Abstract
This study aimed to analyze the characteristics of the non-specific uptake (NSU) of 18F-labeled fibroblast activation protein inhibitor (18F-FAPI) of the pancreas and investigate the related factors. Totally, 78 patients who underwent both 18F-fluorodeoxyglucose (FDG) and 18F-FAPI PET/CT examinations were divided into normal (n = 53) and NSU (n = 25) groups. The differences in general information, medical history, laboratory indexes and uptake were compared. Receiver operating characteristic (ROC) curves were used to analyze the optimal cut-off values. The correlations between 18F-FAPI-SUVmax and blood cell analysis, liver function indexes, tumor markers, and inflammatory indices were analyzed. The logistic regression model was used to estimate the independent factors. Both 18F-FAPI (4.48 ± 0.98 vs. 2.01 ± 0.53, t = 11.718, P < 0.05) and 18F-FDG (2.23 ± 0.42 vs. 2.02 ± 0.44, t = 2.036, P = 0.045) showed significantly higher in NSU group. Patients in the NSU group tended to be complicated with a history of drinking (P = 0.034), chronic liver diseases (P = 0.006), and surgery of gastrectomy (P = 0.004). ROC analysis showed cutoff values of 3.25 and 2.05 for 18F-FAPI and 18F-FDG in identifying the NSU. Patients in the NSU group showed less platelet count, higher platelet volume, higher total bilirubin, direct or indirect bilirubin (P < 0.05). Platelet count, platelet crit, large platelet ratio, aspartate aminotransferase (AST), α-l-fucosidase, and total, direct or indirect bilirubin were correlated with 18F-FAPI-SUVmax (P < 0.05). AST [1.099 (1.014, 1.192), P = 0.021] and total bilirubin [1.137 (1.035, 1.249), P = 0.007] were two independent factors in the step forward logistic regression, and platelet/% [1.079 (1.004, 1.160), P = 0.039] and total bilirubin [1.459 (1.016, 2.095), P = 0.041] were two independent factors in the step backward logistic regression for the prediction of pancreatic uptake of 18F-FAPI. 18F-FAPI-PET/CT was better than 18F-FDG in predicting the pancreatic NSU, and NSU is related to a history of drinking, chronic liver diseases, gastrectomy, heteromorphic platelet, and impaired liver function.
Similar content being viewed by others
Introduction
Fibroblast activation protein (FAP), a type II transmembrane glycoprotein, is an antigenic molecule on the surface of cancer-associated fibroblasts (CAFs)1,2. FAP is often highly expressed in tumors of epithelial origin3, and FAP inhibitors (FAPIs) are small molecule compounds synthesized based on the structure of quinoline, which can bind specifically to FAP on the surface of CAFs. Thus, FAPI positron emission tomography/computed tomography (PET/CT) is commonly used in the clinical imaging of malignancies. Besides, FAP can also be found during the remodeling of the extracellular matrix, such as chronic inflammation, arthritis, fibrosis, and ischemic heart tissue after a myocardial infarction4. Thus, non-oncological FAPI uptake can be seen in liver fibrosis, cirrhosis, arthritis, cardiovascular disease, IgG4-related disease, and benign tumors5.
The pancreas, a vital digestive organ, is surrounded by a fibrous capsule from which connective tissue septa extend into the gland. FAPI is highly expressed in pancreatic cancers due to the abundant extracellular matrix and stromal cells, including CAFs. Although mesenchyme accounts for approximately 15–25% of total pancreas volume6, FAPI uptake was low in the normal tissues of the pancreas due to the inactivated mesenchyme fibroblast, with a maximum standardized uptake value (SUVmax) of 1.04–3.0, even lower than the FDG uptake7,8,9.
Except for the oncological uptake, FAPI accumulation has also been confirmed in acute pancreatitis (average SUVmax: 7.5 ± 3.5, n = 8)10 and IgG4-related pancreatitis (average SUVmax: 15.2 ± 9.0, n = 19)11. Zhang12 has reported 7 cases of focally elevated uptake of 68Ga-FAPI-04 in the pancreas, and lesions were identified, including pancreatic pseudocysts, sites of prior pancreatitis, and IgG 4-related disease. However, in our clinical observation, we noticed that some cases without pancreatic cancer and acute or IgG4-related pancreatitis also showed an accumulation of 18F-FAPI in the pancreas. Rare studies have mentioned this non-specific uptake (NSU) of FAPI in the pancreas. Thus, this study aimed to analyze the characteristics of the NSU of 18F-FAPI of the pancreas and investigate the potential independent factors.
Materials and Methods
Materials
This was a post-hoc analysis of a single-center, ongoing prospective clinical trial conducted at the First Affiliated Hospital of Xi’an Jiaotong University (approval number: XJTU1AF-CRF-2022-021). The study protocol was approved by the Ethics Committee of Xi’an Jiaotong University (XJTU1AF2022LSL-021). This study was registered at ClinicalTrials Gov (number NCT05788874). All participants signed an informed consent form following the national regulations of the Declaration of Helsinki and Good Clinical Practice.
This retrospective study included 86 patients who underwent both 18F-FDG and 18F-FAPI PET/CT examinations at an interval of 1–43 days. One patient with a history of pancreatic resection was excluded, and all patients were followed up for the final diagnosis. 4 cases of autoimmune pancreatitis (AIP) and 3 cases of pancreatic cancer (PC) confirmed by imaging manifestations, or histopathological evidence, were excluded. None of the women included in this study were pregnant. The study flow is displayed in Fig. 1.
Methods
PET/CT image acquisition
Preparation of 18F-FDG and 18F-FAPI-04
18F-FDG and 18F-FAPI-04 were synthesized using a GE MINItrace cyclotron and Tracerlab FX-FN multifunctional synthesizer. The synthetic precursor kits, FDG and FAPI, were purchased from ABX (Germany) and Jiangyuan (China). The radio-chemical purity of the synthesized drugs exceeded 95%. Further physical and biological quality controls were performed in compliance with current pharmacopeias.
PET/CT imaging
All patients underwent PET/CT on the same scanner (Gemini TF PET/CT, Philips, Netherlands). For 18F-FDG PET/CT scans, the patients fasted for ≥ 6 h, and the blood glucose levels were ≤ 12 mmol/L before the injection (370 MBq/kg). There was no special preparation for patients on the day of 18F-FAPI PET/CT scanning, and 18F-FAPI PET/CT scan was initiated 60 min after injection (370 MBq/kg).
Images encompassing the head to the mid-thigh were obtained for both scans. PET scans (1.5 min/bed position, 6–10 bed/per person) were acquired with an interval of 68.5 ± 12.1 min (range, 47 ~ 90 min) in three-dimensional mode after the injection. CT scans were performed (tube voltage 120 kV, tube current 50–100 mAs, layer thickness, 5 mm; 512 × 512 matrix) for attenuation correction and anatomical reference. The images were then reconstructed using an iterative method and time of flight, and the image data were transferred to an Extended Brilliance Workstation for image interpretation.
PET/CT image evaluation
The 18F-FDG and 18F-FAPI PET/CT images were interpreted by two > 10 years of experienced PET/CT physicians (Y.L.) and (C.S.), and a consensus was performed. Any disagreements were resolved by a more experienced PET/CT physician. The NSU group was defined as the increased radioactivity uptake of FAPI in the pancreas compared to the background, without confirming pancreatic cancer, acute or IgG4-related pancreatitis by other imaging methods, serology, or pathological results (if available).
For the normal group, the criteria were: (1) without 18F-FAPI uptake compared with the background; (2) without elevated serum tumor biomarkers or pancreatitis biomarkers; (3) without a history of pancreatic disease; or (4) without pancreatic-related symptoms or body signs.
The same nuclear medicine physician (C.S.) measured the pancreas' SUVmax values using circular regions of interest (ROI) placed on axial slices. The CT image features of NSU patients, including pancreatic swelling, calcification, and irregular dilatation of the pancreatic ducts, were also evaluated.
Clinical indexes
General clinical indices, including sex (male/female), age (years), primary diagnosis (specific name), height (cm), weight (kg), and BMI (kg*m−2), were recorded. The medical history, including smoking (no/yes), drinking (no/yes), hypertension (no/yes), diabetes (no/yes), chronic liver diseases (no/yes), active tumor (no/yes), chemotherapy (no/yes), gastrectomy (no/yes), intestine enterectomy (no/yes) and intrahepatic metastasis (no/yes) were recorded.
Laboratory test indexes
Laboratory tests at an interval of 3 days with the 18F-FAPI-PET/CT scan were recorded (if available), including the following parameters:
Blood cell indicators: red blood cell count (1012*L−1), hemoglobin (g*L−1), hematocrit (%), mean erythrocyte volume (fL), average hemoglobin (pg), average hemoglobin concentration (g*L−1), erythrocyte width-CV (%), erythrocyte width SD (fL), platelet count (109*L−1), platelet distribution width (fL), mean platelet volume (fL), large platelet ratio (%), platelet accumulation (%), white blood cell count (109*L−1), lymphocyte count (109*L−1), monocyte count (109*L−1), neutrophil count (109*L−1), eosinophilic cell count (109*L−1), basophilic cell count (109*L−1).
Liver function indicators: aspartate aminotransferase (AST) (U*L−1), alanine transaminase (ALT) (U*L−1), AST/ALT, alkaline phosphatase (U*L−1), γ-glutamyl transpeptidase (U*L−1), total bilirubin (TBIL) (μmol*L−1), direct bilirubin (DBIL) (μmol*L−1), indirect bilirubin (IDBIL) (μmol*L−1), total protein (g*L−1), albumin (g*L−1), globulin (g*L−1), albumin-globulin ratio (%), total bile acids (μmol*L−1), blood glucose (mmol*L−1), and α-L-fucosidase (U*L−1).
Tumor markers: squamous cell carcinoma (SCC) (ng*mL−1), carcinoembryonic antigen (CEA) (ng*mL−1), alpha-fetoprotein (AFP) (ng*mL−1), carbohydrate antigen 125 (CA-125) (U*mL−1), CA-199 (U*mL−1), CA-724 (U*mL−1), cytokeratin fragment 19 (CYFRA-19) (ng*mL−1), and neuron-specific enolase (NSE) (ng*mL−1).
Inflammatory indices: C-reactive protein (CRP) (mg*L−1), interleukin 6 (IL-6) (pg*mL−1), IL-10 (pg*mL−1), IL-17 (pg*mL−1).
Statistical analysis
IBM SPSS Statistics for Windows, version 25.0 (IBM Corp., Armonk, NY, USA) was used for the statistical analyses. Continuous variables with normal distribution and variance uniformity were represented as means ± standard deviation and analyzed by independent-sample t-tests, and continuous variables without normal distribution were expressed as median [25%, 75%] and were tested using the Mann–Whitney U test. Categorical variables were defined as several cases and analyzed by χ2 or Fisher exact tests. Kappa test was used for consistency evaluation between the two readers.
Receiver operating characteristic (ROC) curves were used to analyze the optimal cut-off value of SUVmax for predicting NSU of the pancreas [determined by Youden index = sensitivity + specificity − 1]. The DeLong test was used to compare the performance between the 18F-FAPI and 18F-FDG using Medcalc (v22.009, MedCalc Software Ltd, Belgium).
The correlations between FAPI-SUVmax and blood cell analyzed indicators, liver function indicators, tumor markers, and inflammatory indices were analyzed by Pearson correlation (only continuous variables with normal distribution and variance uniformity) or Spearman correlation. The logistic regression model was used to estimate the factors related to pancreatic NSU. Statistical significance was set at P < 0.05.
Results
Clinical characteristics
Seventy-eight patients (45 males, 33 females) were analyzed with a median age of 60 years old (25% ~ 75%, 52 ~ 68 years old). The primary malignancy or the primary diagnosis was shown in Supplementary Table 1.
Among the 78 patients included, 25 (32.05%) showed NSU in the pancreas with a pattern of diffused uptake. For the 25 cases in the NSU group, the agreement rate of the two readers was 84.00% (21/25), and 4 cases (with the SUVmax of 2.57, 3.33, 3.41 and 3.41, respectively) were judged by the 3rd reader. For the 53 cases in the normal group, the agreement rate of the two readers was 98.11% (52/53), and 1 cases (with the SUVmax of 3.17) were judged by the 3rd reader. The Kappa of the two readers was 0.848 (P < 0.001). None of the patients in the NSU patients showed pancreatic swelling and calcification, and only one patient (4%) showed irregular dilatation of the pancreatic ducts. The tracer uptake of 18F-FAPI showed significantly higher in the NSU group than in the normal group (4.48 ± 0.98 vs. 2.01 ± 0.53, t = 11.718, P < 0.001). Meantime, although with the slight difference of SUVmax, the tracer uptake of FDG also showed significantly higher in the NSU group than that of in the normal group (2.23 ± 0.42 vs. 2.02 ± 0.44, t = 2.036, P = 0.045), see as Table 1.
The tracer uptake in the normal group between the 18F-FAPI and 18F-FDG showed no difference (P = 0.890), while the tracer uptake in the NSU group between 18F-FAPI and 18F-FDG showed a significant difference (P < 0.001), see as Fig. 2.
In the Chi-Square test, patients in the NSU group weretended to complicate with a history of drinking (P = 0.034), chronic liver diseases (P = 0.006), and surgery of gastrectomy (P = 0.004), see Table 1, Figs. 3 and 4.
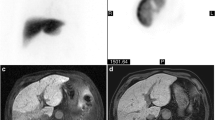
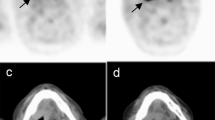
NSU in the 18F-FAPI after the surgery of gastrectomy and negative in the 18F-FDG PET/CT. A male patient, 55 years old, after surgery of gastrectomy for gastric cancer. 18F-FDG PET/CT (A) showed no FDG concentration in the pancreas, and 18F-FAPI PET/CT imaging (B) showed a high concentration of diffuse FAPI in the pancreas, with an SUVmax of 5.3. FAPI fibroblast activation protein, FDG fluorodeoxyglucose, PET/CT positron emission tomography/computed tomography. SUVmax maximum standardized uptake value.
NSU in the 18F-FAPI of the cirrhosis of the liver and negative in the 18F-FDG PET/CT. A male patient, 42 years of age, with chronic cirrhosis of the liver. 18F-FDG PET/CT (A) showed no FDG concentration in the pancreas, and 18F-FAPI PET/CT imaging (B) showed a high concentration in the pancreas, with an SUVmax of 6.3. FAPI fibroblast activation protein, FDG fluorodeoxyglucose, PET/CT positron emission tomography/computed tomography, SUVmax maximum standardized uptake value.
ROC analysis of SUVmax value of two tracers
ROC analysis showed that the cutoff value for FAPI-SUVmax to identify the NSU from normal was 3.25, with an area under the curve (AUC), sensitivity, and specificity of 0.992, 0.960, and 1.000, respectively, see Fig. 5. The cutoff value for FDG-SUVmax to identify the NSU from normal was 2.05, with an AUC an area under the curve (AUC), sensitivity, and specificity of 0.630, 0.720, and 0.509, respectively, see Table 2. The Delong test showed that the two ROC curves differed significantly (Z = 5.348, P < 0.001).
Comparisons of blood cell analysis, liver function indicators, tumor biomarkers, and inflammatory indices between two groups
Patients in the NSU group showed a lower level of platelet count (NSU vs. Normal, 182.26 ± 76.70 vs. 229.30 ± 74.17, t = 2.490, P = 0.015), higher level of mean platelet volume (NSU vs. Normal, 10.93 ± 1.34 vs. 10.26 ± 1.23, t = − 2.108, P = 0.039), and large platelet ratio (NSU vs. Normal, 32.65 ± 10.05 vs. 27.47 ± 8.40, t = − 2.298, P = 0.025) for the complete blood cells analysis, and patients in the NSU group showed a higher level of total bilirubin (NSU vs. Normal, 21.37 ± 15.84 vs. 9.55[6.62, 13.05], Z = − 3.848, P < 0.001), direct bilirubin (NSU vs. Normal, 7.41 ± 6.96 vs. 2.75(1.87, 3.90), Z = − 3.290, P = 0.001), and indirect bilirubin (NSU vs. Normal, 13.95 ± 9.67 vs. 7.97 ± 4.56, t = − 2.725, P = 0.011) in the serum, see as Table 3. The tumor biomarkers and the inflammatory indices didn’t statistically differ in the two groups (P > 0.05), see Table 4.
Correlation analysis of laboratory indicators with the SUVmax value of 18F-FAPI
In the correlation analysis, blood platelet count and platelet crit showed significantly negative correlation with SUVmax (r = − 0.296, P = 0.011; r = 0.252, P = 0.031, respectively), and large platelet ratio, TBIL, DBIL, IDBIL, AST, and α-K-fucosidase showed positive correlation with SUVmax (r ranged 0.239 ~ 0.472, all P value < 0.05), see as Fig. 6. Other correlations without statistical significance were shown in the Supplementary Table.
Logistic regression of all the factors related to pancreatic uptake of 18F-FAPI PET/CT images
In the logistic regression, AST/U*L−1 [OR (95% CI), 1.099 (1.014, 1.192), P = 0.021] and TBIL/μmol*L−1[OR (95%CI), 1.137 (1.035, 1.249), P = 0.007] were two independent factors for the pancreatic uptake of 18F-FAPI with the step forward for the selection of the factors. The ratio of large platelet/% [OR (95% CI), 1.079 (1.004, 1.160), P = 0.039] and TBIL/μmol*L−1 [OR (95% CI), 1.459 (1.016, 2.095), P = 0.041] were two independent factors for the pancreatic uptake of 18F-FAPI with the step backward for the selection of the factors, see as Table 5.
Discussion
This study tried to analyze the characteristics of the NSU uptake of 18F-FAPI in the pancreas by comparing it with the 18F-FDG head-to head. In the previous studies, non-oncological FAPI uptake was mainly explained as the pancreatic pseudocysts, sites of prior pancreatitis, and IgG 4-related disease12. However, in our clinical observations, approximately one-third of patients (25/78) without evidence of AIP and PC showed a kind of diffused NSU FAPI uptake in the pancreas, which means the fibrotic or chronic inflammatory changes of the pancreatic tissue. The difference in SUVmax in the two groups (NSU vs. normal, 4.48 ± 0.98 vs. 2.01 ± 0.53, P < 0.05) was notable and can be identified by human eyes. Meantime, the difference of SUVmax for 18F-FDG PET/CT scan in two groups (NSU vs. normal, 2.23 ± 0.42 vs. 2.02 ± 0.44, P = 0.045), although statistically significant, was slight and was challenging to identify by human eyes. In the ROC analysis, SUVmax derived from 18F-FAPI PET/CT scan showed higher AUC, sensitivity, specificity, and accuracy in differentiating the pancreatic NSU than SUVmax derived from 18F-FDG (P < 0.05), and the Delong test of two ROC curves showed statistically different (Z = 5.348, P < 0.001). These results indicated that 18F-FAPI can detect chronic or fibrotic pancreas lesions that were negative in 18F-FDG.
In our cohort, the cutoff value of the normal pancreas was 3.25 for 18F-FAPI and 2.05 for 18F-FDG. Previous studies reported 18F-FAPI-SUVmax for the normal pancreatic tissues varied from 1.04 to 3.07,9. Frederik L et al. et al. 7 conducted a head-to-head intra-individual comparison of biodistribution of 68Ga-FAPI and 18F-FDG PET/CT in cancer patients, and their results showed the pancreas uptake showed significantly lower for 68Ga-FAPI compared with 18F-FDG (1.82 vs. 1.99; P = 0.027). However, in our cohort, pancreas uptake showed no difference for 18F-FAPI compared with 18F-FDG (2.01 ± 0.53 vs 2.02 ± 0.44, P = 0.900). Cihan Gündoğan analyzed the 68Ga-FAPI-04 uptake in healthy tissues, and the pancreas showed a median SUVmax of 2.61 (minimal-maximal, 1.04 ~ 2.58)13, which is very close to our results.
In our cohort, heavy drinking, chronic liver diseases, and surgery of gastrectomy showed significant correlations with higher 18F-FAPI uptake. Previous study in a large-scale population shows that smoking, obesity, long-term drinking, diabetes, liver diseases, and long-term malnutrition are significantly associated with an increased risk of pancreatic disease14. Alcohol continues to be the an critical risk factor for chronic pancreatitis15. Therefore, alcoholism may have caused chronic pancreatitis. The surgery of gastrectomy, but not the intestine enterectomy, showed a correlation with pancreatic NSU, possibly due to the pancreatic fistula or biochemical leakage after gastrectomy16, which can lead to acute or chronic pancreatitis.
In our results, chronic liver disease, such as hepatitis or cirrhosis, but not liver metastasis, showed a correlation with pancreatic NSU. This can be explained. Hepatotropic viruses, such as hepatitis A, B, and E, were reported to affect of various extrahepatic tissues, such as the kidney, thyroid, pancreas, and bone marrow17,18. The presence of these viruses in pancreatic tissue induces fibrotic or chronic inflammatory changes resulting from the excessive deposition of the extracellular matrix, with the possibility of progression to metaplasia and subsequently, to malignant transformation19. Ying Kou also found the higher uptake of 18F-FAPI in the pancreas, with the SUVmax ± SD of (4.7 ± 1.5)20, which is very close to our results (SUVmax 18F-FAPI: 4.48 ± 0.98). However, they attributed this kind of higher uptake to physiological uptake. Whether the NSU is of clinical importance is not a done deal, 18F-FAPI may be a new way to visible the potential fibrous changes in the pancreas, which is not shown by the traditional imaging modalities.
In the laboratory test, patients in the NSU group showed a lower platelet count, higher mean platelet volume, and large platelet ratio for the complete blood cells analysis (P < 0.05), which means worse platelet morphology. Previous studies showed that the increase of atypical platelets may predict worse clinical outcomes21,22 and poor prognosis in patients with pancreatic cancer23. Also, patients in the NSU group showed higher levels of AST, total bilirubin, direct bilirubin, indirect bilirubin, and α-K-fucosidase in the serum (P < 0.05), which means impaired liver function or liver fibrosis in the patients with NSU of pancreas. In the logistic regression model, large platelet ratio, AST, and TBIL may be the independent factors for pancreatic 18F-FAPI uptake. This can be explained, as AST and the platelet are regarded as the important biomarkers in the evaluation of the liver fibrosis24,25.
To our knowledge, this is the first reported set of pancreatic NSUs for the 18F-FAPI. Whether there were NSU or not, the physician should carefully evaluate pancreatic uptake of 18F-FAPI, integrate the medical history and laboratory tests, and follow up for the final diagnosis in clinical practice.
Our study has certain limitations. The first limitation is the limited sample size. Second, there was no histo-pathological confirmation due to no clear or clinical indication of puncture for the NSU FAPI uptake. Thus, the follow-up is necessary, including the abdominal symptoms, laboratory test, or histo-pathological evidence if available.
In conclusion, we reported about 1/3 pancreatic NSU of 18F-FAPI, besides the AIP- or PC-related uptake. The NSU may be a result of a history of heavy drinking, chronic liver diseases, and surgery for gastrectomy. Patients with NSU showed lower levels of platelet count, larger platelet volume, and higher levels of AST, total bilirubin, direct bilirubin, indirect bilirubin, and α-L-fucosidase in the serum. Large platelet ratio, AST, and TBIL may be the independent factors for pancreatic 18F-FAPI uptake.
Data availability
The datasets used and/or analysed during the current study available from the corresponding author on reasonable request.
Abbreviations
- AFP:
-
Alpha-fetoprotein
- AIP:
-
Autoimmune pancreatitis
- AIP:
-
Autoimmune pancreatitis
- ALT:
-
Alanine aminotransferase
- AST:
-
Aspartate aminotransferase
- AUC:
-
Area under the curve
- BMI:
-
Body mass index
- CA:
-
Carbohydrate antigen
- CAFs:
-
Cancer-associated fibroblasts
- CEA:
-
Carcinoembryonic antigen
- CRP:
-
C reactive protein
- CV:
-
Coefficients of variation
- CYFRA 19:
-
Cytokeratin fragment 19
- DBIL:
-
Direct bilirubin
- FAP:
-
Fibroblast activation protein
- FAPI:
-
Fibroblast activation protein inhibitor
- FDG:
-
Fluorodeoxyglucose
- IDBIL:
-
Indirect bilirubin
- IL-6:
-
Interleukin 6
- NLR:
-
Neutrophil-to-lymphocyte ratio
- NSE:
-
Neuron-specific enolase
- NSU:
-
Non-specific uptake
- PC:
-
Pancreatic cancer
- PET/CT:
-
Positron emission tomography/computed tomography
- ROC:
-
Receiver operating characteristic
- ROI:
-
Region of interest
- SCC:
-
Squamous cell carcinoma
- SD:
-
Standard deviation
- SUVmax:
-
Maximum standardized uptake value
- SUVmax:
-
Maximum standardized uptake value
- TBIL:
-
Total bilirubin
References
Meyer, C. et al. Radiation dosimetry and biodistribution of (68)Ga-FAPI-46 PET imaging in cancer patients. J. Nucl. Med. 61, 1171–1177 (2020).
Sharma, P., Singh, S. S. & Gayana, S. Fibroblast activation protein inhibitor PET/CT: A promising molecular imaging tool. Clin. Nucl. Med. 46, e141–e150 (2021).
Çermik, T. F., Ergül, N., Yilmaz, B. & Mercanoglu, G. Tumor imaging with Ga-DOTA-FAPI-04 PET/CT comparison With 18F-FDG PET/CT in 22 different cancer types. Clin. Nucl. Med. 47, E333–E339 (2022).
Dendl, K. et al. FAP and FAPI-PET/CT in malignant and non-malignant diseases: A perfect symbiosis?. Cancers 13, 4946 (2021).
Mori, Y. et al. FAPI PET: Fibroblast activation protein inhibitor use in oncologic and nononcologic disease. Radiology 306, e220749 (2023).
Dolensek, J., Rupnik, M. S. & Stozer, A. Structural similarities and differences between the human and the mouse pancreas. Islets 7, e1024405 (2015).
Giesel, F. L. et al. Head-to-head intra-individual comparison of biodistribution and tumor uptake of Ga-FAPI and F-FDG PET/CT in cancer patients. Eur. J. Nucl. Med. Mol. Imaging 48, 4377–4385 (2021).
Wei, Y. et al. [(18)F]AlF-NOTA-FAPI-04: FAP-targeting specificity, biodistribution, and PET/CT imaging of various cancers. Eur. J. Nucl. Med. Mol. Imaging 49, 2761–2773 (2022).
Dendl, K. et al. Ga-FAPI-PET/CT in patients with various gynecological malignancies. Eur. J. Nucl. Med. Mol. Imaging 48, 4089–4100 (2021).
Rohrich, M. et al. Impact of Ga-68-FAPI PET/CT imaging on the therapeutic management of primary and recurrent pancreatic ductal adenocarcinomas. J. Nucl. Med. 62, 779–786 (2021).
Luo, Y. et al. Fibroblast activation protein-targeted PET/CT with (68)Ga-FAPI for imaging IgG4-related disease: Comparison to (18)F-FDG PET/CT. J. Nucl. Med. 62, 266–271 (2021).
Zhang, X., Song, W. Y., Qin, C. X., Liu, F. & Lan, X. L. Non-malignant findings of focal Ga-FAPI-04 uptake in pancreas. Eur. J. Nucl. Med. Mol. Imaging 48, 2635–2641 (2021).
Gundogan, C., Guzel, Y., Can, C., Kaplan, I. & Komek, H. FAPI-04 uptake in healthy tissues of cancer patients in (68)Ga-FAPI-04 PET/CT imaging. Contrast Media Mol. Imaging. 2021, 9750080 (2021).
Alsamarrai, A., Das, S. L., Windsor, J. A. & Petrov, M. S. Factors that affect risk for pancreatic disease in the general population: A systematic review and meta-analysis of prospective cohort studies. Clin. Gastroenterol. Hepatol. 12, 1635–1644 (2014).
Yadav, D. & Lowenfels, A. B. The epidemiology of pancreatitis and pancreatic cancer. Gastroenterology 144, 1252–1261 (2013).
Wu, J. et al. Incidence and risk factors for postoperative pancreatic fistula in 2089 patients treated by radical gastrectomy: A prospective multicenter cohort study in China. Int. J. Surg. 98, 106219 (2022).
Jiang, H., Li, Y., Sheng, Q. & Dou, X. Relationship between Hepatitis B virus infection and platelet production and dysfunction. Platelets 33, 212–218 (2022).
Fiorino, S., Cuppini, A., Castellani, G., Bacchi-Reggiani, M. L. & Jovine, E. HBV- and HCV-related infections and risk of pancreatic cancer. JOP 14, 603–609 (2013).
Ferdek, P. E. et al. When healing turns into killing: The pathophysiology of pancreatic and hepatic fibrosis. J. Physiol. 600, 2579–2612 (2022).
Kou, Y. et al. Physiological tracer distribution and benign lesion incidental uptake of Al18F-NOTA-FAPI-04 on PET/CT imaging. Nucl. Med. Commun. 43, 847–854 (2022).
Zheng, Y. Y., Wang, L. & Shi, Q. Mean platelet volume (MPV) and platelet distribution width (PDW) predict clinical outcome of acute ischemic stroke: A systematic review and meta-analysis. J. Clin. Neurosci. 101, 221–227 (2022).
Akin, H., Bilge, O., Yavuz, B., Ozkan, S. & Isik, F. The relationship between mean platelet volume and resistant hypertension. Clin. Exp. Hypertens. 44, 228–232 (2022).
Yagyu, T. et al. Decreased mean platelet volume predicts poor prognosis in patients with pancreatic cancer. BMC Surg. 21, 8 (2021).
Hagström, H., Talbäck, M., Andreasson, A., Walldius, G. & Hammar, M. Ability of non-invasive scoring systems to identify individuals in the population at risk for severe liver disease. Gastroenterology 158, 200–214 (2020).
Ginès, P. et al. Population screening for liver fibrosis: Toward early diagnosis and intervention for chronic liver diseases. Hepatology 75, 219–228 (2022).
Author information
Authors and Affiliations
Contributions
All authors contributed to the study's conception and design. Jungang Gao and Yang Li prepared the data, and Cong Shen and Yan Li collected and analyzed them. Yan Li wrote the first draft of the manuscript, and all authors reviewed the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Li, Y., Gao, J., Li, Y. et al. Non-specific uptake of 18F-FAPI-04 in the pancreas and its related factors: a post-hoc analysis of an ongoing prospective clinical trial. Sci Rep 14, 11141 (2024). https://doi.org/10.1038/s41598-024-62005-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-62005-2
Keywords
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.