioned findings were confirmed in all specimens. Based on the capsular attachment and its layered association with the semimembranosus, the conventional posteromedial knee ligaments may be only a part of the joint capsule divided into two layers by the semimembranosus. If the coordinated action of the joint capsule and semimembranosus partially contributes to the medial meniscus stability, such a structural problem may affect MME formation.
Similar content being viewed by others
Introduction
It is challenging to elucidate the mechanisms for initiation/progression of early knee osteoarthritis in order to establish prevention methods. Medial meniscal extrusion (MME) is the displacement of the medial meniscus from the tibial articular cartilage or the uncovering of the tibial articular cartilage by the medial meniscus; it is one of the structural abnormalities believed to be associated with the initiation and progression of knee osteoarthritis1,2,3. However, the origins and pathophysiology of MME formation itself remain debated. Previous studies have reported that posterior root tears of the medial meniscus4,5,6 and osteophyte formation at the medial tibia7,8 contribute to MME formation. However, these conditions may have occurred after prolonged degeneration9 or repetitive stress10,11; therefore, it is preferable to consider other mechanisms of pathological initiation that can be targeted for early prevention of MME. Moreover, to gain a more comprehensive picture of MME formation, precise anatomical knowledge regarding medial meniscus stabilization may be essential.
There are two types of joint stabilization mechanisms: static (provided by the surrounding ligaments) and dynamic (provided by the adjacent muscles). Regarding the static stabilizer of the medial meniscus, studies have focused on the posteromedial ligaments and their tibial attachment, including the superficial medial collateral ligament (sMCL; also known as the tibial collateral ligament), deep medial collateral ligament (dMCL), posterior oblique ligament (POL), and meniscotibial (coronary) ligament (MTL)12,13,14,15,16,17. Regarding the dynamic stabilizer, most studies have concentrated on the semimembranosus15,18,19. However, the capsular attachment on the posteromedial tibia has rarely been investigated despite the medial meniscus forming a complex with the joint capsule12,20. In addition, the layered structure in the joint capsule and pericapsular muscles is useful in understanding the interrelationships between the static and dynamic stabilizers in most joints21, including the knee22,23. The semimembranosus can be regarded as the knee pericapsular muscle and has been well discussed regarding its connection to the joint capsule15,18,19. However, their layered relationships remain unclear due to the lack of histological analysis, which has only been analyzed macroscopically14. For example, while the sMCL and dMCL form two layers on the medial side of the knee12,14,15,16, whether the joint capsule forms a separate layer from these layers is unknown. Furthermore, where the semimembranosus locates against these two layers on the posteromedial side of the knee and whether it is more superficial or deep than the joint capsule is unclear (Fig. 1). It is difficult to observe uninterrupted continuous sections during histological analysis; however, this limitation can be compensated by phosphotungstic acid-enhanced micro-computed tomography (micro-CT) analysis, which can obtain any sectional information of the soft tissue24,25,26,27,28.
Conventional understanding of the support structures for the medial meniscus at the medial and posteromedial knees. Schematic illustration of the cross sections at the medial (left panel) and posteromedial (right panel) knees. The superficial and deep medial collateral ligaments (sMCL and dMCL, respectively) form two layers on the medial side of the knee, and the medial meniscus (MM) attaches to the tibia via the meniscotibial ligament (MTL). However, whether the joint capsule is located at a separate layer from these two layers and where the joint capsule attaches are not well understood. Additionally, where the semimembranosus (Sm) locates against these two layers on the posteromedial side of the knee, and whether it is more superficial or deep than the joint capsule is unknown. Med Medial, Post/Med Posteromedial, Sup Superior.
This study aimed to investigate the capsular attachment on the posteromedial tibia and its layered association with the semimembranosus using an integrated multidimensional analysis incorporating macroscopic, histological, and micro-CT analyses. We hypothesized that the capsular attachment on the posteromedial tibia varied according to location and the layered relationships between the semimembranosus and joint capsule might suggest the presence of interrelationships between the static and dynamic stabilizers of the medial meniscus.
Results
Macroscopic analysis showing semimembranosus and posteromedial capsular attachment on the tibia
On the posteromedial aspect of the knee, the insertion tendon of the semimembranosus was covered with a tendinous sheath (Fig. 2a). This tendinous sheath comprised a part of the joint capsule and continued to the tendinous membrane, which is located anterior to the semimembranosus tendon (Fig. 2b). In the superficial layer of the semimembranosus, cord-like structures completely independent of the tendinous membrane were not observed. The tendinous membrane and anterior edge of the semimembranosus were separated from each other by the synovial bursa but were partly connected to the posterior portion of the semimembranosus (Fig. 2c). The semimembranosus was attached to the superior edge of the posteromedial tibia with a distinct bony impression (Fig. 2d and Supplementary Fig. S1). The above findings (Fig. 2a–d) were observed in all six knees examined macroscopically (i.e., in all specimens).
Semimembranosus attachment on the superior edge of the tibia and its tendinous sheath. The posteromedial aspect of the right knee. (a) The distal tendon of the semimembranosus (Sm) is covered with its tendinous sheath. (b) After cutting through the superior margin of the tendinous sheath, the distal Sm tendon is partially exposed. The tendinous sheath comprises a part of the joint capsule and continues to the tendinous membrane anterior to the Sm tendon. The synovial bursa (sharp) is located between the anterior edge of the Sm and the tendinous membrane. (c) By detaching the tibial attachment of the tendinous membrane (white dotted line), it becomes continuous with the posterior portion of the Sm (arrowheads). (d) The Sm partially attaches on the superior edge of the tibia (star), and this attachment is located superior to the inferior medial genicular artery (arrows). Po Popliteus, calcaneus, Lat Lateral, Post Posterior, Sup Superior.
On the posterior aspect of the knee, the semimembranosus tendon was also continuous with the posterior joint capsule (Fig. 3a). The joint capsule was attached to the posteromedial tibia with widths that varied according to location. The medial meniscus was continuous with the joint capsule over the entire circumference, and its posterior root area, which is anterior to the posterior cruciate ligament, was also not independent of the capsular attachment area on the tibia (Fig. 3b,c). The above findings were also observed in all six specimens.
Posteromedial capsular attachment on the superior edge of the tibia. (a) Posterior aspect of the right knee. The semimembranosus (Sm) tendon is continuous with the posterior joint capsule (Cap) and superficial tendinous membrane of the popliteus (Po). (b) After removal of the popliteus, the Cap complex with the Sm is detached from the superior edge of the tibia (white dotted line). (c) After detaching the posterior cruciate ligament (PCL), the posterior horn of the medial meniscus (MM) is detached from the tibia to detach the Cap more medially. The posterior root area (triangle) is continuous with the posterior Cap attachment area. (d) Medial aspect of the knee. After detaching the Cap anteriorly to the Sm attachment (star), its attachment widths were measured at the anterior and posterior edges of the Sm attachment (L1 and L3), and the minimum width was measured superior to the Sm attachment (L2). Lat Lateral, Post Posterior, Sup Superior.
The widths of capsular attachment significantly varied according to location [one-way analysis of variance (ANOVA), p < 0.001; anterior to the semimembranosus attachment (Fig. 3d, L1 = 15.1 ± 1.5 mm) vs. superior to the semimembranosus attachment (Fig. 3d, L2 = 5.4 ± 1.7 mm), p < 0.001; L2 vs. posterior to the semimembranosus attachment (Fig. 3d, L3 = 12.6 ± 2.0 mm), p < 0.001]. The width of the capsular attachment was relatively wide posterior to the semimembranosus attachment on the superior edge of the tibia, decreased superior to the semimembranosus attachment, and increased anterior to the semimembranosus attachment in all specimens (Fig. 3d). The width measurements are summarized in Table 1.
Histological and micro-CT analyses showing the layered relationships between the semimembranosus and posteromedial joint capsule
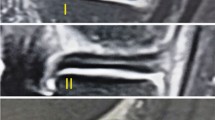
The joint capsule was confirmed to be not histologically independent of the medial meniscus over the entire circumference (Fig. 4a–f). The joint capsule was attached to the posteromedial tibia via fibrocartilage, even where the width of the capsular attachment was narrow (Fig. 4d,e). In addition, the upper margin of the capsular attachment reached the lower margin of the articular cartilage without a gap in any histological section. The semimembranosus was in close contact with the posterior joint capsule (Fig. 4b) and was gradually covered by a loose tendinous sheath at the posteromedial region (Fig. 4c). Furthermore, it was completely covered by a dense fibrous sheath, which was continuous with the posteromedial joint capsule from the posterior to the anterior edge of the proximal tibial attachment (Fig. 4d,e). At the medial side of the tibia anterior to the semimembranosus attachment, the dense fibrous membrane, which was also continuous with the joint capsule, occupied the same layer as the dense fibrous sheath of the semimembranosus (Fig. 4f). The above-mentioned histological findings were based on sagittal and coronal sections of different specimens; however, the radial sequential images obtained from the micro-CT analysis confirmed the layered characteristics from the posterior to medial knee in the same specimen (Fig. 5 and Supplementary Video S1).
Histological analysis of the joint capsule and semimembranosus (Masson’s trichrome staining). Schematic illustration (a), the posteromedial aspect of the right medial knee, indicates histological section locations in sagittal (b and c) and coronal sections (d–f). The joint capsule (Cap) is not histologically independent from the medial meniscus (MM) and attaches to the superior edge of the tibia without any distance from the articular cartilage. The semimembranosus (Sm) is in close contact with the posterior Cap (b); it is gradually covered by a loose tendinous sheath at the posteromedial region (c) and completely covered by a dense fibrous sheath continuous with the Cap at the proximal tibial attachment (Star, d, e). Scale bars = 2.5 mm. Gcm Medial head of the gastrocnemius, Gr Gracilis, MIT Medial intercondylar tubercle, PCL Posterior cruciate ligament, Po Popliteus, Sa Sartorius, St Semitendinosus, Triangle Posterior root area of the MM, Inf Inferior, Med Medial, Lat Lateral, Post Posterior, Sup Superior.
Serial radial sections of the joint capsule and semimembranosus using phosphotungstic acid-enhanced micro-CT. Horizontal enhanced micro-CT image using phosphotungstic acid (a) indicates the radial slice locations centered around the medial intercondylar tubercle (MIT) for visualizing the following sections: images with 15° (b), 30° (c), 45° (d), 75° (e), 90° (f) clockwise from sagittal sections. Scale bars = 5 mm. Cap Joint capsule, Gcm Medial head of the gastrocnemius, Gr Gracilis, MM Medial meniscus, Po Popliteus, Sa Sartorius, Sm Semimembranosus, St Semitendinosus, Star Sm attachment on the superior edge of the tibia, Ant Anterior, Lat Lateral.
Discussion
The present study revealed that the capsular attachment width was wide posterior and anterior to the semimembranosus attachment on the superior edge of the tibia and narrow superior to the semimembranosus attachment. This attachment was not independent of the posterior root of the medial meniscus and was histologically close to the articular cartilage. A portion of the posteromedial joint capsule formed the semimembranosus tendinous sheath. This tendinous sheath gradually became dense fibrous tissue from the posterior to the medial and continued to the dense fibrous membrane as one of the layers of the joint capsule. The medial meniscus was attached to the tibia through the joint capsule and was continuous with the joint capsule over the entire circumference. Our main findings were summarized in Fig. 6.
The layered structure of the joint capsule and semimembranosus. Schematic illustration of the cross sections at the medial (left panel) and posteromedial (right panel) knees. The medial meniscus (MM) attached to the tibia via the joint capsule (Cap), with the attachment varying in width according to location and not distant from the articular cartilage. A part of the posteromedial Cap forms the tendinous sheath of the semimembranosus (Sm). The fibrous membrane superficial to the Sm, which is continuous from the Sm tendinous sheath, exists as one of the layers of the Cap (indicated by red circles). The red diamonds also indicate the corresponding layer of the Cap. Med Medial, Post/Med Posteromedial, Sup Superior.
The capsular attachment in the present study varied in width according to location (range, approximately 5–15 mm) and was not distant from the articular cartilage and posterior root. In a previous report regarding capsular attachment, Warren and Marshall reported, “its lines of attachment above and below the joint are essentially the same as the margins of the articular surfaces”14. Therefore, our results were consistent with the previous study regarding distance to the articular cartilage but differ in terms of the attachment width, which was not linear, and focusing on the proximity to the posterior root. This discrepancy may be attributed to the conventional viewpoint that only the synovial membrane, which constitutes the joint capsule, has been considered the joint capsule, while the fibrous membrane of the joint capsule, is regarded as the MTL. Thus, the general emphasis is that the medial meniscus attaches to the tibia through the MTL rather than the joint capsule20. Additionally, the width of the MTL attachment has been considered to vary between 9 and 17 mm according to location18 and was approximately the same as that of the capsular attachment reported in this study. Because the synovial membrane closely lines the fibrous membrane in most articular systems29, it is improbable that synovial and fibrous membranes could independently move during knee movement. Therefore, it is anatomically and possibly functionally accurate to interpret the medial meniscus as attached to the tibia via the joint capsule, with the capsular attachment being continuous with the posterior root, rather than assuming that the medial meniscus attaches to the tibia via the MTL.
We showed that a dense fibrous membrane continuous from the semimembranosus tendinous sheath was a layer of the joint capsule. Warren and Marshall14 reported the sMCL as superficial to the semimembranosus instead of identifying this fibrous membrane reported in our study. Regarding this fibrous membrane, previous studies have reported similar structures continuous with the sMCL12,30. Furthermore, many studies have shown that the sMCL can be separated from the joint capsule12,14,15,16; however, these studies only pointed out the differences in the layers, with none reporting the clear anterior and posterior boundaries with surrounding structures. Therefore, on the basis of the observed layered relationships, the sMCL may be interpreted as a part of the dense fibrous membrane that is continuous from the semimembranosus tendon sheath rather than a distinct cord-like structure.
Distinct cord-like structures like the dMCL in the same layer as the capsule14 and those like the POL surrounding the semimembranosus13,15 were not observed in the present study, unlike that in previous studies. As most studies have pointed out, the dMCL is interpreted as a constituent of the joint capsule14,15,16; the POL is merely a subdivision, based on its proximal attachment, of what was originally considered the sMCL13,15. Therefore, the “posteromedial knee ligaments” may be nothing more than a regionally named structure that is a joint capsule divided into two layers by the tendon.
Regarding clinical relevance, the present study provided two hypothetical insights regarding MME formation. First, the present study suggested that the medial meniscus may be cooperatively stabilized by the posterior root and joint capsule based on the continuity between the posterior root and capsular attachment. A recent meta-analysis and systematic review suggested that surgical repair of the posterior root biomechanically improved knee contact pressure but did not clinically improve the MME31. Therefore, the posterior root is not considered to support the meniscus independently. The peripheral capsule yielded a smaller tensile modulus than did the meniscus itself or the posterior root32,33; however, the peripheral capsule was suggested to have a sufficient role in maintaining the circumferential hoop tension of the meniscus32. Additionally, the disruption of the MTL, namely the capsular attachment on the tibia, was reported to have a biomechanically significant effect on knee stability34,35. According to Krych et al., the disruption of the MTL was a predisposing event that contributed to the posterior root tears of the medial meniscus36. Therefore, a capsular abnormality may trigger the accumulation of mechanical stress on the posterior root and its tear, although the contribution of the capsular abnormality to MME is assumed to be smaller than that of the posterior root.
Second, according to Hada et al., the medial tibial osteophyte in early knee osteoarthritis occurred close to the articular cartilage and was closely associated with the MME7. The present study revealed that the joint capsule was attached close to the articular cartilage where osteophytes can form; therefore, a capsular abnormality may precede osteophyte formation. Because the medial meniscus was continuous with the joint capsule, which formed the semimembranosus tendinous sheath, the joint capsule may dynamically coordinate the medial meniscus by transmitting semimembranosus action through the tendinous sheaths. Therefore, based on our interpretation that existing ligaments are part of a joint capsule, the dynamic and static stabilizers of the medial meniscus may cooperatively function. We believe structural abnormalities of the joint capsule precede the posterior root tear or osteophyte formation.
This study had some limitations. First, this study was purely anatomical and limited to uninjured specimens; therefore, we could not prove the mechanism of MME formation, and our explanations remain speculative. Since the structural abnormalities of the joint capsule might be interpreted as an early causative factor for MME, examining these abnormalities in depth will be essential in the future. For example, questions on whether MME formation is caused by an attachment abnormality, such as one involving the synovial membrane, or whether MME formation is associated with the semimembranosus should be investigated. Second, the sample size was relatively small. However, we compensated for the small sample size with a multidimensional analysis, which included macroscopic, histological, and micro-CT analyses. Third, the lack of radiographic evaluation meant we could not entirely exclude the knee with osteoarthritis despite this study aiming to analyze the normal structure. Finally, the advanced age of the individuals from whom the cadaveric specimens were obtained might have affected our findings. However, this effect may be negligible because patients with knee osteoarthritis are also often relatively old.
In conclusion, the capsular attachment on the posteromedial tibia varied in width according to location and was not distant from the posterior root. The joint capsule formed the semimembranosus tendinous sheath, and the conventional posteromedial knee ligaments may only be a part of the joint capsule divided into two layers by the semimembranosus tendon. If the coordinated action of the joint capsule and semimembranosus partially contributes to the medial meniscus stability, such a structural problem may affect MME formation.
Methods
Specimen preparation
Sixteen knees from ten Japanese body donors (six males and four females; mean age at death: 80.9 years) donated to the Department of Anatomy at Tokyo Medical and Dental University were used in this study. Before their death, all donors voluntarily declared that their remains be donated for education and research. This study complied with the Japanese law entitled “Act on Body Donation for Medical and Dental Education,” and the study design was approved by the Medical Research Ethics Committee of Tokyo Medical and Dental University (approval no.: #M2018-243-01). In addition, all procedures were performed in accordance with the Japanese guidelines entitled “Ethical Guidelines for Medical and Health Research Involving Human Subjects”.
The anatomic specimens without surgical history in the lower extremity were included in this study, fixed with 8% formalin, and preserved in 30% ethanol. Using a diamond saw (EXAKT 312; EXAKT Advanced Technologies, Norderstedt, Germany), the knee specimens were obtained by cutting proximal at the center of the patella and distal at the superior one-third of the tibia. Then, the medial half of the knee was acquired by cutting off the lateral half, leaving the medial meniscus undamaged. Based on the half-sectioned aspect, all specimens were macroscopically assessed for distinct intra-articular abnormalities such as osteoarthritis changes. In addition, the sectioned specimens underwent micro-CT (inspeXio SMX-100CT; Shimadzu, Kyoto, Japan) with a 200-µm resolution to determine if any bony abnormalities were present. From the series of micro-CT images, three-dimensional reconstruction images were obtained using ImageJ software version 1.53 (National Institutes of Health, Bethesda, MD, USA). Two knees of two cadavers were excluded from the analysis because of osteoarthritis changes observed during the macroscopic and micro-CT assessment of the specimens.
Therefore, 14 knees of eight body donors (five males and three females; mean age at death: 78.6 years) were finally analyzed in this study. Six knees of four body donors were randomly grouped for macroscopic analysis, whereas the remaining eight knees of four body donors were grouped for histological (one side of each donor) and phosphotungstic acid-enhanced micro-CT (the other side of each donor) analyses.
Macroscopic analysis of the posteromedial region of the tibia
For the macroscopic analysis (six knees; three males and one female; mean age at death: 82.8 years), the skin and subcutaneous tissues, muscles comprising the pes anserinus (sartorius, gracilis, and semitendinosus), and medial head of the gastrocnemius were removed. The femur was also removed from the specimen by detaching its capsular attachment. Then, we analyzed the layered relationships and connection to the semimembranosus, joint capsule, and medial meniscus and their attachments to the posteromedial region of the tibia. In addition, the attachment width of the joint capsule on the posteromedial tibia was measured. Measurements were performed twice by a single examiner, and the average of two measurements was recorded for statistical analysis. Intraclass correlation coefficients (ICCs) were calculated to determine the intra-rater reliability of each measured value.
Histological analysis of the posteromedial region of the knee
The four knees (two males and two females; mean age at death: 74.5 years) grouped for histological analysis were embedded in a 3% agar solution and frozen at − 80 °C. Two specimens were then serially sectioned into 5-mm thick segments in the sagittal plane using a band saw (WN-25-3; Nakajima Seisakusho, Osaka, Japan), whereas the remaining two knees were sectioned in the coronal plane. Each section level was identified based on the correspondence between the section bony morphology and that observed on the micro-CT image at the specimen preparation. After removing the excess agar, we chose two sagittal sections at the following levels: immediately medial to the posterior cruciate ligament and its adjacent section, and three coronal sections: posterior and anterior edges of the semimembranosus attachment to the superior end of the tibia and the section anterior to the semimembranosus attachment. Subsequently, we harvested a block from each section, including the semimembranosus, joint capsule, and medial meniscus; the blocks were decalcified for 3 weeks with Plank–Rychlo solution (AlCl3:6H2O [70.0 g/L], HCl [85.0 mL/L], and HCOOH [50.0 mL/L])37. After decalcification, each block was dehydrated and embedded in paraffin. The paraffin-embedded tissue was sliced into 5 μm sections with a 1-mm interval; the sections were stained using the Masson trichrome staining protocol.
Analysis of the posteromedial region of the knee using phosphotungstic acid-enhanced micro-CT
Four knees were analyzed using phosphotungstic acid-enhanced micro-CT. The specimens were dehydrated in 70% ethanol solutions for a day and then stained with 1% phosphotungstic acid solution in 70% ethanol for 16–20 weeks. The stained specimens can acquire bony and soft tissue three-dimensional information using micro-CT, and even a single specimen allows cross-sectional observation in various planes24,25,26,27,28. The specimens were scanned using micro-CT with a 50-µm resolution (an image pixel size of 50 μm with 1024 × 1024 pixels). The scanned sequential images were re-sliced to be horizontal to the superior articular surface of the tibia using the ImageJ software. Then, using the “Radial slice” plugin of ImageJ software, the radial sequential images perpendicular to the articular surface were obtained. The radial slice plane was rotated clockwise at 1° intervals around the medial intercondylar tubercle in the posteromedial quadrant range (Supplementary Video S1).
Statistical analyses
In six knees undergoing macroscopic analysis, statistical comparisons of the attachment widths of the joint capsule were performed using SPSS software version 27.0 (IBM Corp., Armonk, NY, USA). Distributions of all measurements consistently passed the Shapiro–Wilk test, and the data are expressed as mean and standard deviation. The comparisons of the attachment widths were analyzed using a one-way ANOVA. If the one-way ANOVA produced a significant result, the values for the regions were compared using post hoc Tukey's test. Both significance levels of the comparisons were set at p < 0.05. In addition, the effect size was calculated using G*Power software version 3.1.9.6, and post-hoc power analysis was performed. The effect size and power were 0.87 and > 0.99, respectively.
ICCs were also determined using a measurement process analysis. The qualitative cut-offs for ICCs are reported as follows: poor, < 0.40; fair, 0.40–0.59; good, 0.60–0.74; and excellent, 0.75–1.038. All ICCs of the capsular attachment width were ≥ 0.89 (range, 0.89–1.000), indicating excellent agreement.
Data availability
The datasets used and/or analyzed during the current study are available from the corresponding author upon reasonable request.
References
Adams, J. G., McAlindon, T., Dimasi, M., Carey, J. & Eustace, S. Contribution of meniscal extrusion and cartilage loss to joint space narrowing in osteoarthritis. Clin. Radiol. 54, 502–506 (1999).
Gale, D. R. et al. Meniscal subluxation: Association with osteoarthritis and joint space narrowing. Osteoarthr. Cartil. 7, 526–532 (1999).
Badlani, J. T., Borrero, C., Golla, S., Harner, C. D. & Irrgang, J. J. The effects of meniscus injury on the development of knee osteoarthritis: Data from the osteoarthritis initiative. Am. J. Sports Med. 41, 1238–1244 (2013).
Costa, C. R., Morrison, W. B. & Carrino, J. A. Medial meniscus extrusion on knee MRI: Is extent associated with severity of degeneration or type of tear?. AJR Am. J. Roentgenol. 183, 17–23 (2004).
Bhatia, S., LaPrade, C. M., Ellman, M. B. & LaPrade, R. F. Meniscal root tears: Significance, diagnosis, and treatment. Am. J. Sports Med. 42, 3016–3030 (2014).
Cinque, M. E. et al. Meniscal root tears: A silent epidemic. Br. J. Sports Med. 52, 872–876 (2018).
Hada, S. et al. Association of medial meniscal extrusion with medial tibial osteophyte distance detected by T2 mapping MRI in patients with early-stage knee osteoarthritis. Arthritis Res. Ther. 19, 201 (2017).
Sekiya, I. et al. Medial tibial osteophyte width strongly reflects medial meniscus extrusion distance and medial joint space width moderately reflects cartilage thickness in knee radiographs. J. Magn. Reson. Imaging 56, 824–834 (2022).
Park, D. Y. et al. The degeneration of meniscus roots is accompanied by fibrocartilage formation, which may precede meniscus root tears in osteoarthritic knees. Am. J. Sports Med. 43, 3034–3044 (2015).
Kawaguchi, H. Endochondral ossification signals in cartilage degradation during osteoarthritis progression in experimental mouse models. Mol. Cells 25, 1–6 (2008).
Saito, T. & Kawaguchi, H. HIF-2alpha as a possible therapeutic target of osteoarthritis. Osteoarthr. Cartil. 18, 1552–1556 (2010).
Brantigan, O. C. & Voshell, A. F. The tibial collateral ligament: Its function, its bursae, and its relation to the medial meniscus. JBJS 25, 121–131 (1943).
Hughston, J. C. & Eilers, A. F. The role of the posterior oblique ligament in repairs of acute medial (collateral) ligament tears of the knee. J. Bone Jt. Surg. Am. 55, 923–940 (1973).
Warren, L. F. & Marshall, J. L. The supporting structures and layers on the medial side of the knee: An anatomical analysis. J. Bone Jt. Surg. Am. 61, 56–62 (1979).
LaPrade, R. F. et al. The anatomy of the medial part of the knee. J. Bone Jt. Surg. Am. 89, 2000–2010 (2007).
Smigielski, R., Becker, R., Zdanowicz, U. & Ciszek, B. Medial meniscus anatomy-from basic science to treatment. Knee Surg. Sports Traumatol. Arthrosc. 23, 8–14 (2015).
Mameri, E. S. et al. Review of meniscus anatomy and biomechanics. Curr. Rev. Musculoskelet. Med. 15, 323–335 (2022).
DePhillipo, N. N. et al. Quantitative and qualitative assessment of the posterior medial meniscus anatomy: Defining meniscal ramp lesions. Am. J. Sports Med. 47, 372–378 (2019).
Cavaignac, E. et al. What is the relationship between the distal semimembranosus tendon and the medial meniscus? A gross and microscopic analysis from the SANTI study group. Am. J. Sports Med. 49, 459–466 (2021).
Spinner, R. J., Krych, A. J. & Bernard, C. D. Knee and leg. In Gray’s Anatomy: The Anatomical Basis of Clinical Practice (ed. Standring, S.) 1395–1429 (Elsevier Health Sciences, 2021).
Tsutsumi, M., Nimura, A. & Akita, K. Clinical anatomy of the musculoskeletal system in the hip region. Anat. Sci. Int. 97, 157–164 (2022).
Nasu, H., Nimura, A., Yamaguchi, K. & Akita, K. Morphology of the anterolateral ligament: A complex of fibrous tissues spread to the anterolateral aspect of the knee joint. Anat. Sci. Int. 95, 470–477 (2020).
Tharnmanularp, S. et al. Medial patellofemoral ligament is a part of the vastus medialis obliquus and vastus intermedius aponeuroses attaching to the medial epicondyle. Knee Surg. Sports Traumatol. Arthrosc. 30, 3742–3750 (2022).
Jehoon, O., Kwon, H. J., Choi, Y. J., Cho, T. H. & Yang, H. M. Three-dimensional structure of the orbicularis retaining ligament: An anatomical study using micro-computed tomography. Sci. Rep. 8, 17042. https://doi.org/10.1038/s41598-018-35425-0 (2018).
Cho, T. H. et al. Interfascicular septum of the calcaneal tunnel and its relationship with the plantar nerves: A cadaveric study. Clin. Anat. 32, 877–882 (2019).
Hur, M. S., Lee, S., Kang, T. M. & Oh, C. S. The three muscle layers in the pyloric sphincter and their possible function during antropyloroduodenal motility. Sci. Rep. 11, 20094. https://doi.org/10.1038/s41598-021-99463-x (2021).
Yang, S. Y., Kim, H. S., Cho, M. S. & Kim, N. K. Three-dimensional anatomy of the Denonvilliers’ fascia after micro-CT reconstruction. Sci. Rep. 11, 21759. https://doi.org/10.1038/s41598-021-01106-8 (2021).
Tsutsumi, M., Kudo, S., Nimura, A. & Akita, K. Significance of the anatomical relationship between the flexor digitorum longus and sustentaculum tali for reconsideration of the talocalcaneonavicular joint stability mechanism. Sci. Rep. 12, 15218. https://doi.org/10.1038/s41598-022-19543-4 (2022).
Adams, M. A. Funcional anatomy of the musculoskeltal system. In Gray’s Anatomy: The Anatomical Basis of Clinical Practice (ed. Standring, S.) 85–126 (Elsevier Health Sciences, 2021).
Mochizuki, T., Akita, K., Muneta, T. & Sato, T. Pes anserinus: Layered supportive structure on the medial side of the knee. Clin. Anat. 17, 50–54 (2004).
Perry, A. K. et al. Examining the efficacy of medial meniscus posterior root repair: A meta-analysis and systematic review of biomechanical and clinical outcomes. Am. J. Sports Med. 51, 1914–1926 (2023).
Yin, X. Y. et al. The perimensical capsule: Potential supporting structure surrounding meniscus. Cartilage 13, 208S-215S (2021).
Chang, P. S. et al. Mechanical and microstructural properties of meniscus roots vary by location. Am. J. Sports Med. 50, 2733–2739 (2022).
Peltier, A. et al. The role of the meniscotibial ligament in posteromedial rotational knee stability. Knee Surg. Sports Traumatol. Arthrosc. 23, 2967–2973 (2015).
Smith, P. A., Humpherys, J. L., Stannard, J. P. & Cook, J. L. Impact of medial meniscotibial ligament disruption compared to peripheral medial meniscal tear on knee biomechanics. J. Knee Surg. 34, 784–792 (2021).
Krych, A. J. et al. Investigating the chronology of meniscus root tears: Do medial meniscus posterior root tears cause extrusion or the other way around?. Orthop. J. Sports Med. 8, 2325967120961368. https://doi.org/10.1177/2325967120961368 (2020).
Plank, J. & Rychlo, A. Eine Schnellentkalkungsmethode A method for quick decalcification. Zentralbl Allg. Pathol. 89, 252–254 (1952).
Cicchetti, D. V. Guidelines, criteria, and rules of thumb for evaluating normed and standardized assessment instruments in psychology. Psychol. Assess. 6, 284–290 (1994).
Acknowledgements
This study was supported by JSPS KAKENHI (Grant Number JP 22K17645) and Morinomiya University President’s Research Encouragement Award (Grant Number 2022MPA1). The micro-CT analysis was performed in part at the Research Core of Tokyo Medical and Dental University (TMDU). The authors thank Editage (www.editage.com) for English language editing. In addition, the authors acknowledge and thank the anonymous individuals who generously donated their bodies for this study.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study’s conception and design. M.T. and S.T. prepared the materials and performed the data collection and analysis. M.T. wrote the first draft of the manuscript, and all authors commented on the previous versions of the manuscript. All authors have read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Tsutsumi, M., Nimura, A., Tharnmanularp, S. et al. Posteromedial capsular anatomy of the tibia for consideration of the medial meniscal support structure using a multidimensional analysis. Sci Rep 13, 12030 (2023). https://doi.org/10.1038/s41598-023-38994-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-023-38994-x
This article is cited by
-
Revealing the complexity of meniscus microvasculature through 3D visualization and analysis
Scientific Reports (2024)
-
Meniscectomy is associated with a higher rate of osteoarthritis compared to meniscal repair following acute tears: a meta‐analysis
Knee Surgery, Sports Traumatology, Arthroscopy (2023)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.