Abstract
The aim of this study was to evaluate the association between obstructive sleep apnea and morning headache and to assess the improvement of morning headache following positive airway pressure therapy. One hundred and sixteen participants were enrolled in this study; all of them received positive airway pressure therapy for at least 3 months. We checked the differences in various sleep apnea-related parameters according to the presence of morning headache and evaluated the improvement of morning headache following positive airway pressure therapy. Among the 116 study participants, 103 were men, with a mean age and body mass index of 50.34 ± 10.23 years and 28.00 ± 4.21 kg/m2, respectively. The severity of morning headache was higher in the severe obstructive sleep apnea group than in the mild to moderate group (2.16 ± 1.70 vs. 1.50 ± 1.57, P = 0.027). However, the various polysomnographic parameters did not significantly differ according to the presence of headache. The Epworth sleepiness scale score was significantly higher in the morning headache presence group than in the absence group (10.90 ± 5.45 vs. 8.13 ± 4.27, P = 0.003). Furthermore, a notable correlation was observed between the reduction in daytime sleepiness and the improvement in morning headache following PAP treatment (r = 0.503, P < 0.001). Morning headache significantly improved following positive airway pressure therapy (prevalence: 53.4–16.4%; severity: 1.92 ± 1.67 vs. 0.86 ± 0.80, all P < 0.001), especially in the patients with morning headache before positive airway pressure therapy. Morning headache is significantly associated with daytime sleepiness and positive airway pressure therapy improves morning headache.
Similar content being viewed by others
Introduction
Obstructive sleep apnea (OSA) is a common disorder, with a prevalence of 22% (9–37%) in men and 17% (4–50%) in women1. It is characterized by repetitive upper airway obstruction during sleep, hypoxia, and hypercapnia. These events activate the sympathetic nervous system and eventually lead to various diseases, including cardiovascular, metabolic, neurologic, and psychological problems2,3,4,5,6. Thus, appropriate treatment is essential for the prevention of various morbidities associated with OSA. Positive airway pressure (PAP) therapy is the standard first-line treatment for OSA, especially in patients with moderate to severe OSA7,8; it improves patients’ quality of life, excessive daytime sleepiness (EDS), and various morbidities9,10,11.
In our experience, many patients with OSA complain of morning headache in outpatient clinics, and several clinical studies have reported the prevalence of morning headache in patients with OSA from 15.2 to 74%12,13. When we consider the prevalence of morning headache in the general population (5–7%)13, it can be suggested that OSA and morning headache are significantly associated. Furthermore, a number of patients with OSA accompanied by morning headache reported improvements of headache after PAP therapy. However, the causal relationship between various sleep apnea-related parameters and morning headache is controversial14,15,16,17. In addition, the relief of morning headache after PAP therapy is also debatable12,18.
The aim of this study was to evaluate the association between various sleep apnea-related parameters and morning headache and to assess morning headache improvement before and 3 months after PAP therapy.
Results
Among the 116 study participants, 103 were men, with a mean age and body mass index of 50.34 ± 10.23 years and 28.00 ± 4.21 kg/m2, respectively. The prevalence of morning headache in our study subjects was 53.4% (62/116) before PAP therapy. In the comparison of the severity and prevalence of morning headache according to OSA severity, we found that the severity of morning headache was significantly higher in the severe OSA group than in the mild to moderate OSA group. Furthermore, the prevalence of morning headache was also higher in the severe OSA group than in the mild to moderate OSA group; however, this difference was not significant (Table 1).
We compared the various parameters of polysomnography (PSG) and demographics according to the presence of morning headache and did not find any differences between the two groups. However, the ESS score was significantly higher in the morning headache group (Table 2). In the evaluation of changes in morning headache after PAP therapy, we found that the prevalence of morning headache significantly decreased after PAP therapy from 53.4 to 16.4%. Moreover, the severity of morning headache significantly decreased with PAP therapy. When we evaluated in the group with morning headache before PAP therapy, the severity of morning headache significantly decreased following PAP therapy (3.15 ± 1.34 to 1.13 ± 0.86, P < 0.001), and improvement of morning headache was observed in both the mild to moderate and severe OSA groups. Particularly, among the patients with severe sleep apnea with morning headache initially, the severity of morning headache improved by 72% after PAP therapy (3.20 ± 1.41 to 0.95 ± 0.71, P < 0.001). Therefore, we suggest that the improvement of morning headache was significantly greater when only those with headache were analyzed (Table 3). Furthermore, although there was no statistical significance in the improvement of headaches according to PAP compliance, it was observed that the good compliance group (n = 92) showed a greater improvement in headaches (0.83 ± 1.55 vs 1.12 ± 1.66, P = 0.447) compared to the poor compliance group (n = 24). Additionally, when analyzing whether there was a significant correlation between the improvement in daytime sleepiness measured by Epworth sleepiness scale (ESS) and the improvement in morning headache after PAP treatment, it was found that there was a statistically significant correlation (Fig. 1).
Discussion
In our study participants with OSA, the prevalence of morning headache was reported as 53.4%, and various demographics and polysomnographic parameters did not significantly differ according to the presence of morning headache. To date, several studies have reported an association between morning headache and sleep apnea-related parameters. In a previous large population-based study, Kristiansen et al. reported that the average and lowest oxygen saturation levels during sleep were not significantly different according to the presence of morning headache, and Sand et al. also reported that there was no relationship between headache and oxygen desaturation17,19. Moreover, Lovati et al. reported that better respiratory parameters (higher mean oxygen saturation and lower time with an oxygen saturation lower than 90%) were found among headache sufferers with respect to those without headache20. When we consider the results of these studies, hypoxia and respiratory events were not sufficient factors for explaining the mechanism of morning headache. Therefore, we should perform further evaluation to reveal the pathophysiologic mechanism, including the factors related to elevated intracranial pressure21. We consider that basic research is needed to suggest the candidate factors associated with causal relationships.
In this study, we found that daytime sleepiness was significantly associated with morning headache. The ESS is a questionnaire used for the assessment of daytime sleepiness (0–24 points), and the sum of each scale number from 10 to 24 reflects EDS22,23,24. In our analysis, the mean ESS score was 10.90 ± 5.45 in the morning headache presence group and 8.13 ± 4.27 in the morning headache absence group. Recently, Kristoffersen et al. reported that increased EDS was associated with a higher headache frequency25. In addition, Kim et al. also reported that the prevalence of EDS was higher among subjects with chronic tension-type headache (TTH), and those with TTH with EDS had a higher frequency and intensity of headache than those without EDS26. They also reported that EDS is a disabling condition caused by poor nocturnal sleep, which can lead to daytime dysfunction, and is significantly associated with TTH exacerbation26. Thus, we considered that patients with morning headache also experience EDS, and treatment for EDS may be helpful in improving morning headache. According to the recommendations of the Standards of Practice Committee and the Board of Directors of the AASM, continuous PAP is indicated for improving self-reported sleepiness in patients with OSA, and the recommendation grade was suggested as the standard27. According to the definition of the recommendations, the term “standard” reflects a high degree of clinical certainty and generally implies the use of level I evidence27. Therefore, we considered that PAP therapy might also improve morning headache and then assessed changes in morning headache after PAP therapy.
To our knowledge, this study is the largest study (n = 116) that compared morning headache after PAP therapy among patients with OSA. Herein, we found that the prevalence and severity of morning headache significantly improved with PAP therapy. Several studies have reported the improvement of headache after PAP therapy in patients with OSA. Goksan et al. reported that among 76 patients treated with PAP therapy, morning headache was totally resolved in 70 patients after 1 month of treatment12. Furthermore, Johnson et al. also performed a retrospective study in 52 patients with OSA and concluded that treating OSA with PAP therapy improves headache in some patients18. We also found another study that concluded that PAP therapy alone did not improve headache. However, the authors also mentioned that their study sample size was fairly small (n = 21); thus, further investigation is needed28.
This study has several limitations. First, owing to the retrospective nature of this study, we could only find an association between EDS and morning headache. We could not determine the causal relationship between EDS and morning headache and could not suggest the pathophysiologic mechanism underlying morning headache. Thus, additional basic studies including cytokine or genetic analyses of study subjects are needed to provide more valuable data on this topic. Second, we evaluated morning headache among subjects with OSA but found that morning headache was not always associated with OSA. Furthermore, according to the International Classification of Headache Disorders third edition, sleep apnea-related headache was classified separately from morning headache29. Because of the retrospective design of this study, we do not have sufficient data on the characteristics of headache for the diagnosis of sleep apnea-related headache. We consider that if the assessment was performed using the sleep apnea-related headache criteria, we might have found associations with various PSG parameters. Therefore, we will conduct an additional prospective study on various PSG parameters and sleep apnea-related headache. Third, due to the majority of participants being male in this study, statistical analysis based on gender differences could not be performed. However, previous studies have reported that the incidence of morning headache is about twice as high in women compared to men19. Therefore, it is important to always consider gender differences when interpreting the results of this study.
Conclusions
Morning headache is a common symptom in patients with OSA. Herein, the severity was higher in the severe OSA group than in the mild to moderate OSA group. Although we could not find an association between morning headache and various PSG parameters, subjective daytime sleepiness was significantly associated with morning headache. We found that short-term PAP therapy can improve morning headache in adult patients with OSA. Moreover, it can improve the severity of morning headache by 72% in patients with severe OSA. Therefore, when patients with OSA complain of morning headache, PAP therapy may be used as a fundamental treatment modality, which can reduce the need for medication.
Methods
Participants
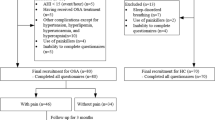
We retrospectively reviewed the medical records of 116 patients with OSA who received PAP therapy consecutively for at least 3 months from December 2017 to June 2020. All of the study subjects underwent endoscopic and computed tomographic examination of the upper airway and full-night PSG for the evaluation and diagnosis of OSA. In addition, all participants completed symptom questionnaires, including the ESS, for the assessment of daytime sleepiness at the initial visit and before and 3 months after PAP therapy. The patients with neurological disorders or those regularly taking analgesics were excluded during the initial data collection phase. In our institutes’ clinical setting, when the patients were diagnosed with OSA based on the PSG findings and the physician decided the treatment modality as PAP therapy, PAP titration was conducted manually by well-trained sleep technicians at the sleep study center of our tertiary hospital and reviewed by certified sleep physicians. The physician prescribed the auto PAP device (DreamStation AutoCPAP, Philips Respironics, Murrysville, PA, USA) according to the optimal pressure range (optimal pressure ± 2 cmH2O). The patients visited our outpatient clinic at 2 weeks, 5 weeks, and 3 months after PAP initiation, and the PAP device was repeatedly set up for appropriate treatment. The compliance to PAP therapy was also assessed at 3 months after PAP therapy initiation; good compliance was defined as using a PAP device for ≥ 4 h daily and ≥ 70% of nights30. This study was approved by the Institutional Ethics Committee of Korea University Ansan Hospital and informed consent is waived due to the nature of the study, according to the approval of the Institutional Review Board (2020AS0258). All research was performed in accordance with the Declaration of Helsinki.
Polysomnographic evaluation
Full-night PSG was performed using an Alice 6 device (Respironics, Murrysville, PA, USA) in our tertiary hospital using the standard American Academy of Sleep Medicine (AASM)-recommended neurophysiologic and respiratory signals, electroencephalography, electromyography, electrooculography, and electrocardiography. Oro-nasal airflow was detected using a thermistor for apnea detection and a pressure transducer for hypopnea detection. Chest and abdominal wall movements were also measured using plethysmography, and oxygen saturation was measured using pulse oximetry. Polysomnographic data were manually scored by a well-trained sleep technician and reviewed by certified clinical physicians according to the recommended AASM criteria31.
Apnea and hypopnea were defined as > 90% reduction of airflow and ≥ 30% reduction of airflow with a decrease in SpO2 of ≥ 4% or arousal for at least 10 s, respectively. We described OSA as an apnea–hypopnea index (AHI) of ≥ 5 and classified it by severity into mild to moderate (AHI: 5–30) and severe (AHI: ≥ 30) OSA groups.
Assessment of headache
All participants completed a questionnaire on the severity of morning headache over the past four weeks using a 7-point Likert scale (0–6 points) before and 3 months after PAP initiation. For the assessment of the prevalence of morning headache as a categorical variable, the subjects who checked points 0 and 1 were considered to have no morning headache.
Statistical analysis
Statistical analysis was performed using the Statistical Package for the Social Sciences version 21 (IBM Corporation, Armonk, NY, USA). An independent t-test or the Mann–Whitney U test was performed on the basis of the data distribution to compare the demographics of the patients and to evaluate the association between the presence of headache and various PSG parameters. The chi-square test or Fisher’s exact test was performed to compare the prevalence of morning headache according to OSA severity and PAP therapy. Spearman’s correlation coefficient was used to assess the relationship between improvement of headache and improvement of daytime sleepiness according to ESS score.
Ethics approval
This study was approved by the Institutional Ethics Committee of Korea University Ansan Hospital (2020AS0258).
Data availability
The datasets generated and analyzed during the current study are available from the corresponding author on reasonable request.
References
Franklin, K. A. & Lindberg, E. Obstructive sleep apnea is a common disorder in the population—A review on the epidemiology of sleep apnea. J. Thorac. Dis. 7, 1311–1322 (2015).
Seo, M. Y. et al. Association of obstructive sleep apnea with subclinical cardiovascular disease predicted by coronary artery calcium score in asymptomatic subjects. Am. J. Cardiol. 120, 577–581 (2017).
Shahar, E. et al. Sleep-disordered breathing and cardiovascular disease: Cross-sectional results of the Sleep Heart Health Study. Am. J. Respir. Crit. Care Med. 163, 19–25 (2001).
Stucki, A. et al. Content comparison of health-related quality of life instruments for obstructive sleep apnea. Sleep Med. 9, 199–206 (2008).
Wenner, J. B., Cheema, R. & Ayas, N. T. Clinical manifestations and consequences of obstructive sleep apnea. J. Cardiopulm. Rehabil. Prev. 29, 76–83 (2009).
Yaggi, H. K. et al. Obstructive sleep apnea as a risk factor for stroke and death. N. Engl. J. Med. 353, 2034–2041 (2005).
Rotenberg, B. W., Murariu, D. & Pang, K. P. Trends in CPAP adherence over twenty years of data collection: A flattened curve. J. Otolaryngol. Head Neck Surg. 45, 43 (2016).
Sullivan, C. E., Issa, F. G., Berthon-Jones, M. & Eves, L. Reversal of obstructive sleep apnoea by continuous positive airway pressure applied through the nares. Lancet 1, 862–865 (1981).
Doherty, L. S., Kiely, J. L., Swan, V. & McNicholas, W. T. Long-term effects of nasal continuous positive airway pressure therapy on cardiovascular outcomes in sleep apnea syndrome. Chest 127, 2076–2084 (2005).
Engleman, H. M., Martin, S. E., Deary, I. J. & Douglas, N. J. Effect of continuous positive airway pressure treatment on daytime function in sleep apnoea/hypopnoea syndrome. Lancet 343, 572–575 (1994).
Marin, J. M., Carrizo, S. J., Vicente, E. & Agusti, A. G. Long-term cardiovascular outcomes in men with obstructive sleep apnoea–hypopnoea with or without treatment with continuous positive airway pressure: An observational study. Lancet 365, 1046–1053 (2005).
Goksan, B. et al. Morning headache in sleep apnoea: Clinical and polysomnographic evaluation and response to nasal continuous positive airway pressure. Cephalalgia 29, 635–641 (2009).
Ohayon, M. M. Prevalence and risk factors of morning headaches in the general population. Arch. Intern. Med. 164, 97–102 (2004).
Goder, R. et al. Morning headaches in patients with sleep disorders: A systematic polysomnographic study. Sleep Med. 4, 385–391 (2003).
Greenough, G. P., Nowell, P. D. & Sateia, M. J. Headache complaints in relation to nocturnal oxygen saturation among patients with sleep apnea syndrome. Sleep Med. 3, 361–364 (2002).
Russell, M. B., Kristiansen, H. A. & Kvaerner, K. J. Headache in sleep apnea syndrome: Epidemiology and pathophysiology. Cephalalgia 34, 752–755 (2014).
Sand, T., Hagen, K. & Schrader, H. Sleep apnoea and chronic headache. Cephalalgia 23, 90–95 (2003).
Johnson, K. G., Ziemba, A. M. & Garb, J. L. Improvement in headaches with continuous positive airway pressure for obstructive sleep apnea: A retrospective analysis. Headache 53, 333–343 (2013).
Kristiansen, H. A. et al. Sleep apnoea headache in the general population. Cephalalgia 32, 451–458 (2012).
Lovati, C. et al. Possible relationships between headache-allodynia and nocturnal sleep breathing. Neurol. Sci. 32(Suppl 1), S145-148 (2011).
Alberti, A. Headache and sleep. Sleep Med. Rev. 10, 431–437 (2006).
Johns, M. W. A new method for measuring daytime sleepiness: The Epworth sleepiness scale. Sleep 14, 540–545 (1991).
Johns, M. W. Reliability and factor analysis of the Epworth sleepiness scale. Sleep 15, 376–381 (1992).
Johns, M. W. Daytime sleepiness, snoring, and obstructive sleep apnea. The Epworth sleepiness scale. Chest 103, 30–36 (1993).
Kristoffersen, E. S., Stavem, K., Lundqvist, C. & Russell, M. B. Excessive daytime sleepiness in chronic migraine and chronic tension-type headache from the general population. Cephalalgia 38, 993–997 (2018).
Kim, K. M. et al. Excessive daytime sleepiness in tension-type headache: A population study. Front. Neurol. 10, 1282 (2019).
Kushida, C. A. et al. Practice parameters for the use of continuous and bilevel positive airway pressure devices to treat adult patients with sleep-related breathing disorders. Sleep 29, 375–380 (2006).
Mitsikostas, D. D., Vikelis, M. & Viskos, A. Refractory chronic headache associated with obstructive sleep apnoea syndrome. Cephalalgia 28, 139–143 (2008).
Arnold, M. Headache Classification Committee of the International Headache Society (IHS) The international classification of headache disorders. Cephalalgia 38, 1–211 (2018).
Seo, M. Y. & Lee, S. H. Compliance with continuous positive airway pressure in patients with obstructive sleep apnea. Sleep Med. Res. 11, 7–14 (2020).
Iber, C., Ancoli-Israel, S., Chesson, A. L. Jr., Quan, S. F., American Academy of Sleep Medicine. The AASM Manual for the Scoring of Sleep and Associated Events (American Academy of Sleep Medicine, 2007).
Acknowledgements
This study was supported by National Research Foundation of Korea (NRF) grant funded by Korean government (Ministry of Education) (NRF-2020R1I1A1A01063604). The funder has no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript. We would like to thank Editage (www.editage.co.kr) for English language editing.
Author information
Authors and Affiliations
Contributions
Conceptualization: S.H.L. Data curation: M.Y.S., M.K.L., M.S.H., J.Y. Funding acquisition: M.Y.S. Methodology: S.H.L. Writing – original draft: M.Y.S. Writing – review and editing: S.H.L., M.Y.S.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Seo, M.Y., Lee, M.K., Han, M.S. et al. Improvement of morning headache in adults with obstructive sleep apnea after positive airway pressure therapy. Sci Rep 13, 14620 (2023). https://doi.org/10.1038/s41598-023-34896-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-023-34896-0
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.