Abstract
Utilizing automatic daily body weight (BW) measurements may be helpful for assessing nutritional status and detecting underlying diseases particularly in older people who require nursing care. This preliminary study aimed to verify effectiveness of eating assistance for maintaining BW in older people using a contact-free load cells under the bed (Bed Sensor System: BSS). BW was measured every night for 3 months in eight nursing home older people with severe cognitive and physical dysfunctions. Body composition of the subject's trunk and each limb was measured using a segmented multi-frequency bioelectrical impedance analyzer (BIA). A monthly BW loss was estimated as a slope of linear regression of the daily BW plot. BSS successfully measured daily BW for the study period in all participants. The 4 residents with eating assistance gained slightly more weight, while the 4 residents without eating assistance lost weight. There was a significant difference between the two groups in the monthly BW change (− 0.79 ± 0.51 kg/month versus 0.20 ± 0.49 kg/month, P = 0.030). None of the BIA-derived parameters was associated with the monthly BW change. BSS revealed effectiveness of eating assistance to maintain BW in nursing home residents with severe cognitive and physical dysfunctions.
Similar content being viewed by others
Introduction
Weight loss is a bio-maker for malnutrition, frailty and the end of life in older people1,2,3. Older nursing home residents who need high levels of nursing home care are at higher risk of weight loss4. High-level care dependency and unexpected weight loss are the main factors for the decline of nutritional status in nursing home residents5. Eating assistance is commonly provided to older residents aiming for improving their nutritional status. In fact, by measuring body weight every month for a year in nursing home residents with low oral intake, eating assistance either twice per day during or between meals was demonstrated to successfully prevent weight loss6. Certainly, frequent body weight measurements serve to assess effectiveness of the eating assistance.
Despite importance of early detection of weight loss and intervention of eating assistance, frequent body weight measurements are difficult laborious task in nursing homes due to lack of staffs and limited physical functions of the older people. Because of the difficulties, little information is available regarding long-term body weight change and effectiveness of eating assistance in the nursing home residents with impairment of cognitive and physical performances which are common features of Japanese nursing home residents7. In this context, development of early and accurate diagnostic tools for weight loss without laborious burden to the nursing home staffs may improve nursing home care for older people.
We have developed a contact-free unconstraint vital sign monitor using high resolution strain gauge load cells placed under the bed legs (Bed Sensor Vital Sign Monitoring System: BSS, Minebea-Mitsumi, Nagano, Japan), allowing long-term continuous automatic measurements of body weight, time spending on bed, and vital signs including respiratory rate. We have already reported its accuracy for assessments of the respiratory status of healthy subjects8 and advanced cancer patients9. The purpose of this study is to test whether the BSS can be used in nursing home older patients to determine if mealtime assistance is effective in maintaining their weight.
Methods
Study design and participants
This observational study was approved by the Ethics Committee of the Graduate School of Nursing, Chiba University (Accreditation Number 29-27). The subjects of this study were older people living in a nursing home. After reviewing the cognitive and physical status of the residents with nursing staffs, we selected residents who are older than 75 years and require high levels of nursing care due to moderate to severe difficulties of physical and cognitive performance. The purposes and risks of this study were fully explained to the candidate residents and their families, and a written informed consent was obtained from each.
Body composition was routinely assessed at admission using a segmental multifrequency bioelectrical impedance analysis (BIA) device (InBody S10; Biospace, Koto-ku, Tokyo, Japan), which measured the body composition of the trunk and each limb separately in addition to a total body weight. Several BIA-derived parameters such as Skeletal Muscle Index, Body Fat, and Basal Metabolic Rate were obtained.
Unconstraint under-bed vital sign monitoring for continuous body weight measurements
A contact-free unconstraint vital sign monitor using high resolution strain gauge load cells placed under the bed legs (Bed Sensor Vital Sign Monitoring System: BSS, Minebea-Mitsumi, Nagano, Japan) was used for continuous measurements of body weight and body movement parameters on the bed every minute. The BSS measurements were continued for more than 3 months without restricting routine care and daily activities. Among the BSS data collected during the nighttime hours from 2:00 a.m. to 3:00 a.m., body weight data with minimum body movements were selected and the values greater than one standard deviation were excluded as outliers. A single value of body weight for the day was determined as a median of the selected body weight data. With using the daily body weight data for the 3 months, monthly body weight loss was estimated as a slope of the linear regression line (kg/month).
Data analysis
Based on the participants’ eating dependence, we compared the variables between participants with and without eating assistance (self-eating group: S-group versus eating assistance group: A-group). Variables were expressed as means and standard deviations. Comparisons between the groups were performed with independent t-test and Fisher’s exact test for continuous and categorical data, respectively (SigmaPlot 12.0; Systat Software Inc., Point Richmond, CA). A value of p < 0.05 was considered statistically significant, and all p-values were two sided.
Ethics approval
The study protocol was approved by the Ethics Committee of the Graduate School of Nursing, Chiba University. All experiments were performed in accordance with relevant guidelines and regulations. Informed consent was obtained from all participants and/or their legal guardians. All Research have been performed in accordance with the Declaration of Helsinki.
Results
Background differences between the groups
Eight older residents participated in this study (Table 1). All participants needed high levels of nursing care either due to cognitive or physical dysfunctions while none had paralysis of their extremities. Based on eating dependency, four participants were classified into S-group and the other four participants were classified into A-group. Body weight, Body Mass Index, Skeletal Muscle Index and percentage of body fat did not differ between the two groups. Basal Metabolic Rate was slightly but significantly higher in S-group than A-group. Caloric intake tended to be higher in S-group.
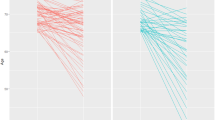
Monthly body weight loss
All 4 participants of S-group lost weight whereas 3 A-group participants did not lose weight during the 3-month study period. The A-group gained slightly more weight, while the S-group lost weight. There was a significant difference between the two groups in the monthly BW change (− 0.79 ± 0.51 kg/month versus 0.20 ± 0.49 kg/month, P = 0.030) (Fig. 1). None of the BIA-derived parameters was associated with the monthly body weight change.
Discussion
In this preliminary observational study, we succeeded in automatic unconstrained daily body weight measurements for 3 months and estimated monthly body weight loss in nursing care residents with severe cognitive and physical dysfunctions. Monthly body weight loss was significantly greater in the residents without eating assistance than in those with eating assistance. Continuous body weight measurements with unconstraint under-bed vital sign monitoring may serve for assessing trends of nutritional status and general conditions in nursing home older people.
Potential early recognition of weight loss with unconstraint under-bed vital sign monitoring for automatic daily body weight measurements
Weight loss has been reported to be an independent risk factor for death among older people in nursing homes1,10. A significant association between weight loss of 5 kg or more in a year and death within 6 months was documented2. Furthermore, one of the diagnostic criteria for frailty is a weight loss of 2–3 kg in 6 months3. Therefore, accurate diagnosis of weight loss requires long-term monthly body weight measurements as reported in many previous studies. However, such long-term diagnosis period may delay appropriate interventions for preventing development of malnutrition and frailty as the frailty-related diseases may have already progressed by the time of its diagnosis. Clearly, continuous assessments of monthly weight loss estimated by automatic daily body weight measurements used in this study are advantageous for early detection of frailty and potential end stage of the life over the conventional manual body weight measurements which are laborious and difficult in older people with physical disabilities. In fact, we identified three S-group participants and one A-group participant fulfilling the frailty criteria.
Dietary intake methods and body weight loss
This is the first study assessing effectiveness of eating assistance for maintaining body weight of older nursing care residents with cognitive and physical dysfunctions. It has been previously reported that appropriate interventions for the elderly in nursing homes may improve weight loss in a comparison between groups requiring dietary assistance11,12. We found monthly body weight loss was significantly greater in the residents without eating assistance than in those with eating assistance. As discussed above, the weight loss detected in the residents without eating assistance fulfills the frailty criteria, and the potentially-pathological weight loss information could be used as an early alert for malnutrition. Previous studies have reported that delayed awareness of a gradual functional decline in dietary intake among nursing home staffs leads to weight loss and malnutrition in the residents, ultimately increasing the risk of death13. Despite importance of accurate dietary intake assessment, it is very difficult to objectively assess a gradual decline of the dietary intake. Furthermore, insufficient manpower in the nursing home, a common situation in Japan, was reported to be associated with weight loss of the residents14. Based on early recognition of weight loss by means of automatic daily body weight measurements, caregivers efficiently determine residents who really need eating assistance for recovering from the frailty process.
Limitations of the study
There are several limitations to this study. First, the number of subjects in this study was small, which has insufficient statistical power. Also, there was low uniformity among the individual older. However, the analysis was performed after confirming that there were no significant differences between the S and A-group in terms of body composition using BIA, Calorie intake, and Calorie intake/Basal metabolic rate. Despite the limited number of subjects, it is interesting to note that the dietary assistance group maintained their weight significantly better than the independent diet group. In addition, it is very important to minimize the loss of lean body mass in the older people, but in this study, the observation period was short and it has not yet been possible to examine whether the suppression of weight loss by dietary assistance directly leads to the suppression of muscle mass loss. We plan to solve these problems by continuing this study in the future.
In conclusion, monthly body weight change can be estimated by automatic daily body weight measurements with unconstraint under-bed vital sign monitoring in nursing home residents with severe cognitive and physical dysfunctions. Eating assistance serves for maintaining body weight possibly preventing development of frailty.
Data availability
Under request to the corresponding author.
References
Hanson, L. C., Ersek, M., Lin, F. C. & Carey, T. S. Outcomes of feeding problems in advanced dementia in a nursing home population. J. Am. Geriatr. Soc. 61, 692–1697. https://doi.org/10.1111/jgs.12448 (2013).
Wirth, R. et al. The impact of weight loss and low BMI on mortality of nursing home residents—Results from the nutrition Day in nursing homes. Clin. Nutr. 35, 900–906. https://doi.org/10.1016/j.clnu.2015.06.003 (2016).
Fried, L. P. et al. Frailty in older adults: Evidence for a phenotype. J. Gerontol. A Biol. Sci. Med. Sci. 56, 146–156. https://doi.org/10.1093/gerona/56.3.m146 (2001).
Murden, R. A. & Ainslie, N. K. Recent weight loss is related to short-term mortality in nursing homes. J. Gen. Intern. Med. 9, 648–650. https://doi.org/10.1007/BF02600311 (1994).
Bauer, S., Halfens, R. J. G. & Lohrmann, C. Changes in nutritional status in nursing home residents and associated factors in nutritional status decline: A secondary data analysis. J. Adv. Nurs. 73, 2420–2429. https://doi.org/10.1111/jan.13297 (2017).
Simmons, S. F. et al. Prevention of unintentional weight loss in nursing home residents: A controlled trial of feeding assistance. J. Am. Geriatr. Soc. 56, 1466–1473. https://doi.org/10.1111/j.1532-5415.2008.01801.x (2008).
Fetherstonhaugh, D., Haesler, E. & Bauer, M. Promoting mealtime function in people with dementia: A systematic review of studies undertaken in residential aged care. Int. J. Nurs. Stud. 96, 99–118. https://doi.org/10.1016/j.ijnurstu.2019.04.005 (2019).
Isono, S. et al. Contact-free unconstraint respiratory measurements with load cells under the bed in awake healthy volunteers: Breath-by-breath comparison with pneumotachography. J. Appl. Physiol. 126, 1432–1441. https://doi.org/10.1152/japplphysiol.00730.2018 (2019).
Hasegawa, M. et al. Effects of opioids on respiration assessed by a contact-free unconstraint respiratory monitor with load cells under the bed in advanced cancer patients. J. Appl. Physiol. https://doi.org/10.1152/japplphysiol.00904.2020 (2021).
Alley, D. E. et al. Changes in weight at the end of life: Characterizing weight loss by time to death in a cohort study of older men. Am. J. Epidemiol 172, 558–565. https://doi.org/10.1093/aje/kwq168 (2010).
Palecek, E. J. et al. Comfort feeding only: A proposal to bring clarity to decision-making regarding difficulty with eating for persons with advanced dementia. J. Am. Geriatr. Soc. 58, 580–584. https://doi.org/10.1111/j.1532-5415.2010.02740.x (2010).
Rantz, M. J. et al. Randomized multilevel intervention to improve outcomes of residents in nursing homes in need of improvement. J. Am. Med. Dir. Assoc. 13, 60–682. https://doi.org/10.1016/j.jamda.2011.06.012 (2012).
Ito, K., Kanehisa, Y., Yamada, R. & Yoshihara, A. Self-feeding ability as a predictor of mortality Japanese nursing home residents: A two-year longitudinal study. J. Nutr. Health Aging 23, 157–164. https://doi.org/10.1007/s12603-018-1125-2 (2019).
Tamura, B. K. et al. Factors associated with weight loss, low BMI, and malnutrition among nursing home patients: A systematic review of the literature. J. Am. Med. Dir. Assoc. 14, 649–655. https://doi.org/10.1016/j.jamda.2013.02.022 (2013).
Disclosure
This study used data obtained during collaborative research between Chiba University and Minebea-Mitsumi Inc. The funders had no role in data analysis.
Author information
Authors and Affiliations
Contributions
T.I. designed the study, analysis and interpretation of data, and wrote the initial draft of the manuscript. I.S. and S.I. contributed to analysis and interpretation of data and involved in important revision of the manuscript. A.A., R.K. and S.S. collected of date, contributed to analysis of data and critically reviewed the manuscript. I.S. and S.I. involved in supervise the project. All authors discussed the results and contributed to the final manuscript.
Corresponding author
Ethics declarations
Competing interests
Takahiro Ishikawa, Ikuko Sakai, Ayumi Amemiya, Ryou Komatsu and Shoko Sakuraba declare no competing interests. Siroh Isono received scholarship donations from Minebea-Mitsumi Inc. as head of the Department of Anesthesiology, Chiba University.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Ishikawa, T., Sakai, I., Amemiya, A. et al. Long-term body weight change assessed by non-contact load cells under the bed in older people with and without eating assistance: a preliminary study. Sci Rep 12, 8107 (2022). https://doi.org/10.1038/s41598-022-12291-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-022-12291-5
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.