Abstract
While retrospective studies have compared the efficacy of anti–tumour necrosis factor (TNF) agents and tacrolimus (TAC) in ulcerative colitis (UC), information regarding first-time use of these agents is limited. The aim of our study was to investigate the short- and long-term efficacy of anti-TNF agents [adalimumab (ADA) and infliximab (IFX)] and TAC in anti-TNF agent- and TAC-naïve steroid-refractory UC patients. We evaluated 150 steroid-refractory UC patients receiving anti-TNF agents (IFX: n = 30, ADA: n = 41) or TAC (n = 79) at eight institutions in Japan. Clinical response rates at 8 weeks were 73.2% and 75.9% while remission rates were 30.1% and 25.3% in the anti-TNF and TAC groups, respectively. Logistic regression analysis showed the male sex and higher C-reactive protein to be independent factors for response to anti-TNF agents and TAC, respectively. Use of TAC was an independent factor for relapse. No differences in response to the treatment or relapse were observed between IFX and ADA. In conclusion, TAC and anti-TNF agents promoted similar short-term effects, but anti-TNF agents ensured better long-term outcomes at first-time treatment of steroid-refractory UC patients.
Similar content being viewed by others
Introduction
Ulcerative colitis (UC) is a disabling chronic inflammatory condition of the large intestine of unknown aetiology. Moreover, UC markedly impairs patients' quality of life due to its symptoms such as diarrhoea, bloody stool, abdominal cramps, and faecal urgency1,2. Conventional therapeutic options including 5-aminosalicylates as first-line therapy and corticosteroids as second-line therapy, are effective in inducing remission in the majority of UC patients. However, 20–50% of patients are either resistant to or dependent on steroids3,4,5. Additionally, a subset of the patients is not able to tolerate steroid therapy due to side effects such as worsening of diabetes, osteoporosis, and high blood pressure.
Third-line therapies for steroid-refractory UC such as anti–tumour necrosis factor (TNF) agents or tacrolimus (TAC) are usually considered at this point. The efficacy of anti-TNF agents has been established in randomized controlled trials (RCTs). Infliximab (IFX) was the first anti-TNF agent to demonstrate efficacy in achieving and maintaining clinical remission and response in moderate-to-severe UC in the ACT1 and ACT2 trials6,7. Additionally, the efficacy of adalimumab (ADA) and golimumab for the induction and maintenance of remission was also established in the ULTRA1, ULTRA2, ULTRA38,9,10, and PURSUIT trials11,12. The calcineurin inhibitor, TAC, similar to ciclosporin (CsA), has been reported to exert a more potent immunosuppressive effect with less severe adverse events compared to CsA13,14,15. In clinical practice, ADA as well as TAC have been reported to be effective, especially in anti-TNF agent–naïve patients16,17. The efficacy of TAC in achieving steroid-refractory UC clinical remission was also demonstrated by RCTs18,19. However, the efficiency of TAC in maintaining remission is largely unknown. Therefore, in Japan, TAC is currently being employed as an induction therapy to be given for 3 months, but not as a maintenance therapy.
To date, there is no RCT comparing the efficacy of anti-TNF agents with TAC, but there are several reports of retrospective observational studies conducted in Japan20,21,22,23,24,25,26, where both IFX and TAC appeared to be equally safe and effective as induction therapy. However, most of these studies have investigated the use of IFX and TAC, and data including ADA are rather limited21,24. Further, the majority of these studies included either anti-TNF agent–experienced or TAC-experienced patients. Because the response rate of these agents may vary between first time use and experienced cases, further investigation focusing on either condition are required.
Therefore, the present study aimed to assess the contributing factors for effectiveness, and to compare the safety between anti-TNF agents including ADA, and TAC in anti-TNF agent–naïve and TAC-naïve steroid-refractory UC patients.
Methods
Study design and patients
This was a multicentre retrospective observational study of steroid-refractory UC patients receiving anti-TNF agents or TAC between March 2010 and March 2017. A total of eight medical sites including Nagasaki University Hospital and its related facilities were involved. This study was performed in accordance with the ethical guidelines of the Declaration of Helsinki and was reviewed and approved by the Nagasaki University Hospital Ethics Committee (Approval number: 16092630-2) before initiation. Informed consent was obtained in the form of opt-out on the website. Patients who did not provide informed consent were excluded from this study: this opt-out consent method was also approved by Nagasaki University Hospital Ethics Committee.
Patients who did not provide informed consent were excluded from this study. The diagnosis of UC was confirmed according to standardized criteria by prior clinical assessment, endoscopy, and histology. Patients who failed to complete 12 weeks of follow-up due to relocation were excluded from the final analysis.
Treatment protocol
The IFX was administered at a dose of 5 mg/kg at 0, 2, and 6 weeks and then every 8 weeks thereafter. The ADA was administered at an initial dose of 160 mg and a second dose of 80 mg with a 2-week induction interval. Thereafter, ADA 40 mg was administered every other week. However, IFX or ADA dose intensification was not included in this study because it is not currently approved in Japan. The TAC was administered orally at an initial dose of 0.1 mg/kg/day in two divided doses. The doses of TAC were adjusted to achieve first a blood trough level of 10 to 15 ng/mL until week 2, and then a level of 5 to 10 ng/mL thereafter. At week 12, TAC was discontinued based on the rules provided by the Japanese healthcare system. The attending physicians at each site selected from among these protocols at their discretion. All the treatment protocols were conducted according to evidence-based clinical guidelines for Inflammatory Bowel Disease developed by the Japanese Society of Gastroenterology27.
Data collection
A shared common database was used to collect demographic and clinical data relevant to this study. Data collected at baseline included gender, age, disease duration, disease extension, concomitant medications, C-reactive protein (CRP) level, partial Mayo score (pMS), and Mayo endoscopic score (MES). Disease activity was evaluated using the CRP level, pMS, and MES. The date of and reason for treatment discontinuation, requirement for further rescue therapy, and any adverse events were also recorded.
Definitions
We defined clinical remission as a pMS less than two points together with a score of zero points in the rectal bleeding section. Clinical response was defined as a decrease in pMS by three or more points from baseline. Relapse was defined as the occurrence of any UC clinical symptoms requiring further rescue therapy. Steroid-refractory UC was defined as either steroid resistance or dependence. Steroid resistance was defined as the absence of a response to an oral or intravenous prednisolone dose of more than 30 mg/day for 1 to 2 weeks. Steroid dependence was defined when prednisolone could not be reduced to less than 10 mg/day without disease recurrence or relapse occurring within 3 months of stopping prednisolone.
Endpoints
The primary endpoints of the study were rates of clinical remission and response at 8 weeks. The secondary endpoints were cumulative relapse-free rates. Long-term outcomes were evaluated using data from patients who were followed up for more than 6 months after IFX, ADA, or TAC treatment.
Statistical analysis
Statistical analysis was performed by a statistician (HK). Differences in quantitative parameters between the two groups were assessed with the Wilcoxon rank sum test. Fisher’s exact test was used for analysis of categorical data. Differences in the values between the two time periods for each patient were assessed using the Wilcoxon signed rank test. Logistic regression was employed to estimate odds ratios (ORs) and 95% confidence intervals (CIs) for each factor that contributed to remission or effectiveness of the drugs in 8 weeks. The Cox proportional hazard model with person-days as the underlying metric was employed to estimate hazard ratios (HRs) and 95% CIs of each risk factor for relapse of the UC. All statistical tests were two-sided, and p-values of less than 0.05 were considered to be statistically significant. The calculations were performed using the LOGISTIC and PHREG procedures in the SAS software package (version 9.4; SAS Institute, Inc., Cary, NC, USA).
Results
Patient demographics
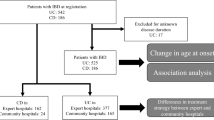
A total of 150 cases were analysed. Seventy-one individuals were treated with anti-TNF agents, and 79 individuals received TAC (Fig. 1). Baseline characteristics of the 150 study participants are presented in Table 1. Among these patients, the mean age was 46.2 ± 16.7 years, 51.3% were men, the mean disease duration was 90.8 ± 89.9 months, and 64.7% had total colitis. No differences were found with respect to epidemiologic characteristics between the anti-TNF and TAC groups, except for disease extension. The proportion of patients with total colitis, rate of hospitalization, cytomegalovirus (CMV) infection, pMS, MES, and baseline CRP level tended to be higher in the TAC group (Table 1). The rate of steroid-dependent patients with prior treatment consisting of thiopurine was higher in the anti-TNF group, whereas more patients with steroid resistance were found in the TAC group (Table 1).
Detailed characteristics of the 71 patients who were treated with anti-TNF agents are further shown separately in Table 2. Of these 71 patients, 30 and 41 were treated by IFX and ADA, respectively. No significant differences in the sex ratio, age, disease duration, disease extension, prior treatment with thiopurine, CMV infection, or mean serum CRP level were observed between the IFX and ADA groups. Although most of the patients in the IFX group were hospitalized (96.7%), mostly to monitor infusion reaction, only 61% were hospitalized in the ADA group. Additionally, both the pMS and MES tended to be higher in the IFX than in the ADA group.
Clinical efficacy at 8 weeks
The clinical response rates at 8 weeks after treatment were 74.0% (111/150) in total, and 73.2% (52/71) and 74.7% (59/79) in the anti-TNF and TAC groups, respectively. The clinical remission rates at 8 weeks after the start of treatment were also comparable (28.7% in total, 31.0% and 26.6% in the anti-TNF and TAC groups, respectively). No differences in response rate or remission rate were observed, by Fisher’s exact test, between the TAC and anti-TNF groups.
Changes in the pMS and MES and the CRP level during the 8 week-treatment period are presented in Fig. 2. The corresponding pMS, MES, and CRP level at baseline and 8 weeks after the start of therapy decreased in both the TAC and TNF groups.
Changes in partial Mayo Score (pMS) (A), C-reactive protein(CRP) (B), Mayo Endoscopic Score (MES) (C) during the 8-week treatment period in the tacrolimus (TAC) and anti-TNF groups. Mean ± standard error values are presented. Statistical differences between baseline versus week 8 are shown: (A) p < 0.0001, TAC; p < 0.0001, Anti-TNF. (B) p < 0.0001, TAC; p = 0.0003, Anti-TNF. (C) p < 0.0001, TAC; p < 0.0001, Anti-TNF.
Subsequently, the anti-TNF group was analysed separately. The clinical response rates at 8 weeks after treatment were 76.7% (23/30) and 70.7% (29/41) in the IFX and ADA groups, respectively. Remission rates were 13/30 (43.3%) and 9/41 (22.0%) in the IFX and ADA groups, respectively. No differences in response rate or remission rate were observed, by Fisher’s exact test, between the IFX and ADA groups.
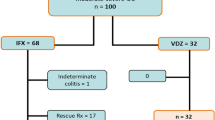
The pMS, CRP, and EMS improved significantly at 8 weeks after initiation of the treatments in both the IFX and ADA groups (Fig. 3A-C).
Changes in partial Mayo Score (pMS) (A), C-reactive protein (CRP) (B), Mayo Endoscopic Score (MES) (C) during the 8-week treatment period in the infliximab (IFX) and adalimumab (ADA) groups. Mean ± standard error values are presented. Statistical differences between baseline versus week 8 are shown: (A) p < 0.0001, IFX; p < 0.0001, ADA (B) p = 0.0011, IFX group; p < 0.0001, ADA Group. (C) p = 0.0313, IFX group; p = 0.0103, ADA Group.
Among the total cases, multivariate logistic regression analysis revealed that the male sex was more likely to respond to the treatment (OR 2.397, 95% CI 1.009–5.690, p = 0.0476) (Table 3). Use of azathioprine and 6-mercaptopurine (AZA/6MP) tended to increase the odds for response, although not reaching statistical difference (p = 0.053). Subsequently, factors affecting clinical response were separately investigated, by logistic regression analysis, in the TAC and anti‐TNF groups. In the TAC group, high CRP increased the odds of treatment response (OR: 1.548, 95% CI: 1.031–2.234, p = 0.0351). In contrast, the serum CRP before treatment did not have a significant impact on the patients’ response to treatment in the anti-TNF group. Within the anti-TNF group overall, selection of IFX or ADA did not affect the odds of response in 8 weeks. The male sex increased the odds of effectiveness only in the TNF group (OR 4.455, 95% CI 1.099–18.107, p = 0.0368).
Other factors including age, hospitalization, and Mayo score at the beginning of the treatment did not seem to significantly contribute to the outcomes of short-term response to either drugs in the logistic regression analysis (Table 3).
Long-term outcomes
Long-term outcomes of overall therapy in the multivariate Cox regression models are shown in Table 4. Analysis of overall cases indicated that the use of TAC rather than anti-TNF therapy was an independent risk factor for relapse (HR 4.284, 95% CI 2.143–8.564 p < 0.0001). A higher Mayo score at 8 weeks after treatment initiation also significantly increased the risk for relapse in all cases (HR 1.305, 95% CI 1.062–1.603). Other factors such as age, sex, use of AZA/6MP, and steroid resistance were not significantly associated with clinical relapse. Figure 4A demonstrates the relapse free-survival period in the TNF versus TAC groups.
Factors affecting clinical response were then investigated separately in the TAC and anti‐TNF groups. However, there were no significant factors that influenced the long-term outcomes in multivariate analysis, suggesting similar drug persistence on both drug choices. The relapse free survival period in the IFX versus ADA groups is shown in Fig. 4B.
Adverse effects
No deaths occurred during the study period. In the IFX group, IFX was withdrawn in five patients (17%), including three females with infusion reaction, a male with seroconversion of the interferon-gamma release assay (a marker for tuberculosis), and another male with pneumocystis pneumonia. On the other hand, ADA was withdrawn in one female patient (2%) who experienced skin eruption. In the TAC group, TAC was withdrawn in three patients (4%), including two cases with leukocytopenia (one female and one male) and one male with renal dysfunction.
Discussion
This observational study, to our knowledge, is the largest case series to date comparing the efficacy of anti-TNF agents and TAC in steroid-refractory UC patients in routine clinical practice involving multiple facilities. The features of the present study are the focus on anti-TNF agent–naïve and TAC-naïve steroid-refractory UC patients and the fact that more than half of the participants treated with TNF agents were treated with ADA.
Both TAC and anti-TNF agents yielded sufficient response rates at 8 weeks: our logistic regression analysis showed that the selection of either treatment did not statistically influence the response. This is in line with the observations of Yamamoto et al.21, where most patients treated with anti-TNF agents were treated with IFX. In fact, the baseline clinical condition of UC in our study was worse in the TAC compared to the TNF group. These tendencies are observed in other studies as well: it has been demonstrated that physicians tended to select TAC, because of its highly immunosuppressive effect, for use in patients with severe UC22,25. Additionally, lower clinical activity has been shown to be associated with better response to anti-TNF agents, but not in patients treated with TAC21. Indeed, in our study, higher CRP increased the odds of response within the TAC group, suggesting that in severe steroid-refractory UC, TAC may be an optimal choice for inducing remission.
The current study also showed that the overall OR of treatment effectiveness at 8 weeks was significantly higher in male than in female patients. The odds became higher when the data was analysed within the anti-TNF group, whereas this trend was not observed in the TAC group. The impact of sex in response to TNF inhibitors in UC has been reported previously. For instance, significantly lower response rates to treatment with TNF inhibitors are known in not only inflammatory bowel diseases, but also in ankylosing spondylitis28. This may be due to a higher rate of production of the anti-TNF antibody, which decreases the blood concentration of the agent, lowering the effect in females29. In addition, more females than males have been reported to discontinue ADA due to adverse events, especially skin reactions30. In fact, only female patients experienced an infusion reaction and skin eruption in this study. Our study and others show that attention is required for a potentially lower response and more adverse events in females undergoing anti-TNF agent treatment. Considering the data for the IFX and ADA subgroups, we did not see any differences in overall efficiency in 8 weeks. Mizoshita et al.31 showed that the efficacy of ADA in remission induction was also equivalent to that of IFX in UC patients who had not previously used anti-TNF agents. Contrarily, a recent indirect comparison meta-analysis32 and network meta-analysis33,34 showed that IFX is superior to ADA in the induction of remission in UC patients. Although further study is required, our data suggest that steroid-refractory UC in anti-TNF agent naïve cases responds well to both agents, and drug choice can be made considering the patient’s condition. Our Cox hazard model showed that the use of TAC increased the odds of relapse compared to the anti-TNF therapy. Based on the 3 month-prescription rule of TAC in Japan, in most of the studies with long-term outcomes of TAC, TAC would have been switched to thiopurine at 3 months22,24,26. In contrast, anti-TNF therapy could go on while the treatment is effective without adverse side effects. Under these conditions, it is understandable that anti-TNF therapy is better than TAC treatment for attaining remission. Although some patients maintain long-term remission after introducing TAC, other treatment options should be prepared when patients show signs of relapse. Optimal alternative treatments would include anti-TNF agents, ustekinumab, vedolizumab, and tofacitiniby35,36. This study has several limitations. First, it included unselected patients with heterogeneous baseline characteristics in a real practice setting, which was adjusted by multivariable analysis. Head-to- head comparison in a large population with long-term TAC administration in a prospective manner is needed. Second, we did not evaluate the trough level of either IFX or ADA nor the faecal calprotectin levels: monitoring of these was not approved in Japan during the research period.
In conclusion, our results indicated that TAC and anti-TNF agents exert similar satisfactory short-term effects. However, anti-TNF agents yielded better long-term outcomes than TAC in the treatment of TAC- and anti-TNF agent–naïve steroid-refractory UC patients.
Data availability
All data generated or analysed in this study are included in this published article.
References
Cosnes, J., Gower-Rousseau, C., Seksik, P. & Cortot, A. Epidemiology and natural history of inflammatory bowel diseases. Gastroenterology 140, 1785–1794. https://doi.org/10.1053/j.gastro.2011.01.055 (2011).
Danese, S. & Fiocchi, C. Ulcerative colitis. N Engl J Med 365, 1713–1725. https://doi.org/10.1056/NEJMra1102942 (2011).
Faubion, W. A. Jr., Loftus, E. V. Jr., Harmsen, W. S., Zinsmeister, A. R. & Sandborn, W. J. The natural history of corticosteroid therapy for inflammatory bowel disease: a population-based study. Gastroenterology 121, 255–260 (2001).
Turner, D., Walsh, C. M., Steinhart, A. H. & Griffiths, A. M. Response to corticosteroids in severe ulcerative colitis: a systematic review of the literature and a meta-regression. Clin. Gastroenterol. Hepatol. 5, 103–110. https://doi.org/10.1016/j.cgh.2006.09.033 (2007).
Khan, N., Abbas, A., Williamson, A. & Balart, L. Prevalence of corticosteroids use and disease course after initial steroid exposure in ulcerative colitis. Dig. Dis. Sci. 58, 2963–2969. https://doi.org/10.1007/s10620-013-2748-0 (2013).
Rutgeerts, P. et al. Infliximab for induction and maintenance therapy for ulcerative colitis. N. Engl. J. Med. 353, 2462–2476. https://doi.org/10.1056/NEJMoa050516 (2005).
Reinisch, W. et al. Long-term infliximab maintenance therapy for ulcerative colitis: the act-1 and -2 extension studies. Inflamm. Bowel. Dis. 18, 201–211. https://doi.org/10.1002/ibd.21697 (2012).
Reinisch, W. et al. Adalimumab for induction of clinical remission in moderately to severely active ulcerative colitis: results of a randomised controlled trial. Gut 60, 780–787. https://doi.org/10.1136/gut.2010.221127 (2011).
Sandborn, W. J. et al. Adalimumab induces and maintains clinical remission in patients with moderate-to-severe ulcerative colitis. Gastroenterology 142(257–265), e251-253. https://doi.org/10.1053/j.gastro.2011.10.032 (2012).
Colombel, J. F. et al. Four-year maintenance treatment with adalimumab in patients with moderately to severely active ulcerative colitis: data from ultra 1, 2, and 3. Am. J. Gastroenterol. 109, 1771–1780. https://doi.org/10.1038/ajg.2014.242 (2014).
Adedokun, O. J. et al. Pharmacokinetics and exposure-response relationship of golimumab in patients with moderately-to-severely active ulcerative colitis: results from phase 2/3 pursuit induction and maintenance studies. J. Crohns Colitis 11, 35–46. https://doi.org/10.1093/ecco-jcc/jjw133 (2017).
Hibi, T., Imai, Y., Senoo, A., Ohta, K. & Ukyo, Y. Efficacy and safety of golimumab 52-week maintenance therapy in Japanese patients with moderate to severely active ulcerative colitis: A phase 3, double-blind, randomized, placebo-controlled study-(Pursuit-J Study). J. Gastroenterol. 52, 1101–1111. https://doi.org/10.1007/s00535-017-1326-1 (2017).
Kino, T. et al. Fk-506, a novel immunosuppressant isolated from a streptomyces. II. Immunosuppressive effect of Fk-506 in vitro. J. Antibiot. (Tokyo) 40, 1256–1265 (1987).
Komaki, Y., Komaki, F., Ido, A. & Sakuraba, A. Efficacy and safety of tacrolimus therapy for active ulcerative colitis: A systematic review and meta-analysis. J. Crohns Colitis 10, 484–494. https://doi.org/10.1093/ecco-jcc/jjv221 (2016).
Damiao, A. et al. Conventional therapy for moderate to severe inflammatory bowel disease: A systematic literature review. World J. Gastroenterol. 25, 1142–1157. https://doi.org/10.3748/wjg.v25.i9.1142 (2019).
Iborra, M. et al. Effectiveness of adalimumab for the treatment of ulcerative colitis in clinical practice: Comparison between anti-tumour necrosis factor-naive and non-naive patients. J. Gastroenterol. 52, 788–799. https://doi.org/10.1007/s00535-016-1274-1 (2017).
Rodriguez-Lago, I. et al. Previous exposure to biologics and C-reactive protein are associated with the response to tacrolimus in inflammatory bowel disease. Rev. Esp. Enferm. Dig. 108, 550–557. https://doi.org/10.17235/reed.2016.4447/2016 (2016).
Ogata, H. et al. A randomised dose finding study of oral tacrolimus (Fk506) therapy in refractory ulcerative colitis. Gut 55, 1255–1262. https://doi.org/10.1136/gut.2005.081794 (2006).
Ogata, H. et al. Double-blind, placebo-controlled trial of oral tacrolimus (Fk506) in the management of hospitalized patients with steroid-refractory ulcerative colitis. Inflamm. Bowel Dis. 18, 803–808. https://doi.org/10.1002/ibd.21853 (2012).
Minami, N. et al. Tacrolimus or infliximab for severe ulcerative colitis: Short-term and long-term data from a retrospective observational study. BMJ Open Gastroenterol. 2, e000021. https://doi.org/10.1136/bmjgast-2014-000021 (2015).
Yamamoto, T., Shimoyama, T., Umegae, S., Matsumoto, K., & Tacrolimus, V.S. Anti-tumour necrosis factor agents for moderately to severely active ulcerative colitis: A retrospective observational study. Aliment Pharmacol. Ther. 43(705–716), 2016. https://doi.org/10.1111/apt.13531 (2016).
Endo, K. et al. A comparison of short- and long-term therapeutic outcomes of infliximab-versus tacrolimus-based strategies for steroid-refractory ulcerative colitis. Gastroenterol. Res. Pract. 2016, 3162595. https://doi.org/10.1155/2016/3162595 (2016).
Nuki, Y. et al. Comparison of the therapeutic efficacy and safety between tacrolimus and infliximab for moderate-to-severe ulcerative colitis: A single center experience. Scand. J. Gastroenterol. 51, 700–705. https://doi.org/10.3109/00365521.2016.1138239 (2016).
Matsumoto, S. et al. Tacrolimus versus anti-tumor necrosis factor agents for steroid-refractory active ulcerative colitis based on the severity of endoscopic findings: A single-center, open-label cohort study. Clin. Exp. Gastroenterol 10, 249–258. https://doi.org/10.2147/CEG.S143224 (2017).
Yamagami, H. et al. A comparison of short-term therapeutic efficacy between infliximab and tacrolimus for moderate to severe ulcerative colitis. Rom. J. Intern. Med. 55, 151–157. https://doi.org/10.1515/rjim-2017-0012 (2017).
Otsuka, T. et al. Short-term and long-term outcomes of infliximab and tacrolimus treatment for moderate to severe ulcerative colitis: Retrospective observational study. Kobe J. Med. Sci. 64, E140–E148 (2018).
Matsuoka, K. et al. Evidence-based clinical practice guidelines for inflammatory bowel disease. J. Gastroenterol. 53, 305–353. https://doi.org/10.1007/s00535-018-1439-1 (2018).
Rusman, T., van Vollenhoven, R. F. & van der Horst-Bruinsma, I. E. Gender differences in axial spondyloarthritis: Women are not so lucky. Curr. Rheumatol. Rep. 20, 35. https://doi.org/10.1007/s11926-018-0744-2 (2018).
Hambardzumyan, K. et al. Association of female sex and positive rheumatoid factor with low serum infliximab and anti-drug antibodies, related to treatment failure in early rheumatoid arthritis: Results from the SWEFOT trial population. Scand. J. Rheumatol. 48, 362–366. https://doi.org/10.1080/03009742.2019.1602670 (2019).
Tanaka, H. et al. Long-term retention of adalimumab treatment and associated prognostic factors for 1189 patients with Crohn’s disease. J. Gastroenterol. Hepatol. 33, 1031–1038. https://doi.org/10.1111/jgh.14034 (2018).
Mizoshita, T. et al. Prospective comparison of preference and efficacy of adalimumab and infliximab for treating ulcerative colitis naive to antitumor necrosis factor therapy. Medicine (Baltimore) 96, 7800. https://doi.org/10.1097/MD.0000000000007800 (2017).
Thorlund, K., Druyts, E., Mills, E. J., Fedorak, R. N. & Marshall, J. K. Adalimumab versus infliximab for the treatment of moderate to severe ulcerative colitis in adult patients naive to anti-TNF therapy: An indirect treatment comparison meta-analysis. J. Crohns Colitis 8, 571–581. https://doi.org/10.1016/j.crohns.2014.01.010 (2014).
Thorlund, K., Druyts, E., Toor, K. & Mills, E. J. Comparative efficacy of golimumab, infliximab, and adalimumab for moderately to severely active ulcerative colitis: A network meta-analysis accounting for differences in trial designs. Expert Rev. Gastroenterol. Hepatol. 9, 693–700. https://doi.org/10.1586/17474124.2015.1024657 (2015).
Vickers, A. D. et al. Systematic review with network meta-analysis: Comparative efficacy of biologics in the treatment of moderately to severely active ulcerative colitis. PLoS ONE 11, e0165435. https://doi.org/10.1371/journal.pone.0165435 (2016).
Barre, A., Colombel, J. F. & Ungaro, R. Review article: Predictors of response to vedolizumab and ustekinumab in inflammatory bowel disease. Aliment Pharmacol. Ther. 47, 896–905. https://doi.org/10.1111/apt.14550 (2018).
Verstockt, B., Ferrante, M., Vermeire, S. & Van Assche, G. New treatment options for inflammatory bowel diseases. J. Gastroenterol. 53, 585–590. https://doi.org/10.1007/s00535-018-1449-z (2018).
Author information
Authors and Affiliations
Contributions
MK, FT, and YA participated in the study design, data collection, data analysis, and drafting and editing of the manuscript. HK did the statistical analysis. DY, SH, TM, HO, MI, YN, MT, KH, KM, YA, NY collected patients’ data. KN finalized the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Kitayama, M., Akazawa, Y., Yoshikawa, D. et al. Comparative efficacy of antitumor necrosis factor agents and tacrolimus in naïve steroid-refractory ulcerative colitis patients. Sci Rep 10, 12546 (2020). https://doi.org/10.1038/s41598-020-68828-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-020-68828-z
This article is cited by
-
Relapse rates after withdrawal versus maintaining biologic therapy in IBD patients with prolonged remission
Clinical and Experimental Medicine (2023)
-
Clinical outcome of ulcerative colitis with severe onset in children: a multicenter prospective cohort study
Journal of Gastroenterology (2023)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.