Abstract
Plasma N-terminal prohormone of brain natriuretic peptide (NT-proBNP) level is primarily used as a biomarker for left ventricular (LV) dysfunction. It is influenced by various conditions, such as myocardial strain and situations affecting the clearance of NT-proBNP, including sepsis and shock. In this study, we investigated the appropriateness of NT-proBNP as a prognostic factor for septic shock. Patients with septic shock who visited the emergency department of the Ewha Womans’ University Mokdong Hospital between January 1, 2018, and December 31, 2020, were classified into the survival group (those who survived in the hospital and were discharged) and the death group (those who died in the hospital). The effectiveness of NT-proBNP, lactate, and blood urea nitrogen as predictive factors of in-hospital mortality was evaluated using the area under the receiver operating characteristic (AUROC) curve. The AUROC curve was 0.678 and 0.648 for lactate and NT-proBNP, respectively, with lactate showing the highest value. However, there was no significant difference between lactate and NT-proBNP levels in the comparison of their AUROC curve (p = 0.6278). NT-proBNP could be a useful predictor of in-hospital mortality in patients with septic shock who present to the emergency department.
Similar content being viewed by others
Introduction
Sepsis is a life-threatening organ dysfunction resulting from a dysregulated host response to infection. Septic shock is a progression of sepsis in which the underlying circulatory and cellular metabolic abnormalities are severe enough to significantly increase mortality1. Sepsis is characterized by rapid progression that can lead to multiple organ dysfunction syndrome and high mortality rates2,3,4. Sepsis continues to be the primary contributor to hospital fatalities, with mortality rates ranging from approximately 15–20%, as reported in previous clinical trials5. Notably, the mortality rate escalates to about 50% in the critically ill subset of individuals experiencing septic shock1,6,7. The medical treatment cost for patients with sepsis is increasing continuously. In the United States, the total cost of hospitalizations and skilled nursing facility admissions for Medicare A/B/C patients increased from $27.7 billion in 2012 to $41.5 billion in 20188. In South Korea, the standardized medical costs for sepsis increased by 75.5% from 2005 to 20129.
Despite numerous discussions on the diagnosis and management of sepsis, it remains challenging owing to its various etiologies and clinical presentations1,10,11,12,13,14,15,16,17,18. Sepsis exhibits evolving characteristics over time, and sepsis-induced organ dysfunction may be occult. Contrastingly, septic shock sends an immediate danger signal to clinicians owing to a rapid decrease in blood pressure, which is subsequently diagnosed through interventions such as administering vasopressors or fluid resuscitation and lactate tests1.
To date, little distinction has been made between sepsis and septic shock, and many studies have focused on biomarkers19,20. Sepsis is difficult to detect, requiring various scoring systems21 and continuous monitoring. Septic shock can be immediately recognized through the patient’s clinical status and has a higher mortality rate than sepsis. Emergency medicine doctors often encounter patients with unstable vital signs due to septic shock. Identifying predictive factors for in-hospital mortality in septic shock will ultimately help increase patient survival rates through the efficient operation of limited emergency department (ED) staff and medical resources. In patients with unstable vital signs, N-terminal prohormone of brain natriuretic peptide (NT-proBNP) levels are measured to detect left ventricular dysfunction. NT-proBNP levels can also be used as a predictor of sepsis22. In this study, we conducted an analysis to investigate the suitability of NT-proBNP as a predictive factor in patients with septic shock who present to the emergency department.
Methods
Study design and data collection
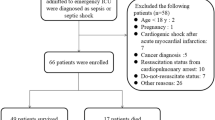
This study was a retrospective data analysis of patients visiting the ED of Ewha Womans University Mokdong Hospital between January 1, 2018 and December 31, 2020. The number of annual visits to the ED was approximately 40,000. In this study, we selected patients who received intravenous antibiotics in the ED during the study period and chose those with quick Sepsis-related Organ Failure Assessment (qSOFA, i.e., alteration in mental status, systolic blood pressure (SBP) ≤ 100 mmHg, or respiratory rate (RR) ≥ 22/min) scores ≥ 2 as patients with sepsis1,21. Seymour et al. reported that qSOFA and SOFA have similar predictive validity in the outside ICU setting, and based on its clinical utility, we adopted qSOFA as a diagnostic tool21. Among them, patients who received vasopressors to maintain mean arterial pressure > 65 mmHg after an initial fluid bolus of 20 ~ 30 ml/kg/hr were defined as the final study population for septic shock. Although lactate levels after fluid administration would also ideally be included in the diagnostic criteria, we did not include patients with serum lactate levels > 2 mmol/L (18 mg/dL) in the selection of patients with septic shock because lactate levels were measured as an initial blood test when sepsis was suspected, but this is not routinely performed after fluid administration.
Pediatric patients (aged < 18 years) were excluded from the study. Patients with out-of-hospital cardiac arrest, trauma, or non-infectious diseases were excluded, as were those for whom NT-proBNP levels in the blood were not measured. The survival and death groups were determined according to the results of discharge from the ED or hospital.
Data including age, sex, medical history, chief complaint, mental state, and vital signs were recorded immediately after the patients arrived at the ED. Blood examinations, including complete blood count, blood urea nitrogen (BUN), creatinine, C-reactive protein (CRP), procalcitonin, NT-proBNP, lactate, ketone, arterial pH, and blood culture, were performed immediately after each patient arrives at the ED. All data were recorded using an electronic medical recording system. Two board-certified emergency physicians selected and analyzed the data.
Statistical analysis
The Mann–Whitney U test was used for the analysis of continuous variables, while the chi-squared test or Fisher’s exact test was used for categorical variables, depending on appropriateness. Quantitative data are presented as medians with interquartile ranges, whereas categorical data are expressed as numbers and percentages. Statistical significance was set at a two-tailed p-value < 0.05. Analysis was conducted using the Statistical Package for the Social Science (SPSS) version 26.
To assess predictive accuracy, receiver operating characteristic (ROC) curve analysis was performed for WBC, neutrophil, BUN, creatinine, CRP, lactate, procalcitonin, NT-proBNP, and arterial pH. MedCalc statistical software version 19.4.1 was employed for the ROC curve analysis.
The method of DeLong et al.23 was used to calculate the standard error of the area under the curve (AUC) and the difference between the two AUCs. The predictive accuracy for in-hospital mortality was compared among early blood test measurements using area under the ROC curve (AUROC) and 95% confidence interval (CI).
The optimal cutoff points for each blood test were determined using the Youden Index of ROC curves. Sensitivity, specificity, positive likelihood ratio (+ LR), and negative likelihood ratio (-LR). CI was used to estimate the prognostic accuracy of each criterion for the proposed cutoff points.
Ethics statement
This study was approved by the Institutional Review Board (IRB) of the Ewha Womans University Mokdong Hospital (IRB No. 2023–04-008). All methods were carried out in accordance with relevant guidelines and regulations. The need for informed consent was waived by the IRB of Ewha Womans University Mokdong Hospital (IRB No. 2023–04-008) because of the retrospective nature of the study, and patient information was anonymized before analysis to ensure confidentiality.
Results
Patient baseline
The participants were 418 patients with septic shock (Fig. 1). During the study period, 307 patients survived and were discharged (survival group), and 111 patients died (death group) (Table 1). The median age of the survival group was 76 years old (IQR: 64.00–82.00), and that of the death group was 79 years old (IQR: 70.00–84.00, p < 0.05). The study sample comprised 241 males (57.7%) and 177 females (42.3%). In both groups, most patients with septic shock were hypertensive (143 and 50 patients, respectively), and the only significant difference between the groups was the incidence of stroke (p < 0.05). The most common symptom reported in both groups was dyspnea (survival vs. death; n = 85, 27.7% vs. n = 42, 37.8%). The second most frequently reported symptom differed between the two groups: it was fever in the survival group (n = 77, 25.1%) but altered mental status in the death group (n = 28, 25.2%, p < 0.05). At the time of arrival in the ED, the level of consciousness was predominantly alert in the survival group (n = 160, 52.1%), whereas the death group had a higher proportion of patients with pain-responsive consciousness (n = 43, 38.7%; p < 0.05).
The two groups included patients with septic shock, and their overall vital signs were as follows: SBP: 85.00 mmHg (IQR: 73–98.00), diastolic blood pressure: 51.00 mmHg (IQR: 41.50–61.00), heart rate: 105.00/min (IQR: 89.00–123.00), RR: 22.00 (IQR: 20.00–26.00), and body temperature: 37.2 °C (IQR: 36.20–38.20). There was a significant difference in body temperature between the groups (p < 0.05).
Comparison of laboratory test and management
Among the various blood tests performed (Table 2), only BUN, creatinine, CRP, procalcitonin, NT-proBNP, lactate, and arterial pH showed significant differences between the groups (p < 0.05).
Respiratory tract infection was the most common infection in both groups (survival vs. death; 58.6% vs. 71.2%), followed by genitourinary tract infection (n = 95, 30.9%) in the survival group and intra-abdominal infection (n = 23, 20.7%) in the death group. The most common antibiotics used in all patients with septic shock were meropenem (n = 119, 28.5%) and piperacillin/tazobactam (n = 107, 25.6%). The two groups predominantly used norepinephrine alone (survival vs. death; n = 260, 84.7% vs. n = 49, 44.1%), and the duration of inotrope or vasopressor use was 2.00 days (IQR: 1.00–4.00) in the survival group and 3.00 days (IQR 2.00–7.00) in the death group (p < 0.05).
Patients who received mechanical ventilation had a rate of 26.1% (n = 80) in the survival group compared with 60.4% (n = 67, p < 0.05) in the death group. Among the patients who received continuous renal replacement therapy, the survival group had a rate of 6.5% (n = 20), whereas the death group had a rate of 21.6% (n = 24, p < 0.05). The blood culture test did not detect any bacterial growth in 57.0% of the patients in the survival group and in 58.6% in the death group. The length of stay in the ED was 6.13 h (IQR: 4.75–8.68, p = 0.752) overall, and the total length of hospital stay was 14.18 days (IQR: 6.91–25.89) for the survival group and 3.24 days (IQR: 0.82–13.73, p < 0.05) for the death group.
NT-proBNP as a predictive factor
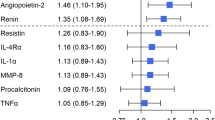
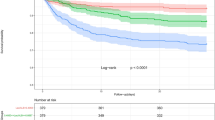
ROC curve analysis was performed for lactate, NT-proBNP, BUN, arterial pH, CRP, creatinine, and procalcitonin levels (p < 0.05; Table 3). The AUC values for predicting in-hospital mortality were as follows: Lactate, 0.678 (95% CI: 0.627–0.726); NT-proBNP, 0.648 (95% CI: 0.600–0.694); BUN, 0.630 (95% CI: 0.582–0.676), arterial pH, 0.618 (95% CI: 0.570–0.665); CRP, 0.607 (95% CI: 0.558–0.654); creatinine, 0.588 (95% CI: 0.539–0.636) and procalcitonin, 0.573 (95% CI: 0.522–0.624). ROC curves were compared using three blood tests with high AUROC values: lactate, NT-proBNP, and BUN (Fig. 2). In the comparisons between the two blood tests, lactate vs. NT-proBNP (p = 0.6278), lactate vs. BUN (p = 0.1667), and NT-proBNP vs. BUN (p = 0.3188), findings were not significantly different (Table 4).
Discussion
In this study, we investigated the utility of NT-proBNP as a biomarker for predicting in-hospital mortality in patients presenting to the emergency department with septic shock. The results revealed that NT-proBNP was a valuable predictive factor comparable to lactate, emphasizing its significance in predicting in-hospital mortality.
NT-proBNP is widely used in the ED for the diagnosis of heart failure. NT-proBNP, a metabolite of pro-BNP, is a prohormone secreted by myocardial cells24. The prohormone of brain natriuretic peptide (proBNP) is decomposed into the active metabolite brain natriuretic peptide and the inactive metabolite NT-proBNP. NT-proBNP has a longer half-life, so it remains in the bloodstream for a longer period of time25,26. Natriuretic peptides are predominantly secreted during volume overload and cardiomyocyte stretching27. Although BNP is eliminated through various pathways, NT-proBNP is cleared exclusively by the kidneys28,29,30,31,32. Research comparing BNP and NT-proBNP is ongoing; however, there is still no consensus on which peptide is superior33,34,35,36,37, and the roles of these peptides have not been thoroughly studied32,38.
Although an increased plasma NT-proBNP level is primarily used as a biomarker for left ventricular (LV) dysfunction26, it is not necessarily specific to heart failure and is influenced by various conditions that cause myocardial strain and affect the clearance of NT-proBNP, including myocardial ischemia, arrhythmia, sepsis, shock, anemia, renal failure, pulmonary embolism, asthma, acute respiratory disease syndrome, and chronic obstructive pulmonary disease32,36,39,40,41,42. NT-proBNP levels can increase in various situations, particularly in septic shock, a systemic inflammatory response accompanied by multi-organ damage, and there may be diverse interpretations as to whether the elevated levels are indicative of LV dysfunction or other diseases32,43,44,45,46,47.
Since the underlying conditions can be difficult to ascertain in the ED, predicting the mortality rate in patients with septic shock using NT-proBNP levels, regardless of the underlying diseases, would be clinically useful. This analysis did not exclude patients with preexisting heart or kidney diseases. The survival and death groups included patients with various diseases, and the only significant difference between the two groups was stroke (p < 0.05, Table 1).
In this study, lactate had an AUC of 0.678 (95% CI: 0.627–0.726), and NT-proBNP had an AUC of 0.648 (95% CI: 0.600–0.694) as predictors of mortality in patients with septic shock, and this finding is consistent with previous research results32,36,48,49,50,51,52. There was no significant difference in the ROC curves between lactate and NT-proBNP (p = 0.6278, Table 4), indicating that NT-proBNP may serve as a substitute for lactate in predicting mortality in patients with septic shock when lactate cannot be used.
NT-proBNP could be a useful predictor of in-hospital mortality in patients with septic shock who present to the emergency department.
Limitations
This study has several limitations. Owing to its single-center design, caution should be exercised when extrapolating and applying the research findings on a broader scale. Additionally, the retrospective nature of this study introduced inherent limitations, particularly in defining sepsis. In the ED, patients with suspected sepsis are routinely tested for their initial lactate levels. However, lactate levels are not monitored after adequate fluid resuscitation, which does not fulfill the definition of septic shock recommended by Sepsis-31.
Data availability
The datasets used and analyzed during the current study are available from the corresponding author on reasonable request.
References
Singer, M. et al. The third international consensus definitions for sepsis and septic shock (Sepsis-3). JAMA 315, 801–810 (2016).
Watson, R. S. et al. The epidemiology of severe sepsis in children in the United States. Am. J. Respir. Crit. Care Med. 167, 695–701 (2003).
Wheeler, D. S., Jeffries, H. E., Zimmerman, J. J., Wong, H. R. & Carcillo, J. A. Sepsis in the pediatric cardiac Intensive Care Unit. World J. Pediatr. Congenit. Heart Surg. 2, 393–399 (2011).
Zhang, Y. et al. Correlations of changes in brain natriuretic peptide (BNP) and cardiac troponin I (cTnI) with levels of C-reactive protein (CRP) and TNF-α in pediatric patients with sepsis. Med. Sci. Monit. 25, 2561–2566 (2019).
Bauer, M. et al. Mortality in sepsis and septic shock in Europe, North America and Australia between 2009 and 2019—Results from a systematic review and meta-analysis. Crit. Care 24, 239 (2020).
Pavon, A. et al. Profile of the risk of death after septic shock in the present era: An epidemiologic study. Crit. Care Med. 41, 2600–2609 (2013).
Tintinalli, J. E. et al. Tintinalli's Emergency Medicine A Comprehensive Study Guide. Ninth ed. (McGraw-Hill, 2019).
Buchman, T. G. et al. Sepsis among Medicare beneficiaries: 1. The Burdens of Sepsis, 2012–2018. Crit. Care Med. 48, 276–288 (2020).
Kim, J., Kim, K., Lee, H. & Ahn, S. Epidemiology of sepsis in Korea: A population-based study of incidence, mortality, cost and risk factors for death in sepsis. Clin. Exp. Emerg. Med. 6, 49–63 (2019).
Jentzer, J. C. et al. Management of refractory vasodilatory shock. Chest 154, 416–426 (2018).
Mahfood Haddad, T., Vallabhajosyula, S., Nawaz, M. S. & Vivekanandan, R. Fatal pneumocystis jiroveciipneumonia in a HIV-negative adult. BMJ Case Rep. (2015): p. bcr2015210117.
Mahfood Haddad, T., Vallabhajosyula, S., Sundaragiri, P. R. & Vivekanandan, R. Mycotic pseudoaneurysm by vancomycin-intermediate Staphylococcus aureus: a rare cause of persistent bacteraemia. BMJ Case Rep. 2015 (2015) (apr01 1): p. bcr2014209003-b.
Rose, S. R. et al. The utility of bronchoalveolar lavage beta-D-glucan testing for the diagnosis of invasive fungal infections. J. Infect. 69, 278–283 (2014).
Sundaragiri, P. R., Vallabhajosyula, S., Mahfood Haddad, T. & Esterbrooks, D. J. Tricuspid and mitral endocarditis due to methicillin-resistant staphylococcus aureus exhibiting vancomycin-creep phenomenon. BMJ Case Rep. (2015): p. bcr2015211974.
Vallabhajosyula, S., Varma, M. D., Vallabhajosyula, S. & Vallabhajosyula, S. Association of hyponatremia with in-hospital outcomes in infective endocarditis: A 5-year review from an Indian Intensive Care Unit. Indian J. Crit. Care Med. 20, 597–600 (2016).
Vallabhajosyula, S., Varma, M. D., Vallabhajosyula, S. & Vallabhajosyula, S. Right-sided infective endocarditis in an Indian Intensive Care Unit. J. Glob. Infect. Dis. 8, 124–125 (2016).
Varma, M. D., Vengalil, S., Vallabhajosyula, S., Krishnakumar, P. C. & Vidyasagar, S. Leptospirosis and dengue fever: a predictive model for early differentiation based on clinical and biochemical parameters. Trop. Doct. 44, 100–102 (2014).
Da Silva Ramos, F. J., De Freitas, F. G. R. & Machado, F. R. Sepsis in patients hospitalized with coronavirus disease 2019: How often and how severe? Curr. Opin. Crit. Care 27, 474–479 (2021).
Vincent, J. L. The clinical challenge of sepsis identification and monitoring. PLOS Med. 13, e1002022 (2016).
Pierrakos, C. & Vincent, J. L. Sepsis biomarkers: A review. Crit. Care 14, R15 (2010).
Seymour, C. W. et al. Assessment of clinical criteria for sepsis: for the third international consensus definitions for sepsis and septic shock (Sepsis-3). JAMA 315, 762–774 (2016).
Shojaee, M. et al. Pro, B N P versus MEDS score in determining the prognosis of sepsis patients; a diagnostic accuracy study. Emergency 6, e4 (2018).
Delong, E. R., Delong, D. M. & Clarke-Pearson, D. L. Comparing the areas under two or more correlated receiver operating characteristic curves: A nonparametric approach. Biometrics 44, 837–845 (1988).
Qian, A., Zhang, M. & Zhao, G. Dynamic detection of N-terminal pro-B-type natriuretic peptide helps to predict the outcome of patients with major trauma. Eur. J. Trauma Emerg. Surg. 41, 57–64 (2015).
Hall, C. Essential biochemistry and physiology of (NT-pro)BNP. Eur. J. Heart Fail. 6, 257–260 (2004).
McKie, P. M. & Burnett, J. C. NT-proBNP: The gold standard biomarker in heart failure. J. Am. Coll. Cardiol. 68, 2437–2439 (2016).
Vanderheyden, M., Bartunek, J. & Goethals, M. Brain and other natriuretic peptides: Molecular aspects. Eur. J. Heart Fail. 6, 261–268 (2004).
Smith, M. W., Espiner, E. A., Yandle, T. G., Charles, C. J. & Richards, A. M. Delayed metabolism of human brain natriuretic peptide reflects resistance to neutral endopeptidase. J. Endocrinol. 167, 239–246 (2000).
Mukoyama, M. et al. Brain natriuretic peptide as a novel cardiac hormone in humans. Evidence for an exquisite dual natriuretic peptide system, atrial natriuretic peptide and brain natriuretic peptide. J. Clin. Investig. 87, 1402–1412 (1991).
Valli, N., Gobinet, A. & Bordenave, L. Review of 10 years of the clinical use of brain natriuretic peptide in cardiology. J. Lab. Clin. Med. 134, 437–444 (1999).
Zakynthinos, E., Kiropoulos, T., Gourgoulianis, K. & Filippatos, G. Diagnostic and prognostic impact of brain natriuretic peptide in cardiac and noncardiac diseases. Heart Lung 37, 275–285 (2008).
Pandompatam, G., Kashani, K. & Vallabhajosyula, S. The role of natriuretic peptides in the management, outcomes and prognosis of sepsis and septic shock. Rev. Bras. Ter. Intensiva 31, 368–378 (2019).
Yeo, K. T. et al. Multicenter evaluation of the Roche NT-proBNP assay and comparison to the Biosite Triage BNP assay. Clin. Chim. Acta 338, 107–115 (2003).
Pfister, R., Scholz, M., Wielckens, K., Erdmann, E. & Schneider, C. A. Use of NT-proBNP in routine testing and comparison to BNP. Eur. J. Heart Fail. 6, 289–293 (2004).
Hill, S. A. et al. Use of BNP and NT-proBNP for the diagnosis of heart failure in the emergency department: A systematic review of the evidence. Heart Fail. Rev. 19, 421–438 (2014).
Bai, Y. L., Hu, B. L., Wen, H. C., Zhang, Y. L. & Zhu, J. J. Prognostic value of plasma brain natriuretic peptide value for patients with sepsis: A meta-analysis. J. Crit. Care 48, 145–152 (2018).
Rørth, R. et al. Comparison of BNP and NT-proBNP in patients with heart failure and reduced ejection fraction. Circ. Heart Fail. 13, e006541 (2020).
Machado, R. D. L. et al. Related prognostic factors in elderly patients with severe sepsis and septic shock. Rev. Bras. Ter. Intensiva 21, 9–17 (2009).
Vallabhajosyula, S. et al. Role of B-type natriuretic peptide in predicting in-hospital outcomes in acute exacerbation of chronic obstructive pulmonary disease with preserved left ventricular function: A 5-year retrospective analysis. J. Intensive Care Med. 33, 635–644 (2018).
Mitaka, C. et al. Increased plasma concentrations of brain natriuretic peptide in patients with acute lung injury. J. Crit. Care 12, 66–71 (1997).
Enea, I. et al. Biohumoral markers and right ventricular dysfunction in acute pulmonary embolism: The answer to thrombolytic therapy. Ital. Heart J. Suppl. 5, 29–35 (2004).
McLean, A. S. & Huang, S. J. Brain not processing: Is finding a role for BNP in sepsis like fitting a square peg into a round hole?. Crit. Care 18, 161 (2014).
Shor, R. et al. BNP in septic patients without systolic myocardial dysfunction. Eur. J. Intern. Med. 17, 536–540 (2006).
McLean, A. S. et al. Prognostic values of B-type natriuretic peptide in severe sepsis and septic shock. Crit. Care Med. 35, 1019–1026 (2007).
Papanikolaou, J. et al. New insights into the mechanisms involved in B-type natriuretic peptide elevation and its prognostic value in septic patients. Crit. Care 18, R94 (2014).
Burjonroppa, S. C. et al. Cancer patients with markedly elevated B-type natriuretic peptide may not have volume overload. Am. J. Clin. Oncol. 30, 287–293 (2007).
Vallabhajosyula, S. et al. Basic and advanced echocardiographic evaluation of myocardial dysfunction in sepsis and septic shock. Anaesth. Intensive Care 46, 13–24 (2018).
Varpula, M. et al. Predictive value of N-terminal pro-brain natriuretic peptide in severe sepsis and septic shock. Crit. Care Med. 35, 1277–1283 (2007).
Casserly, B. et al. Lactate measurements in sepsis-induced tissue hypoperfusion: Results from the Surviving Sepsis Campaign database. Crit. Care Med. 43, 567–573 (2015).
Liu, G. et al. Early actate levels for prediction of mortality in patients with sepsis or septic shock: A meta-analysis. Int. J. Clin. Exp. Med. 10, 37–47 (2017).
Jansen, T. C. et al. Early lactate-guided therapy in intensive care unit patients: A multicenter, open-label, randomized controlled trial. Am. J. Respir. Crit. Care Med. 182, 752–761 (2010).
Filho, R. R. et al. Blood lactate levels cutoff and mortality prediction in sepsis—Time for a reappraisal? A retrospective cohort study. Shock 46, 480–485 (2016).
Funding
This work was supported by an Ewha Womans University research grant in 2021. The funders played no role in the study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Author information
Authors and Affiliations
Contributions
Acquisition, analysis, and interpretation of data: J.H.L., Y.C. Drafting the manuscript for intellectual content: J.H.L., Y.C. Statistical analysis: J.H.L., Y.C. All authors reviewed, revised, and approved the manuscript for submission.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Choi, Y., Lee, J.H. Clinical usefulness of NT-proBNP as a prognostic factor for septic shock patients presenting to the emergency department. Sci Rep 14, 10999 (2024). https://doi.org/10.1038/s41598-024-61888-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-61888-5
Keywords
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.