Abstract
Tacrolimus is the mainstay of immunosuppression in liver transplantation to prevent rejection. However, the clinical use of tacrolimus is complicated by its narrow therapeutic window and significant intra-patient variability (IPV). High tacrolimus IPV is associated with overexposure and adverse effects, including malignancy. The effects of tacrolimus IPV in liver transplant recipients with and without hepatocellular carcinoma (HCC) are unknown. We investigated the association between tacrolimus IPV and transplant outcomes in 636 liver transplant patients. Tacrolimus IPV was determined by calculating the coefficient of variance (CV) of outpatient tacrolimus trough levels from 3 to 12 months after transplantation. High tacrolimus IPV was defined as CV > 30%. Patients were grouped according to tacrolimus IPV and HCC status. Among 636 liver transplant patients, 349 had HCC and 287 had no HCC. Overall survival in HCC patients was significantly reduced with high tacrolimus IPV (P < 0.001), whereas survival of non-HCC patients was not associated with tacrolimus IPV. Multivariable analysis confirmed the independent association between high tacrolimus IPV and overall mortality in HCC patients (HR, 3.010; 95% CI, 1.084–4.918). HCC recurred in 59 patients (16.9%) post-transplantation. After adjusting for donor/recipient factors, immunosuppression, and tumor characteristics, high tacrolimus IPV was independently associated with an increased risk of HCC recurrence (HR, 2.196; 95% CI, 1.272–3.791). High tacrolimus IPV was associated with significantly increased risks of overall mortality and HCC recurrence in liver transplant recipients with HCC.
Similar content being viewed by others
Introduction
Hepatocellular carcinoma (HCC) is the third most common cause of cancer-related mortality in the world and has become the major indication for liver transplantation (LT)1,2,3. Refinements in selection criteria, surgical techniques, and immunosuppressive therapies have dramatically improved short-term outcomes4,5,6,7. However, long-term outcomes remain suboptimal, primarily because of the adverse effects of immunosuppression, including HCC recurrence8. Although accumulating evidence has revealed the relationship between overexposure to immunosuppressive agents and an increased risk of HCC recurrence, optimal immunosuppressive regimens have not been clearly defined9,10,11,12.
Tacrolimus is a highly effective immunosuppressant and the current standard of care following LT2,13. Because of its narrow therapeutic window and pharmacokinetic variability, tacrolimus requires therapeutic drug monitoring (TDM)14. Although trough concentrations are used in most transplant centers for tacrolimus TDM, trough concentrations measured at a single time point have limited performance because of high intra-patient variability (IPV). Patients with high tacrolimus IPV may be at risk of underexposure and graft rejection or overexposure and adverse effects, including malignancy and infection15. Therefore, tacrolimus IPV has become recognized as a novel marker to identify solid organ transplant recipients at risk for poor outcomes15,16,17,18,19,20.
Despite increasing awareness of the negative influence of high tacrolimus IPV, the effects of high tacrolimus IPV in LT patients with and without HCC have not been investigated. Therefore, we conducted this study to examine the association between tacrolimus IPV and LT outcomes according to HCC status in a large cohort of liver transplant recipients.
Results
Baseline characteristics
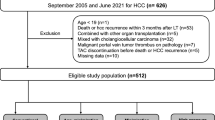
A total of 636 patients who underwent LT with tacrolimus-based immunosuppression were included in this study: 349 with HCC and 287 without HCC. Baseline patient characteristics are summarized in Table 1. Compared to non-HCC recipients, HCC recipients were significantly older, were more likely to be male, were less likely to receive a liver from a deceased donor, and had a significantly lower laboratory Model for End-stage Liver Disease sodium (MELD Na) score. Hepatitis B virus (HBV) was the most common cause of the liver disease (61.3%) in the entire cohort, and the proportion of HBV was significantly higher in the HCC group than in the non-HCC group (79.1% vs. 39.7%, P < 0.001). The median follow-up duration was 62 months (interquartile range, 38.0–95.5 months).
Tacrolimus trough levels and intra-patient variability
A total of 6948 blood samples were analyzed for tacrolimus trough concentrations. The mean number of trough concentration measurements per patient between 3 and 12 months after LT was 11.0 ± 3.1 for HCC patients, and 10.7 ± 2.7 for non-HCC patients (P = 0.253). The mean tacrolimus level was 6.8 ± 1.9 ng/mL for the entire cohort, 6.7 ± 1.9 ng/mL for patients with HCC, and 6.8 ± 1.8 ng/mL for those without HCC (P = 0.370). The mean tacrolimus IPV was 26.7 ± 12.2% for the entire cohort, 26.8 ± 12.4% for the HCC group, and 26.5 ± 12.0% for the non-HCC group. The proportion of patients with high tacrolimus IPV was not significantly different between groups (29.9% vs. 31.0% for the HCC vs. non-HCC groups, respectively; P = 0.770).
To explore potential risk factors associated with high tacrolimus IPV, we performed a multivariable logistic regression analysis (Table 2). Low mean tacrolimus concentration between 3 and 12 months, serum albumin, and hematocrit at 3 months post-transplantation were significantly associated with high tacrolimus IPV.
Tacrolimus intra-patient variability and overall survival
During the follow-up period, 101 patients (15.9%) died: 67 in the HCC group and 34 in the non-HCC group. The 1-year, 2-year, and 5-year overall survival rates were 97.4%, 92.0%, and 82.3% for the HCC group and 99.3%, 96.5%, and 90.1% for the non-HCC group (P = 0.020). In the HCC group, recurrent HCC (n = 38, 56.7%) and infection (n = 19, 28.4%) were the major causes of death. In the non-HCC group, the major causes of death were liver failure (n = 11, 32.4%), other malignancy (n = 8, 23.5%), and infection (n = 6, 17.6%).
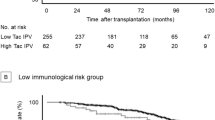
The association between high tacrolimus IPV and patient survival was evident in the HCC group. Overall patient survival in the HCC group was significantly reduced in patients with high tacrolimus IPV (P < 0.001; Fig. 1A). Multivariable Cox regression analysis confirmed that high tacrolimus IPV was independently associated with higher overall mortality in the HCC group (Table 3; hazard ratio [HR], 3.010; 95% CI, 1.842–4.918; P < 0.001). Higher tacrolimus IPV was also associated with an increased risk of overall mortality when assessed as a continuous variable (HR, 1.049; 95% CI, 1.031–1.067; P < 0.001). By contrast, the overall survival of non-HCC patients was not significantly different according to tacrolimus IPV status (P = 0.274; Fig. 1B). In the non-HCC group, recipient age ≥ 60 years and donor age were significantly associated with an increased risk of overall patient mortality, whereas HBV-related liver disease was significantly associated with a lower risk of overall mortality.
Tacrolimus intra-patient variability and biopsy proven allograft rejection
A total of 69 biopsy proven allograft rejection (BPAR) episodes occurred in 52 patients (17 [8.7%] in high tacrolimus IPV group and 35 [7.9%] in low tacrolimus IPV group). The cumulative incidence of BPAR was comparable between high and low tacrolimus IPV group (P = 0.641). The mean tacrolimus IPV was 26.9 ± 12.0% for patients with BPAR, and 26.7 ± 12.3% for those without BPAR (P = 0.930). The mean tacrolimus level was not significantly different (BPAR 6.8 ± 1.9 ng/mL vs. no BPAR 6.9 ± 1.5 ng/mL; P = 0.605).
Tacrolimus intra-patient variability and hepatocellular carcinoma recurrence
We also analyzed the association between tacrolimus IPV and HCC recurrence after LT. As shown in Table 4, there were no significant differences in donor or recipient characteristics between the low and high tacrolimus IPV groups in patients who underwent LT for HCC. The mean tacrolimus trough level of the high tacrolimus IPV group was significantly lower than the low tacrolimus IPV group (6.1 ± 2.1 ng/mL vs. 6.9 ± 1.8 ng/mL, P < 0.001). Compared to low tacrolimus IPV group, high tacrolimus IPV group recipients were more likely to receive mammalian target of rapamycin (mTOR) inhibitor. Mean trough level of mTOR inhibitor was significantly higher in high tacrolimus IPV group than in low tacrolimus IPV group. Tumor characteristics, including pre-transplant alpha-fetoprotein (AFP), viable tumor number, microvascular invasion, differentiation, and maximum tumor size were comparable between the two groups.
HCC recurred in 59 (16.9%) patients after LT. Recurrence-free survival rates at 1, 2, and 5 years were 93.8%, 90.1%, and 86.6% for the low tacrolimus IPV group and 84.7%, 76.9%, and 74.5% for the high tacrolimus IPV group (P = 0.001; Fig. 2). On univariable analysis, high tacrolimus IPV was significantly associated with an increased risk of HCC recurrence. After adjusting for donor and recipient factors, immunosuppression, and tumor characteristics, high tacrolimus IPV was independently associated with an increased risk of HCC recurrence on multivariable analysis (HR, 2.196; 95% CI, 1.272–3.791; P = 0.005; Table 5). Higher tacrolimus IPV was also associated with an increased risk of HCC recurrence when assessed as a continuous variable (HR, 1.019; 95% CI, 1.002–1.037; P = 0.035). High pre-transplant AFP level (HR, 2.537; 95% CI, 1.372–4.692; P = 0.003), microvascular invasion (HR, 2.671; 95% CI, 1.459–4.890; P = 0.001), viable tumor number (HR, 1.058; 95% CI, 1.019–1.099; P = 0.003), and maximum tumor size (HR, 1.196; 95% CI, 1.046–1.366; P = 0.009) were independent risk factors for HCC recurrence, whereas recipient age ≥ 60 years was associated with a decreased risk of HCC recurrence.
Discussion
The rate of recurrent HCC after LT is as high as 15–20% despite careful candidate selection21. Although immunosuppression plays an important role in HCC recurrence, optimal immunosuppressive strategies have not been clearly defined9,10,11,12. In the present study, the effects of tacrolimus IPV on patient survival differed significantly between patients with and without HCC. In patients with HCC, high tacrolimus IPV was significantly associated with an increased risk of overall mortality and HCC recurrence. In contrast, tacrolimus IPV was not associated with overall survival in patients without HCC.
Tacrolimus is the mainstay of immunosuppression in solid organ transplantation to prevent rejection and graft loss2. However, the clinical use of tacrolimus is complicated by its narrow therapeutic window and significant IPV22. Since Borra et al. first described the negative effects of high tacrolimus IPV on graft outcomes after kidney transplantation23, there has been a growing body of literature supporting the association between high tacrolimus IPV and deleterious graft outcomes following non-kidney solid organ transplantation14,19,20.
In the LT setting, several studies have suggested a potential association between high tacrolimus IPV and increased risk of rejection, de novo donor-specific antibodies, or graft failure17,18. By contrast, van der Veer MAA et al. failed to find an association between tacrolimus IPV and immune-mediated graft injury24. However, previous studies used infrequent trough concentration measurements during the early postoperative period. In addition, high heterogeneity of disease severity, comorbidities, and HCC status of patients undergoing LT make it especially challenging to draw conclusions regarding the effects of tacrolimus IPV after LT15. To our knowledge, this is the first study to assess the effects of tacrolimus IPV on outcomes in LT recipients with and without HCC.
In this study, overall patient survival in the HCC group was significantly reduced in patients with high tacrolimus IPV. High tacrolimus IPV was also significantly associated with an increased risk of HCC recurrence. Importantly, the effects of high tacrolimus IPV on HCC recurrence remained significant in the fully adjusted model accounting for differences in tumor number, tumor size, microvascular invasion, AFP level, and mean tacrolimus trough concentration. By contrast, tacrolimus IPV was not associated with patient survival in individuals without HCC. In addition, high tacrolimus IPV was not associated with BPAR. Overall low alloimmune reactivity of liver grafts may attenuate potential adverse effects of high tacrolimus IPV, such as graft rejection and immune-mediated graft injury24,25.
As the immune system plays a critical role in preventing cancer development and progression26, use of immunosuppression may increase the risk of cancer after LT, including recurrent HCC11,27. In vitro and in vivo studies have demonstrated that tacrolimus enhances proto-oncogenes and cancer pathways in a dose-dependent manner28,29,30. Clinical studies have also demonstrated a dose-dependent relationship between tacrolimus and HCC recurrence9,10. However, optimal tacrolimus trough concentrations in LT recipients with and without HCC have not been extensively evaluated11. In addition, none of these studies analyzed tacrolimus IPV.
The causes of tacrolimus IPV are multifactorial and include medication non-adherence, drug-drug interactions, food intake, and gastrointestinal disorders14,15,31. Although medication non-adherence is a major determinant of high IPV, some degree of IPV exists regardless of adherence22. In this study, we observed a significant association between albumin concentration, hematocrit, and high tacrolimus IPV. This may be attributed to the documented effects of albumin concentration and hematocrit on tacrolimus distribution32. Regardless of the cause, high tacrolimus IPV is an important risk factor for poor outcomes in patients with HCC. Previous studies have shown that adherence-enhancing interventions can improve tacrolimus IPV33. Taken together, our findings suggest that HCC patients with high tacrolimus IPV require close surveillance for recurrence of HCC.
This study has several limitations worth considering. First, it is a single-center retrospective study, with the usual drawbacks of a retrospective study, as well as potentially limited generalizability. However, the single-center design has the advantage of homogeneity of immunosuppressive regimens and follow-up protocols. Second, as with any observational study, we can neither prove causality nor exclude the possibility of potential confounders. Third, information about tacrolimus adherence is lacking. Objective data regarding adherence are difficult to obtain in routine clinical practice. Nevertheless, we evaluated other potential risk factors for high tacrolimus IPV.
In conclusion, our study highlights the differential effects of tacrolimus IPV between LT recipients with and without HCC. High tacrolimus IPV significantly increased the risk of overall patient mortality and HCC recurrence after LT. These findings have important implications for managing transplant recipients, as HCC is a major indication for LT worldwide. Using tacrolimus IPV to individualize immunosuppressive treatment and employing stringent surveillance regimens for HCC recurrence may improve long-term outcomes.
Methods
Study population
We screened 772 adults who underwent LT and received tacrolimus-based immunosuppression between January 2009 and December 2018 at the Severance Hospital, Seoul, Republic of Korea. Patients who underwent re-transplantation or who experienced graft loss within 3 months were excluded. We excluded patients with less than five tacrolimus trough concentrations between 3 and 12 months after LT or with combined hepatocellular-cholangiocarcinoma. After excluding ineligible patients, 636 transplant recipients were included in this study. These patients were categorized according to HCC status and tacrolimus IPV (Fig. 3).
HCC selection criteria and loco-regional treatment
We accepted patients with HCC for LT irrespective of tumor number and size, in the absence of extrahepatic metastases. In patients exceeding the Milan criteria (1 lesion ≤ 5 cm or 2–3 lesions ≤ 3 cm), pretransplant loco-regional treatment was used for downstaging. Response evaluation was done at 4–6 weeks after loco-regional treatment. LT was performed if tumor number or size decreased or tumor marker decreased after loco-regional treatment. Loco-regional treatment was also used in those within the Milan criteria for bridging to LT.
Clinical and laboratory measurements
Routine biochemical tests, including tacrolimus trough concentrations, were performed every month during the first year after LT and then every 1 to 2 months thereafter. As surveillance for HCC recurrence, serum AFP levels were measured every 1 to 2 months, and chest radiography and dynamic liver computed tomography were performed every 3 to 6 months. When HCC recurrence was suspected, magnetic resonance imaging, whole-body bone scintigraphy, or positron emission tomography was performed to establish the diagnosis.
We analyzed outpatient tacrolimus trough concentrations between 3 and 12 months. Tacrolimus trough concentrations were measured using a microparticle enzyme immunoassay: Tacrolimus II MEIA/IMx analyzer (Abbott Laboratories, Chicago, IL, USA) until May 8, 2008; Dimension RxL (Siemens, Munich, Germany) between May 9, 2008 and February 25, 2013; Architect i2000 (Abbott Laboratories) from February 26, 2013 to the end of the study. We excluded erroneously high tacrolimus concentrations (> 20 ng/mL) resulting from patients taking their morning dose of tacrolimus before blood sampling. Tacrolimus IPV was estimated by calculating the coefficient of variance (CV) using this equation: CV (%) = (standard deviation/mean tacrolimus trough concentration) × 100.
Immunosuppression
Immunosuppression was performed according to the standard protocol at our institution34. Most patients received induction immunosuppression with basiliximab (20 mg on days 0 and 4 post-transplantation). Maintenance immunosuppression for all patients consisted of tacrolimus, prednisolone, and mycophenolate mofetil (MMF) or mammalian target of rapamycin (mTOR) inhibitor. The initial tacrolimus dosage (0.1 mg/kg) was administered orally. Subsequent doses were adjusted to maintain a target trough concentration between 5 and 8 ng/mL. The initial dose of methylprednisolone (500–1000 mg) was gradually reduced and replaced with oral prednisolone (5–10 mg/day) during the first 3 weeks after transplantation. MMF was initiated at 1.0–1.5 g/day, and the dose was subsequently adjusted to minimize adverse events, such as neutropenia or gastrointestinal side effects. mTOR inhibitor was usually initiated at 4 weeks after transplantation.
Study endpoints and definitions
High tacrolimus IPV was defined as a CV > 30%15,22,31. HCC recurrence was defined according to radiologic evidence. Patient survival was calculated from the date of transplantation to the date of death, loss to follow-up, or December 31, 2020 (end of the follow-up period). The primary study endpoint was overall patient survival. The secondary endpoints were HCC recurrence, recurrence-free survival, and BPAR.
Statistical analysis
Depending on the type of variable, data were expressed as frequency, mean and standard deviation, or median and interquartile range. Continuous variables were compared using Student’s t-test for parametric data or the Mann–Whitney test for nonparametric data. Chi-square or Fisher’s exact tests were used as appropriate to compare categorical variables. Multivariable logistic regression analysis was performed using high tacrolimus IPV (CV > 30%) as the outcome variable. Covariates were defined a priori and included baseline characteristics and laboratory findings at 3 months post-LT. Covariates with P < 0.2 in univariable analyses were entered into the multivariable logistic regression model. Overall patient survival and recurrence-free survival were analyzed using Kaplan–Meier curves and the log-rank test. Cox proportional hazard regression analyses with the backward conditional method were used to evaluate associations between tacrolimus IPV and time-to-event outcomes (overall mortality and HCC recurrence). All tests were performed two-tailed, and P values < 0.05 were considered statistically significant. Statistical analyses were performed using SPSS software (version 25.0; SPSS Inc., Chicago, IL, USA).
Ethics statement
All study procedures were conducted in accordance with the Declaration of Helsinki and were approved by the Institutional Review Board of Severance Hospital (2020-2851-001). All living donations were voluntary, and all donors underwent evaluation by transplant surgeons, hepatologists, and clinical psychologists. All deceased donors were brain dead. No donor organs were obtained from executed prisoners or other institutionalized persons. Informed consent was waived by the Institutional Review Board of Severance Hospital because of the study’s retrospective design.
Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Sung, H. et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J. Clin. 71, 209–249 (2021).
Kwong, A. et al. OPTN/SRTR 2018 annual data report: Liver. Am. J. Transplant. 20(Suppl S1), 193–299 (2020).
Adam, R. et al. 2018 Annual report of the european liver transplant registry (ELTR) - 50-year evolution of liver transplantation. Transpl. Int. 31, 1293–1317 (2018).
Mazzaferro, V. et al. Liver transplantation for the treatment of small hepatocellular carcinomas in patients with cirrhosis. N. Engl. J. Med. 334, 693–699 (1996).
Yao, F. Y. et al. Liver transplantation for hepatocellular carcinoma: Validation of the UCSF-expanded criteria based on preoperative imaging. Am. J. Transplant. 7, 2587–2596 (2007).
Mazzaferro, V. et al. Predicting survival after liver transplantation in patients with hepatocellular carcinoma beyond the Milan criteria: a retrospective, exploratory analysis. Lancet Oncol. 10, 35–43 (2009).
Toso, C. et al. Total tumor volume and alpha-fetoprotein for selection of transplant candidates with hepatocellular carcinoma: A prospective validation. Hepatology 62, 158–165 (2015).
Wallace, D. et al. Assessing the impact of suboptimal donor characteristics on mortality after liver transplantation: A time-dependent analysis comparing HCC with non-HCC patients. Transplantation 103, e89–e98 (2019).
Rodríguez-Perálvarez, M. et al. Reduced exposure to calcineurin inhibitors early after liver transplantation prevents recurrence of hepatocellular carcinoma. J. Hepatol. 59, 1193–1199 (2013).
Vivarelli, M. et al. Liver transplantation for hepatocellular carcinoma under calcineurin inhibitors: reassessment of risk factors for tumor recurrence. Ann. Surg. 248, 857–862 (2008).
Rodríguez-Perálvarez, M., De la Mata, M. & Burroughs, A. K. Liver transplantation: Immunosuppression and oncology. Curr. Opin. Organ Transplant. 19, 253–260 (2014).
Geissler, E. K. et al. Sirolimus use in liver transplant recipients with hepatocellular carcinoma: A randomized, multicenter, open-label phase 3 trial. Transplantation 100, 116–125 (2016).
Haddad, E.M., McAlister, V.C., Renouf, E., Malthaner, R., Kjaer, M.S., Gluud, L.L. Cyclosporin versus tacrolimus for liver transplanted patients. Cochrane Database Syst. Rev. 4, CD005161 (2006).
Brunet, M. et al. Therapeutic drug monitoring of tacrolimus-personalized therapy: Second consensus report. Ther. Drug Monit. 41, 261–307 (2019).
Gonzales, H. M. et al. A comprehensive review of the impact of tacrolimus intrapatient variability on clinical outcomes in kidney transplantation. Am. J. Transplant. 20, 1969–1983 (2020).
Shemesh, E. et al. The medication level variability index (MLVI) predicts poor liver transplant outcomes: A prospective multi-site study. Am. J. Transplant. 17, 2668–2678 (2017).
Rayar, M. et al. High intrapatient variability of tacrolimus exposure in the early period after liver transplantation is associated with poorer outcomes. Transplantation 102, e108–e114 (2018).
Del Bello, A. et al. High tacrolimus intra-patient variability is associated with graft rejection, and de novo donor-specific antibodies occurrence after liver transplantation. World J. Gastroenterol. 24, 1795–1802 (2018).
Ensor, C. R. et al. Increasing tacrolimus time-in-therapeutic range is associated with superior one-year outcomes in lung transplant recipients. Am. J. Transplant. 18, 1527–1533 (2018).
Gueta, I. et al. High tacrolimus trough level variability is associated with rejections after heart transplant. Am. J. Transplant. 18, 2571–2578 (2018).
Bruix, J. & Sherman, M. Management of hepatocellular carcinoma. Hepatology 42, 1208–1236 (2005).
Leino, A. D. et al. Assessment of tacrolimus intrapatient variability in stable adherent transplant recipients: Establishing baseline values. Am. J. Transplant. 19, 1410–1420 (2019).
Borra, L. C. et al. High within-patient variability in the clearance of tacrolimus is a risk factor for poor long-term outcome after kidney transplantation. Nephrol. Dial Transplant. 25, 2757–2763 (2010).
van der Veer, M. A. A. et al. High Intrapatient variability in tacrolimus exposure is not associated with immune-mediated graft injury after liver transplantation. Transplantation 103, 2329–2337 (2019).
Benseler, V. et al. The liver: A special case in transplantation tolerance. Semin. Liver Dis. 27, 194–213 (2007).
Hanahan, D. & Weinberg, R. A. Hallmarks of cancer: The next generation. Cell 144, 646–674 (2011).
Yokoyama, I., Carr, B., Saitsu, H., Iwatsuki, S. & Starzl, T. E. Accelerated growth rates of recurrent hepatocellular carcinoma after liver transplantation. Cancer 68, 2095–2100 (1991).
Maluccio, M. et al. Tacrolimus enhances transforming growth factor-beta1 expression and promotes tumor progression. Transplantation 76, 597–602 (2003).
Khanna, A., Cairns, V. & Hosenpud, J. D. Tacrolimus induces increased expression of transforming growth factor-beta1 in mammalian lymphoid as well as nonlymphoid cells. Transplantation 67, 614–619 (1999).
Ogawa, T. et al. Rho-associated kinase inhibitor reduces tumor recurrence after liver transplantation in a rat hepatoma model. Am. J. Transplant. 7, 347–355 (2007).
Kim, E. J. et al. Clinical significance of tacrolimus intra-patient variability on kidney transplant outcomes according to pre-transplant immunological risk. Sci. Rep. 11, 12114 (2021).
Robles-Piedras, A. L. et al. Relationship among changes in hematocrit, albumin and corticosteroid dose on the disposition of tacrolimus during the first six months following renal transplantation. Proc. West Pharmacol. Soc. 54, 30–32 (2011).
Kuypers, D. R. et al. Improved adherence to tacrolimus once-daily formulation in renal recipients: a randomized controlled trial using electronic monitoring. Transplantation 95, 333–340 (2013).
Kang, I. et al. Impact of everolimus on survival after liver transplantation for hepatocellular carcinoma. Clin. Mol. Hepatol. 27, 589–602 (2021).
Funding
The authors declare no funding was received for this study.
Author information
Authors and Affiliations
Contributions
H.J.K.: data acquisition, statistical analysis, writing, and revision of the manuscript. J.L.: study design, data acquisition, statistical analysis, writing, and revision of the manuscript. D.J.J: study design, interpreted the data, revision of the manuscript. J.G.L. and M.S.K.: data acquisition, interpreted the data.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Kim, H.J., Lee, J., Lee, J.G. et al. Clinical association between tacrolimus intra-patient variability and liver transplantation outcomes in patients with and without hepatocellular carcinoma. Sci Rep 12, 16169 (2022). https://doi.org/10.1038/s41598-022-20636-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-022-20636-3
This article is cited by
-
Radiation therapy with phenotypic medicine: towards N-of-1 personalization
British Journal of Cancer (2024)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.