Abstract
SuperPATH is a novel approach to the hip joint that needs to be compared to other known surgical approaches. To conduct a network meta-analysis (NMA) of randomized controlled trials (RCTs) comparing short-term outcomes of SuperPATH, direct anterior (DAA), and posterior/ posterolateral approaches (PA) in total hip joint arthroplasty (THA). We performed a systematic review on PubMed, CNKI, Embase, The Cochrane Library, Clinical trials, and Google Scholar up to November 30th, 2021. We assessed treatment effects between SuperPATH, DAA, and PA by performing a frequentist NMA, including a total of 20 RCTs involving 1501 patients. SuperPATH showed a longer operation time (MD = 16.99, 95% CI 4.92 to 29.07), a shorter incision length (MD = −4.71, 95% CI −6.21 to −3.22), a lower intraoperative blood loss (MD = −81.75, 95% CI −114.78 to −48.72), a higher HHS 3, 6 and 12 months postoperatively (MD = 2.59, 95% CI 0.59–4.6; MD = 2.14, 95% CI 0.5–3.77; MD = 0.6, 95% CI 0.03–1.17, respectively) than PA. DAA showed a higher intraoperative blood loss than PA and SuperPATH (MD = 91.87, 95% CI 27.99–155.74; MD = 173.62, 95% CI 101.71–245.53, respectively). No other relevant differences were found. In conclusion, the overall findings suggested that the short-term outcomes of THA through SuperPATH were statistically superior to PA. DAA and PA as well as SuperPATH and DAA showed indifferent results.
Similar content being viewed by others
Introduction
Patient outcomes after hip arthroplasty have improved over the past few decades. SuperPATH was introduced by Chow in 2011 as a novel hip approach in an attempt to solve the remaining problems1. Benefits of SuperPATH: Hip surgery in situ with the lower limb resting throughout the whole operation; tissue-sparing dissection through the interval between the gluteus medius and piriformis muscles; joint capsule preservation; unproblematic exposure of the acetabulum through accessory access. Two network meta-analyses (NMAs) comparing SuperPATH, the direct anterior approach (DAA), and conventional approaches showed some advantages of SuperPATH2,3. The strong limitation of those two NMAs was that they summarized all conventional approaches, although these differ significantly in terms of surgical techniques and outcome4,5,6. A different methodological approach is required to overcome this limitation. We performed another NMA of randomized controlled trials (RCTs) with the following PICO (Population, Intervention, Control, and Outcomes) question: In patients with hip disease or fracture, is the short-term outcome after total hip arthroplasty (THA) implanted through SuperPATH better compared to DAA and/or posterior/posterolateral (posterior/posterolateral approach = PA)?
Methods
Details on the SuperPATH technique
The SuperPATH technique is briefly described as follows: the incision of the capsule is performed through a 6–10 cm skin incision and a muscle-sparing approach between the piriformis and gluteus minimus muscles in lateral decubitus position. The femoral canal is then opened with a reamer, the femur is broached and osteotomy of the femoral neck is performed. Following exposure of the acetabulum, the acetabular reamers are inserted through the main incision and attached within the surgical field to the shaft of the motorized drill, which is inserted through a separate percutaneous portal passing adjacent to the posterior aspect of the proximal femur. After implantation of the cup, inlay, modular neck, and head, reposition is performed. Wound closure concludes the operation.
Search strategy and study selection
The PRISMA recommendations were followed when performing and presenting our NMA7. The review protocol was registered in PROSPERO on September 11th, 2021 (CRD42021272994). Our search strategy and methods were similar to our previous works2,3. We searched the following databases and checked citations of screened studies and related meta-analyses for relevant manuscripts up to November 30th, 2021, without restrictions to publication date or language: PubMed, China National Knowledge Infrastructure (CNKI), Embase, The Cochrane Library, Clinical trials. We built a BOOLEAN search strategy for RCTs on SuperPATH and DAA as follows: [(SuperPATH OR supercapsular percutaneously assisted approach in total hip arthroplasty)] and [(THR OR THA OR total hip arthroplasty) AND (approach) AND (anterior OR posterior OR posterolateral)]. We adapted search terms to the syntax of the used databases. Furthermore, we searched Google Scholar for relevant RCTs. Titles, abstracts, and then full-text articles were independently reviewed by two reviewers (NR and PL). The decision on the inclusion of each study was determined by the consensus between the two reviewers. Cases of disagreement were resolved by discussion with a third reviewer (KL). Kappa coefficient was used to measure the agreement between the reviewers. The entire search and selection process was carried out separately for studies on DAA and studies on SuperPATH, using the same methods. A Chinese-speaking reviewer (KL) helped with the search in CNKI.
Inclusion/exclusion criteria
We included RCTs with human participants with hip disease or hip fracture, who had THA through either DAA or SuperPATH compared to PA. We excluded studies for the following reasons: no outcome of interest, employment of a computer navigation system, and hip replacement with hemiarthroplasty.
Types of outcome measures
-
1.
Surgical outcome
-
The operation time (in min.) was defined as the time interval from the skin incision to suture. It correlates with the operating skills and with the risk of infection.
-
The incision length (in cm) was measured on a graduated scale. It is one of several indicators of intraoperative trauma.
-
The intraoperative blood loss (in ml) was defined as the total amount of blood from the suction device. It is an indirect indicator of intraoperative trauma.
-
-
2.
Functional outcome
-
The Harris Hip Score (HHS) was developed for the assessment of the results of hip surgery8. The hip joint function was periodically evaluated at 3, 6, and 12 months postoperatively. The score adds points from the evaluation of four categories: pain, function, degree of deformity, and hip range of motion. The best achievable score is 100 points.
-
-
3.
Radiological outcome
-
The acetabular cup anteversion angle and the inclination angle (in degrees) have ideal values for positioning: anteversion angle from 10° to 25° and inclination angle from 40° to 50°9. A too large anteversion angle often leads to posterior impingement, resulting in anterior dislocation, and a too small anteversion angle leads to posterior dislocation.
-
Data extraction and quality assessment
Two reviewers (NR and PL) extracted the following relevant data into a data extraction form in a standard electronic spreadsheet and the Cochrane software program Review Manager Version 5.3: first author, year of publication, number of patients, patient characteristics, risk of bias and outcome. Cases of disagreement were resolved by discussion with a third reviewer (KL). The assessment of the risk of bias and the level of evidence was carried out independently by two reviewers (NR and KL) according to Cochrane's Risk of Bias 2 (RoB 2) tool10, respectively according to the recommendations of the GRADE system11.
Statistical analysis
Direct comparison: measures of treatment effect
SuperPATH or DAA represented the “experimental group” and PA represented the “control group”. A direct comparison with both fixed and random effects models was applied to calculate the results for either SuperPATH or DAA and PA. We limited the presentation of statistical calculations to random effects model, as this method was more conservative and provided better estimates with wider confidence intervals. Mean differences (MDs) with 95% confidence intervals (CIs) were estimated for all outcomes. A common τ2 was assumed for calculation of the estimates of the random effects, using the DerSimonian and Laird method. Study weighting was performed by inverse variance12. In our NMA, we adhered to the Cochrane Handbook for Systematic Reviews of Interventions13.
Indirect comparison: network meta-analysis
A NMA using frequentist methods14 was performed, borrowing information from the direct comparisons mentioned above and using the PA group as a common comparator and reference node within the network. The following programs were used: meta and netmeta15. In addition, we calculated prediction intervals to estimate where to expect the results of future NMAs. We presented both direct comparison estimates and network estimates in a forest plot per outcome on a common scale. All statistic calculations were performed by a professional statistician (SB).
Assessment of heterogeneity
We assessed heterogeneity with a test on Cochrane’s Q statistic, which followed a distribution with k-degrees of freedom (p-value < 0.10 is indicative of heterogeneity), and with a Higgins’ test I2 (low heterogeneity, < 25%; moderate heterogeneity, 25–75%; and high heterogeneity, > 75%)16. Results were presented regardless of the detection of heterogeneity to maintain the informative value within the forest plots. We did not pool study data that were clinically too diverse.
Results
Study identification and selection
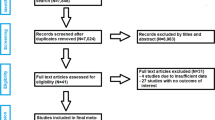
A description of the study selection process is presented in a PRISMA flow diagram (Fig. 1). A total of 1019 studies were identified in our initial literature search on SuperPATH, after removing 501 duplicates. After the first screening procedure by title and abstract (κ = 1.0) with total agreement by the reviewers, 22 RCTs were assessed for eligibility. After the second screening procedure by full-paper analysis (κ = 1.0), 13 RCTs on SuperPATH17,18,19,19,20,21,22,23,24,25,26,27,28 were included in the final NMA. A total of 3074 studies were identified in our initial literature search on DAA, after removing 2251 duplicates. After the first screening procedure by title and abstract (κ = 0.96) with disagreement between the reviewers concerning 1 RCT, 27 RCTs were assessed for eligibility. After the second screening procedure by full-paper analysis (κ = 1.0), 7 RCTs on DAA29,30,31,32,33,34,35 were included in the final NMA.
Characteristics of the RCTs
Thirteen RCTs, published between 2017 and 2021, compared SuperPATH with PA, altogether including 919 patients (with 923 operated hip joints). Of those patients, 459 were operated through SuperPATH and 460 through PA. The sample size of those RCTs ranged from 4 to 116 patients. Four RCTs were published in English language19,20,21,25, five RCTs in Chinese with an English abstract22,23,26,27,28 and four RCTs only in Chinese17,18,19,24. Seven RCTs, published between 2013 and 2020, compared DAA with PA, altogether including 582 patients. Of those patients, 291 were operated through DAA and 291 through PA. The sample size of those RCTs ranged from 46 to 120 patients. All RCTs on DAA were published in English language. Of the 7 RCTs included, 4 RCTs reported having used a traction table in THA through DAA29,30,31,32. The main characteristics of the 20 RCTs on SuperPATH and DAA with an overall 1501 included patients are presented in Table 1.
Risk of bias and level of evidence
The quality of the included RCTs was assessed according to the Cochrane Collaboration’s tool for risk of bias (Table 2) and according to the recommendations of the GRADE system (Table 3).
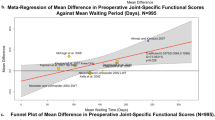
Clinical and statistical heterogeneity
The clinical characteristics for gender, age, and BMI (Table 1) showed no relevant differences between the patients in the experimental (either SuperPATH or DAA) and control group (PA). The statistical heterogeneity of all measured outcomes is shown in Figs. 2, 3, 4, 5, 6, 7, 8, 9.
Outcomes
1. Surgical outcomes
Operation time: SuperPATH vs. PA
In a direct comparison between SuperPATH and PA, data on 711 patients were pooled from 10 RCTs (I2 = 99%, p < 0.01, Fig. 2). The operation time of SuperPATH was 17 min. longer than the operation time of PA (MD = 16.99, 95% CI 4.92 to 29.07).
Operation time: DAA vs. PA
In a direct comparison between DAA and PA, data on 408 patients were pooled from 5 RCTs (I2 = 82%, p < 0.01, Fig. 2). There was no difference in operation time (MD = 15.64, 95% CI −1.02 to 32.29).
Operation time: DAA vs. SuperPATH
In an indirect comparison between DAA and SuperPATH, data on 559 patients were pooled from 15 RCTs (I2 = 98%, p < 0.01, Fig. 2). There was no difference in operation time (MD = −1.36, 95% CI −21.93 to 19.21).
Incision length: SuperPATH vs. PA
In a direct comparison between SuperPATH and PA, data on 805 patients were pooled from 11 RCTs (I2 = 98%, p < 0.01, Fig. 3). The incision length of SuperPATH was 4.7 cm shorter than the incision length of PA (MD = −4.71, 95% CI −6.21 to −3.22).
Incision length: DAA vs. PA
In a direct comparison between DAA and PA, data on 207 patients were pooled from 2 RCTs (I2 = 100%, p < 0.01, Fig. 3). There was no difference in incision length (MD = −1.54, 95% CI −4.98 to 1.91).
Incision length: DAA vs. SuperPATH
In an indirect comparison between DAA and SuperPATH, data on 505 patients were pooled from 13 RCTs (I2 = 99%, p < 0.01, Fig. 3). There was no difference in incision length (MD = 3.18, 95% CI −0.58 to 6.93).
Intraoperative blood loss: SuperPATH vs. PA
In a direct comparison between SuperPATH and PA, data on 689 patients were pooled from 10 RCTs (I2 = 99%, p < 0.01, Fig. 4). The intraoperative blood loss of SuperPATH was 81.8 ml less than the intraoperative blood loss of PA (MD = −81.75, 95% CI −114.78 to −48.72).
Intraoperative blood loss: DAA vs. PA
In a direct comparison between DAA and PA, data on 253 patients were pooled from 3 RCTs (I2 = 89%, p < 0.01, Fig. 4). The intraoperative blood loss of DAA was 91.9 ml higher than the intraoperative blood loss of PA (MD = 91.87, 95% CI 27.99 to 155.74).
Intraoperative blood loss: DAA vs. SuperPATH
In an indirect comparison between DAA and SuperPATH, data on 470 patients were pooled from 13 RCTs (I2 = 99%, p < 0.01, Fig. 4). The intraoperative blood loss of DAA was 173.6 ml higher than the intraoperative blood loss of SuperPATH (MD = 173.62, 95% CI 101.71 to 245.53).
2. Functional outcome: Harris Hip Score
HHS 3 months postoperatively: SuperPATH vs. PA
In a direct comparison between SuperPATH and PA, data on 559 patients were pooled from 9 RCTs (I2 = 95%, p < 0.01, Fig. 5). The HHS 3 months postoperatively of SuperPATH was 2.6 points higher than the HHS 3 months postoperatively of PA (MD = 2.59, 95% CI 0.59 to 4.6).
HHS 3 months postoperatively: DAA vs. PA
In a direct comparison between DAA and PA, data on 362 patients were pooled from 4 RCTs (I2 = 53%, p = 0.09, Fig. 5). There was no difference in HHS 3 months postoperatively (MD = 1.95, 95% CI −1.8 to 5.7).
HHS 3 months postoperatively: DAA vs. SuperPATH
In an indirect comparison between DAA and SuperPATH, data on 459 patients were pooled from 13 RCTs (I2 = 94%, p < 0.01, Fig. 5). There was no difference in HHS 3 months postoperatively of DAA (MD = −0.64, 95% CI −4.89 to 3.61).
HHS 6 months postoperatively: SuperPATH vs. PA
In a direct comparison between SuperPATH and PA, data on 482 patients were pooled from 8 RCTs (I2 = 84%, p < 0.01, Fig. 6). The HHS 6 months postoperatively of SuperPATH was 2.1 points higher than the HHS 6 months postoperatively of PA (MD = 2.14, 95% CI 0.5 to 3.77).
HHS 6 months postoperatively: DAA vs. PA
In a direct comparison between DAA and PA, data on 262 patients were pooled from 3 RCTs (I2 = 0%, p = 0.67, Fig. 6). There was no difference in HHS 6 months postoperatively (MD = 0.66, 95% CI −2.69 to 4.0).
HHS 6 months postoperatively: DAA vs. SuperPATH
In an indirect comparison between DAA and SuperPATH, data on 370 patients were pooled from 11 RCTs (I2 = 80%, p < 0.01, Fig. 6). There was no difference in HHS 6 months postoperatively (MD = −1.48, 95% CI −5.2 to 2.24).
HHS 12 months postoperatively: SuperPATH vs. PA
In a direct comparison between SuperPATH and PA, data on 330 patients were pooled from 6 RCTs (I2 = 0%, p = 0.87, Fig. 7). The HHS 12 months postoperatively of SuperPATH was 0.6 points higher than the HHS 12 months postoperatively of PA (MD = 0.6, 95% CI 0.03 to 1.17).
HHS 12 months postoperatively: DAA vs. PA
In a direct comparison between DAA and PA, data on 243 patients were pooled from 3 RCTs (I2 = 0%, p = 0.46, Fig. 7). There was no difference in HHS 12 months postoperatively of DAA (MD = 1.28, 95% CI −0.28 to 2.84).
HHS 12 months postoperatively: DAA vs. SuperPATH
In an indirect comparison between DAA and SuperPATH, data on 288 patients were pooled from 9 RCTs (I2 = 0%, p = 0.85, Fig. 7). There was no difference in HHS 12 months postoperatively (MD = 0.68, 95% CI −0.98 to 2.35).
3. Radiological outcome
Acetabular cup anteversion angle: SuperPATH vs. PA
In a direct comparison between SuperPATH and PA, data on 160 patients were pooled from 4 RCTs (I2 = 0%, p = 0.75, Fig. 8). There was no difference in acetabular cup anteversion angle (MD = −0.51, 95% CI −3.04 to 2.01).
Acetabular cup anteversion angle: DAA vs. PA
In a direct comparison between DAA and PA, data on 436 patients were pooled from 5 RCTs (I2 = 85%, p < 0.01, Fig. 8). There was no difference in acetabular cup anteversion angle (MD = −1.78, 95% CI −4.09 to 0.53).
Acetabular cup anteversion angle: DAA vs. SuperPATH
In an indirect comparison between DAA and SuperPATH, data on 298 patients were pooled from 9 RCTs (I2 = 75%, p < 0.01, Fig. 8). There was no difference in acetabular cup anteversion angle (MD = −1.27, 95% CI −4.69 to 2.15).
Acetabular cup inclination angle: SuperPATH vs. PA
In a direct comparison between SuperPATH and PA, data on 256 patients were pooled from 5 RCTs (I2 = 26%, p = 0.25, Fig. 9). The acetabular cup inclination angle of SuperPATH was 3.0° lower than the acetabular cup inclination angle of PA (MD = −2.96, 95% CI −5.24 to −0.67).
Acetabular cup inclination angle: DAA vs. PA
In a direct comparison between DAA and PA, data on 536 patients were pooled from 6 RCTs (I2 = 78%, p < 0.01, Fig. 9). There was no difference in acetabular cup inclination angle (MD = 0.14, 95% CI −1.67 to 1.95).
Acetabular cup inclination angle: DAA vs. SuperPATH
In an indirect comparison between DAA and SuperPATH, data on 397 patients were pooled from 11 RCTs (I2 = 68%, p < 0.01, Fig. 9). The acetabular cup inclination angle of SuperPATH was 3.1° lower than the acetabular cup inclination angle of DAA (MD = 3.09, 95% CI 0.18 to 6.01).
Discussion
Main and new findings
Our NMA included 20 RCTs with 1501 patients. Of these, 7 RCTs involving 592 patients compared DAA with PA, and 13 RCTs involving 919 patients compared SuperPATH with PA. Our NMA indicated that the results of THA through SuperPATH were statistically superior to THA through PA regarding the investigated outcomes. SuperPATH showed statistically better results on incision length, intraoperative blood loss, and HHS than PA. SuperPATH showed statistically worse results in operation time than PA. DAA showed statistically worse results in intraoperative blood loss than PA. The other outcomes in THA through DAA and PA were indifferent. SuperPATH showed statistically better results in intraoperative blood loss than DAA. The other outcomes in THA through SuperPATH and DAA were indifferent. All approaches showed sufficient results in acetabular cup positioning.
The value of this NMA comes from the inclusion of RCTs and the employment of high-quality statistical methods. We performed the NMA with both a fixed and a random effects model. Our NMA is an attempt to overcome the limitations of our previous NMAs2,3 by systematically and quantitatively reviewing literature comparing SuperPATH, DAA, and PA.
SuperPATH vs. DAA vs. PA
The mean operation time in our NMA ranged from 57 to 118 min. for SuperPATH, from 60 to 84 min. for DAA, and from 46 to 125 min. for PA. SuperPATH had a 17 min. longer operation time than PA. There was no difference in operation time between DAA vs. PA and SuperPATH vs. DAA. A prolonged operation time was found in other meta-analyses comparing SuperPATH with conventional approaches37,38,39. A 2018 meta-analysis by Wang et al.40 with 9 RCTs and 754 THAs showed no difference in operation time between DAA and PA. Wills et al. found that an operation time > 90 min. in THA leads to increased rates of superficial infections41. Surace et al. determined in an analysis of 89,802 THA cases that an optimal operation time of around 80 min. leads to a lower risk of perioperative complications42. The operational technique through SuperPATH and DAA is somewhat more complicated than through the conventional approaches. Because of this, SuperPATH and DAA have an extended learning curve for operating surgeons43,44. SuperPATH may have the potential for a shorter operation time as it is a novel approach.
The mean incision length in our NMA ranged from 6.9 to 10.4 cm for SuperPATH, from 9.1 to 13.7 cm for DAA, and from 9.1 to 15.2 cm for PA. SuperPATH had a 4.7 cm shorter incision length than PA. There was no difference in incision length between DAA vs. PA and SuperPATH vs. DAA. Several recent meta-analyses found a shorter incision length for SuperPATH compared to conventional approaches37,38,39,45, other meta-analyses found a shorter incision length for DAA compared to conventional approaches40,46. Both SuperPATH and DAA should aim for incision lengths of < 10 cm, as this is a requirement for minimally invasive hip surgery. As can be seen in the corresponding Forest plot, SuperPATH is more likely to meet this requirement. Nevertheless, a 2013 meta-analysis by Xu et al. with 14 RCTs and 1174 patients did not come to a definite overall conclusion on whether there is a relevant difference between mini-incision or standard incision in THA outcome47. On the other hand, a 2013 meta-analysis by Moskal et al. with 30 studies and 3548 THAs concluded that shorter incisions had a better short-term outcome after THA, compared to standard incisions48.
The mean intraoperative blood loss in our NMA ranged from 89 to 1108 ml for SuperPATH, from 166 to 391 ml for DAA, and from 123.8 to 844.6 ml for PA. SuperPATH had 82 ml lower intraoperative blood loss than PA. DAA had 92 ml higher intraoperative blood loss than PA and 174 ml higher intraoperative blood loss than SuperPATH. A lower blood loss for SuperPATH compared to conventional approaches was already found in earlier meta-analyses37,39. However, in our NMA DAA showed a higher blood loss than PA. A possible explanation is bleeding of branches of the lateral circumflex femoral artery, the ligation of which is sometimes problematic. Besides the approaches to the hip joint, other known factors that influence blood loss in hip surgery are the use of tranexamic acid and intraoperative active warming49,50,51.
The mean HHS 3 months postoperatively in our NMA ranged from 72.3 to 93.3 points for SuperPATH, from 85.9 to 91.2 points for DAA, and 78.0 to 91.4 points for PA. The mean HHS 6 months postoperatively in our NMA ranged from 84.3 to 95.8 points for SuperPATH, from 90.1 to 95.8 points for DAA, and from 79.7 to 95.9 points for PA. The mean HHS 12 months postoperatively in our NMA ranged from 85.6 to 94.7 points for SuperPATH, from 94.4 to 97.5 points for DAA, and from 86.6 to 97.3 points for PA. With regards to the postoperative functional outcome (HHS 3, 6, and 12 months postoperatively) SuperPATH demonstrated statistically superior results to PA. The difference in HHS decreased over time after surgery. SuperPATH had a 2.6 point higher HHS 3 months postoperatively, a 2.1 points higher HHS 6 months postoperatively, and a 0.6 points higher HHS 12 months postoperatively. This means that the strength of SuperPATH lies in the early functional outcome. However, when interpreting the results it is important to emphasize that differences in functional outcomes are not clinically relevant. The highest HHS difference noted in our NMA was 2.6 points at 3 months postoperatively. Although in the literature the minimal clinically important difference (MCID) for HHS varies according to different types of hip surgery52,53,54,55, it has been reported as no less than 7.9 points on the 0–100 HHS scale. There was no difference in HHS 3, 6, and 12 months postoperatively between DAA vs. PA and SuperPATH vs. DAA. Several meta-analyses on SuperPATH vs. conventional approaches came to similar conclusions37,38,39,45. In contrast to our findings, several meta-analyses showed better early functional results for DAA compared to conventional approaches40,46,56. However, HHS is a very important outcome parameter as it gives a comprehensive impression of the function of the operated hip.
The mean acetabular cup anteversion angle in our NMA ranged from 13.9° to 21.9° for SuperPATH, from 17.1° to 26.9° for DAA, and from 14.3° to 25.8° for PA. Each in another RCT, DAA33 and PA30 showed a slightly too large angle with 26.9° and 25.8°, respectively. The mean acetabular cup inclination angle in our NMA ranged from 36.9° to 43.9° for SuperPATH, from 37.0° to 47.1° for DAA, and from 39.6° to 46.5° for PA. In general, all approaches stayed within the widely accepted values for acetabular cup positioning: anteversion angle from 10° to 25° and inclination angle from 40° to 50°9. None of the included studies evaluated the restoration of the center of rotation of the native acetabulum, which could be affected during minimally invasive approaches, due to potential upward deviation of the acetabular reamers by the soft tissue tension. Furthermore, the assessment of the anteversion angle, in particular, is questionable, as none of the included RCTs used computed tomography (Table 1). In addition, both acetabular inclination and anteversion change between standing and supine conventional radiographs. Nevertheless, there was no relevant difference between SuperPATH, DAA, and PA in acetabular cup positioning.
Intra- and postoperative fractures, especially trochanteric fractures, infections, and hip dislocations are important complications that seem to show different patterns in certain approaches. Surgical revision rates, leg length discrepancies, and postoperative pain are also parameters often taken into consideration in comparisons of THA. Nevertheless, postoperative complications could not be compared due to the lack of consistent data in the RCTs included.
Limitations
In this NMA we addressed an important limitation of our previous NMAs2,3: we distinguished between each conventional approach and compared SuperPATH, DAA, and PA. The other restrictions remain unchanged: First, due to the lack of RCTs that directly compare SuperPATH and DAA, we provided an indirect comparison of both approaches, which offers weaker evidence. Second, the long-term outcomes of THA were not considered. Third, due to insufficient data, important outcome parameters such as hospitalization time, postoperative drainage volume, postoperative pain, and complications could not be considered. Fourth, this NMA did not consider the possible influence of the surgeon operating skills, the utilization of tranexamic acid and anticoagulants, bone cement, or the types of implants for hip replacement. Fifth, part of the RCTs did not give any information on what exact hip pathology was treated with THA. Sixth, since the SuperPATH approach is a 2-incision approach, it remains unclear whether the included RCTs reported the added incision length or the length of the larger incision, ignoring the smaller additional incision. Lastly, in some cases of the outcomes investigated, the heterogeneity of the included RCTs was high.
Conclusion
Our overall findings suggested that the short-term outcomes of THA through SuperPATH were statistically superior to PA. SuperPATH showed statistically better results in incision length, intraoperative blood loss, and functional outcome than PA. DAA and PA as well as SuperPATH and DAA showed overall indifferent short-term outcomes.
Data availability
The data are available from the corresponding author upon reasonable request.
Abbreviations
- BMI:
-
Body mass index
- CNKI:
-
China National Knowledge Infrastructure
- CI:
-
Confidence interval
- DAA:
-
Direct anterior approach
- HHS:
-
Harris Hip Score
- MD:
-
Mean difference
- NMA:
-
Network meta-analysis
- PA:
-
Posterior and posterolateral approach
- RCT:
-
Randomized controlled trial
- SuperPATH:
-
Supercapsular percutaneously assisted approach in total hip arthroplasty
- THA:
-
Total hip arthroplasty
References
Chow, J., Penenberg, B. & Murphy, S. Modified micro-superior percutaneously-assisted total hip: early experiences & case reports. Curr. Rev. Musculoskelet. Med. 4(3), 146–150. https://doi.org/10.1007/s12178-011-9090-y (2011).
Ramadanov, N., Bueschges, S., Liu, K., Lazaru, P. & Marintschev, I. Comparison of short-term outcomes between direct anterior approach (DAA) and SuperPATH in total hip replacement: A systematic review and network meta-analysis of randomized controlled trials. J. Orthop. Surg. Res. 16(1), 324. https://doi.org/10.1186/s13018-021-02315-7 (2021).
Ramadanov, N., Bueschges, S., Liu, K., Lazaru, P. & Marintschev, I. Direct anterior approach vs. SuperPATH vs. conventional approaches in total hip replacement: A network meta-analysis of randomized controlled trials. Orthop. Traumatol. Surg. Res. 107(8), 103058. https://doi.org/10.1016/j.otsr.2021.103058 (2021).
Putananon, C. et al. Comparison of direct anterior, lateral, posterior and posterior-2 approaches in total hip arthroplasty: network meta-analysis. Eur. J. Orthop. Surg. Traumatol. 28(2), 255–267. https://doi.org/10.1007/s00590-017-2046-1 (2018).
Amlie, E. et al. Worse patient-reported outcome after lateral approach than after anterior and posterolateral approach in primary hip arthroplasty: A cross-sectional questionnaire study of 1,476 patients 1–3 years after surgery. Acta Orthop. 85(5), 463–469. https://doi.org/10.3109/17453674.2014.934183 (2014).
Peters, R. M. et al. Similar Superior Patient-Reported Outcome Measures for Anterior and Posterolateral Approaches After Total Hip Arthroplasty: Postoperative Patient-Reported Outcome Measure Improvement After 3 months in 12,774 Primary Total Hip Arthroplasties Using the Anterior, Anterolateral, Straight Lateral, or Posterolateral Approach. J. Arthroplasty. 33(6), 1786–1793. https://doi.org/10.1016/j.arth.2018.01.055 (2018).
Hutton, B. et al. The PRISMA extension statement for reporting of systematic reviews incorporating network meta-analyses of health care interventions: Checklist and explanations. Ann Intern. Med. 162(11), 777–784. https://doi.org/10.7326/M14-2385 (2015).
Harris, W. H. Traumatic arthritis of the hip after dislocation and acetabular fractures. Treatment by mold arthroplasty. An end-result study using a new method of result evaluation. J. Bone Jt. Surg. Am. 51, 737–755 (1969).
Tan, S. C. et al. Effect of taper design on Trunnionosis in metal on polyethylene total hip arthroplasty. J. Arthroplasty. 30, 1269–1272 (2015).
Sterne, J. A. C. et al. RoB 2: A revised tool for assessing risk of bias in randomised trials. BMJ 28, 366. https://doi.org/10.1136/bmj.l4898 (2019).
Guyatt, G. H. et al. GRADE: An emerging consensus on rating quality of evidence and strength of recommendations. BMJ 336(7650), 924–926. https://doi.org/10.1136/bmj.39489.470347.AD (2008).
Deeks, J. J., Higgins, J. P. T., Altman, D. G. (editors). Chapter 10: Analysing data and undertaking meta-analyses. In: Higgins, J. P. T., Thomas, J., Chandler, J., Cumpston, M., Li, T., Page, M. J., Welch, V. A. (editors). Cochrane Handbook for Systematic Reviews of Interventions version 6.0 (updated July 2019). Cochrane, 2019. www.training.cochrane.org/handbook. Accessed 31 October 2021.
Schünemann, H. J., Vist, G. E., Higgins, J. P. T., Santesso, N., Deeks, J. J., Glasziou, P., Akl, E. A., Guyatt, G. H. Chapter 15: Interpreting results and drawing conclusions. In: Higgins, J. P. T., Thomas, J., Chandler, J., Cumpston, M., Li, T., Page, M. J., Welch, V. A. (editors). Cochrane Handbook for Systematic Reviews of Interventions version 6.0 (updated July 2019). Cochrane, 2019. www.training.cochrane.org/handbook.
Seide, S. E., Jensen, K. & Kieser, M. A comparison of Bayesian and frequentist methods in random-effects network meta-analysis of binary data. Res. Synth. Methods. 11(3), 363–378. https://doi.org/10.1002/jrsm.1397 (2020).
Neupane, B., Richer, D., Bonner, A. J., Kibret, T. & Beyene, J. Network meta-analysis using R: a review of currently available automated packages. PLoS ONE 9(12), 115065. https://doi.org/10.1371/journal.pone.0115065 (2015).
Higgins, J. P. & Thompson, S. G. Quantifying heterogeneity in a meta-analysis. Stat. Med. 21, 1539–1558 (2002).
Gao, P. & Shi, X. The effect of total hip replacement with minimally invasive SuperPATH approach in the treatment of elderly femoral neck fractures (Article in Chinese). Henan Med. Res. 29(20), 1 (2020).
Li, L. SuperPATH minimally invasive total hip replacement surgery treatment: Analysis of clinical efficacy of aseptic necrosis of femoral head (Article in Chinese). Chin. J. Mod. Drug. Appl. 14(12), 1 (2020).
Li, X., Ma, L., Wang, Q. & Rong, K. Comparison of total hip arthroplasty with minimally invasive SuperPath approach vs. conventional posterolateral approach in elderly patients: A one-year follow-up randomized controlled research. Asian J. Surg. 44(3), 531–536. https://doi.org/10.1016/j.asjsur.2020.11.014 (2021).
Liu, Y., Hu, P., Zhu, J., She, H. & Zhang, Y. The effect of artificial minimally invasive total hip replacement in the treatment of femoral neck fractures in the elderly (Article in Chinese). Prac. J. Med. & Pharm. 38(3), 1. https://doi.org/10.14172/j.issn1671-4008.2021.03.010 (2021).
Meng, W. et al. Supercapsular percutaneously-assisted total hip (SuperPath) versus posterolateral total hip arthroplasty in bilateral osteonecrosis of the femoral head: A pilot clinical trial. BMC Musculoskelet. Disord. 21(1), 2. https://doi.org/10.1186/s12891-019-3023-0 (2019).
Meng, W. et al. Supercapsular percutaneously-assisted total hip (SuperPath) versus mini-incision posterolateral total hip arthroplasty for hip osteoarthritis: a prospective randomized controlled trial. Ann. Transl. Med. 9(5), 392. https://doi.org/10.21037/atm-20-1793a (2021).
Ouyang, C. et al. Randomized controlled trial of comparison between the SuperPATH and posterolateral approaches in total hip arthroplasty (Article in Chinese). Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi 32(12), 1500–1506. https://doi.org/10.7507/1002-1892.201807011 (2018).
Pan, Y. et al. Comparison of SuperPATH and posterolateral total hip replacement (Article in Chinese). Orthop. J. China 28(13), 1 (2020).
Wang, Z. & Ge, W. SuperPATH approach total hip replacement for elderly patients with femoral neck fracture: Impact of hip function (Article in Chinese). Clin. Med. 41(1), 1. https://doi.org/10.1928/j.issn.1003-3548.2021.01.010 (2021).
Xie, J. et al. Comparison of supercapsular percutaneously assisted approach total hip versus conventional posterior approach for total hip arthroplasty: A prospective, randomized controlled trial. J. Orthop. Surg. Res. 12(1), 138. https://doi.org/10.1186/s13018-017-0636-6 (2017).
Yuan, H., Zhu, J., Sun, Z. & Zhang, Z. Comparison of effectiveness between SuperPATH approach and posterolateral approach in total hip arthroplasty (Article in Chinese). Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi 32(1), 14–19. https://doi.org/10.7507/1002-1892.201707121 (2018).
Zhang, Z., Lin, J. & Xia, B. Clinical research on joint function and life quality through SuperPath approach in total hip arthroplasty (Article in Chinese). China J. Integrat. Trad. Chin. Western Med. 25(5), 709–714 (2019).
Zunlong, L., Pinghui, Z. & Yu, F. Analysis of the effect of total hip replacement via SuperPATH approach on the prognosis of elderly patients with femoral neck fracture. Chin. J. Med. Front. 12(5), 1. https://doi.org/10.10237/YXQY.2020.05-10 (2020).
Barrett, W. P., Turner, S. E. & Leopold, J. P. Prospective randomized study of direct anterior vs postero-lateral approach for total hip arthroplasty. J. Arthroplasty. 28(9), 1634–1638. https://doi.org/10.1016/j.arth.2013.01.034 (2013).
Bon, G. et al. Does the direct anterior approach allow earlier recovery of walking following total hip arthroplasty? A randomized prospective trial using accelerometry. Orthop. Traumatol. Surg. Res. 105(3), 445–452. https://doi.org/10.1016/j.otsr.2019.02.008 (2019).
Cheng, T. E. et al. A Prospective Randomized Clinical Trial in Total Hip Arthroplasty-Comparing Early Results Between the Direct Anterior Approach and the Posterior Approach. J Arthroplasty. 32(3), 883–890. https://doi.org/10.1016/j.arth.2016.08.027 (2017).
Moerenhout, K., et al. Direct anterior versus posterior approach for total hip arthroplasty: a multicentre, prospective, randomized clinical trial. Can J Surg. 63(5), E412–E417. https://doi.org/10.1503/cjs.012019 (2020).
Rykov, K., Reininga, I. H. F., Sietsma, M. S., Knobben, B. A. S. & Ten Have, B. L. E. F. Posterolateral vs Direct Anterior Approach in Total Hip Arthroplasty (POLADA Trial): A Randomized Controlled Trial to Assess Differences in Serum Markers. J Arthroplasty 32(12), 3652–3658. https://doi.org/10.1016/j.arth.2017.07.008 (2017).
Taunton, M. J., Trousdale, R. T., Sierra, R. J., Kaufman, K. & Pagnano, M. W. John Charnley Award: Randomized Clinical Trial of Direct Anterior and Miniposterior Approach THA: Which Provides Better Functional Recovery?. Clin Orthop Relat Res. 476(2), 216–229. https://doi.org/10.1007/s11999.0000000000000112 (2018).
Zhao, H. Y. et al. Comparison of Early Functional Recovery After Total Hip Arthroplasty Using a Direct Anterior or Posterolateral Approach: A Randomized Controlled Trial. J Arthroplasty. 32(11), 3421–3428. https://doi.org/10.1016/j.arth.2017.05.056 (2017).
Li, J., Qiu, B. & Zhen, D. Meta-analysis on clinical outcomes of the SuperPATH approach versus traditional approach in hip arthroplasty (Article in Chinese). J. Clin. Reh. Tiss. Eng. Res. 22(15), 2453–2460. https://doi.org/10.3969/j.issn.2095-4344.0194 (2018).
Ramadanov, N., Bueschges, S., Liu, K., Klein, R. & Schultka, R. Comparison of short-term outcomes between SuperPATH approach and conventional approaches in hip replacement: A systematic review and meta-analysis of randomized controlled trials. J. Orthop. Surg. Res. 17(1), 420. https://doi.org/10.1186/s13018-020-01884-3 (2020).
Ramadanov, N. An updated meta-analysis of randomized controlled trials on total hip arthroplasty through SuperPATH versus conventional approaches. Orthop. Surg. 14(5), 807–823. https://doi.org/10.1111/os.13239 (2022).
Wang, Z. et al. A systematic review and meta-analysis of direct anterior approach versus posterior approach in total hip arthroplasty. J. Orthop. Surg. Res. 13(229), 1. https://doi.org/10.1186/s13018-018-0929-4 (2018).
Wills, B. W. et al. Impact of operative time on early joint infection and deep vein thrombosis in primary total hip arthroplasty. Orthop. Traumatol. Surg. Res. 104(4), 445–448. https://doi.org/10.1016/j.otsr.2018.02.008 (2018).
Surace, P. et al. The Association Between Operative Time and Short-Term Complications in Total Hip Arthroplasty: An Analysis of 89,802 Surgeries. J. Arthroplasty. 34(3), 426–432. https://doi.org/10.1016/j.arth.2018.11.015 (2019).
Rasuli, K. J. & Gofton, W. Percutaneously assisted total hip (PATH) and Supercapsular percutaneously assisted total hip (SuperPATH) arthroplasty: learning curves and early outcomes. Ann. Transl. Med. 13(179), 1. https://doi.org/10.3978/j.issn.2305-5839.2015.08.02 (2015).
Van Den Eeden, Y. & Van Den Eeden, F. Learning curve of direct anterior total hip arthroplasty: A single surgeon experience. Acta Orthop. Belg. 84(3), 321–330 (2018).
Sun, Z., Li, H., Yang, H. & Min, J. Systematic review on the curative effect of total hip arthroplasty through supercapsular percutaneously—assisted total hip approach versus posterolateral approach for treatment of hip diseases (Article in Chinese). J. Trad. Chin Orth. 30(1), 32–37 (2018).
Kucukdurmaz, F., Sukeik, M. & Parvizi, J. A meta-analysis comparing the direct anterior with other approaches in primary total hip arthroplasty. Surgeon 17(5), 291–299. https://doi.org/10.1016/j.surge.2018.09.001 (2019).
Xu, C. P., Li, X., Song, J. Q., Cui, Z. & Yu, B. Mini-incision versus standard incision total hip arthroplasty regarding surgical outcomes: A systematic review and meta-analysis of randomized controlled trials. PLoS ONE 8(11), 80021. https://doi.org/10.1371/journal.pone.0080021 (2013).
Moskal, J. T. & Capps, S. G. Is limited incision better than standard total hip arthroplasty? A meta-analysis. Clin. Orthop. Relat. Res. 471(4), 1283–1294. https://doi.org/10.1007/s11999-012-2717-5 (2013).
Qi, Y. M. et al. The efficacy and safety of intravenous tranexamic acid in hip fracture surgery: A systematic review and meta-analysis. J. Orthop. Transl. 19, 1–11. https://doi.org/10.1016/j.jot.2019.03.007 (2019).
Fillingham, Y. A. et al. The efficacy of tranexamic acid in total hip arthroplasty: A network meta-analysis. J Arthroplasty. 33(10), 3083–3089. https://doi.org/10.1016/j.arth.2018.06.023 (2018).
Yi, J., Liang, H., Song, R., Xia, H. & Huang, Y. Maintaining intraoperative normothermia reduces blood loss in patients undergoing major operations: A pilot randomized controlled clinical trial. BMC Anesthesiol. 18(1), 126. https://doi.org/10.1186/s12871-018-0582-9 (2018).
Singh, J. A., Schleck, C., Harmsen, S. & Lewallen, D. Clinically important improvement thresholds for Harris Hip Score and its ability to predict revision risk after primary total hip arthroplasty. BMC Musculoskelet Disord. 17, 256. https://doi.org/10.1186/s12891-016-1106-8 (2016).
Kemp, J. L., Collins, N. J., Roos, E. M. & Crossley, K. M. Psychometric properties of patient-reported outcome measures for hip arthroscopic surgery. Am. J. Sports Med. 41(9), 2065–2073. https://doi.org/10.1177/0363546513494173 (2013).
van der Wees, P. J. et al. Patient-reported health outcomes after total hip and knee surgery in a Dutch University Hospital Setting: Results of twenty years clinical registry. BMC Musculoskelet. Disord. 18(1), 97. https://doi.org/10.1186/s12891-017-1455-y (2017).
Nwachukwu, B. U. et al. Minimal clinically important difference and substantial clinical benefit after revision hip arthroscopy. Arthroscopy 34(6), 1862–1868. https://doi.org/10.1016/j.arthro.2018.01.050 (2018).
Yue, C., Kang, P. & Pei, F. Comparison of Direct Anterior and Lateral Approaches in Total Hip Arthroplasty: A Systematic Review and Meta-Analysis (PRISMA). Medicine (Baltimore) 94(50), 2126. https://doi.org/10.1097/MD.0000000000002126 (2015).
Funding
Open Access funding enabled and organized by Projekt DEAL. We acknowledge the funding by the MHB Open Access Publication Fund supported by the German Research Association (DFG).
Author information
Authors and Affiliations
Contributions
N.R. wrote the manuscript. S.B. and N.R. did the statistics. K.L. helped with Chinese translation. I.M., N.R., and P.L. checked the final version.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Ramadanov, N., Bueschges, S., Liu, K. et al. Direct and indirect comparisons in network meta-analysis of SuperPATH, direct anterior and posterior approaches in total hip arthroplasty. Sci Rep 12, 16778 (2022). https://doi.org/10.1038/s41598-022-20242-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-022-20242-3
This article is cited by
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.