Abstract
Hypertensive patients are at an elevated risk of developing mental diseases such as depression, which can impair their quality of life. The purpose of this study is to measure the prevalence of self-reported depression among hypertensive patients treated at primary health care facilities in Marrakech. Between May 2021 and December 2022, a cross-sectional study of 1053 hypertensive patients attending primary health care facilities in Marrakech was conducted. A face-to-face questionnaire was used to collect socio-demographic, behavioral, and clinical data, as well as hypertension treatment characteristics and the care-patient-physician triad. The Patient Health Questionnaire-9 was used to assess self-reported depression. To identify self-reported depression risk factors, multivariate logistic regression was used. Depressive symptoms were reported by 56.1% of hypertensive patients. The patients' average age was 63.2 ± 9.5 years, and 508 (85.9%) were female. Female sex, stress, a low-salt diet, pain and physical discomfort, an urban living environment, a lack of self-monitoring of hypertension, an unsatisfactory relationship with the healthcare system, a family history of hypertension, and the perception of adverse effects of the antihypertensive drug were all associated with self-reported depression. Self-reported depression is prevalent among hypertensive patients in Marrakech. The mental health component should be emphasized while addressing hypertensive patients in primary health care facilities.
Similar content being viewed by others
Introduction
High blood pressure (HBP) is a significant public health issue. In 2019, 1.28 billion individuals worldwide were afflicted with hypertension, with 82% living in low- or middle-income countries1. This number is anticipated to climb by 60% by 2025, according to epidemiological studies2,3. Every year, HBP kills 9.4 million people. It represents a considerable financial burden for nations with 57 million disability-adjusted life years (DALYs) globally, including 658,301 DALYs in Morocco4,5. The prevalence of HBP was 29.3% in the most current StepWise study on risk factors for noncommunicable diseases, which was conducted on a sample of 5429 persons aged 18 and older in Morocco in 20185,6. Morocco's Ministry of Health and Social Protection has been executing a countrywide hypertension prevention and control program since 1996. This initiative provides 45 million dirhams per year for the purchase of medications and equipment needed by primary health care facilities to guarantee hypertensive patient diagnosis and follow-up7. Primary health care facilities treated and monitored 1,250,000 hypertensive patients in 20217. Despite the fact that hypertensive individuals are more likely to suffer from mental diseases such as depression8, we manage their physical health without addressing their mental health. Depression symptoms include sadness, loss of interest or pleasure, feelings of guilt or low self-esteem, sleep or food problems, weariness, and a lack of attention9. In 2017, depression was observed in 40.1% of 411 hypertensive patients in Karachi, Pakistan. In people with HBP, depression is associated with an increased risk of stroke and myocardial infarction. A delay in diagnosis can lead to problems, a decrease in the quality of life of hypertensive patients, and even death10.
To the best of our knowledge, no epidemiological study has looked at the mental health of Moroccan hypertensives. Given the prevalence of hypertension and its influence on mental health, research into self-reported depression in hypertensives is crucial. This would provide evidence on which policymakers in the country may depend to enhance the hypertension treatment program and meet the overall health needs of hypertensive patients. As a result, the objective of our research was to determine the prevalence of self-reported depression among hypertensive patients followed at primary health care facilities in Marrakech.
Subjects and methods
Marrakech is a Moroccan city in the center of the country. El Kelaa des Sraghna borders it on the north, Al Haouz on the south, Rhamna on the east, and Chichaoua and Safi on the west. It has a population of 1,330,468 people and covers an area of 2625 km211. Its primary care facilities care for and monitor 23,213 hypertensive individuals12.
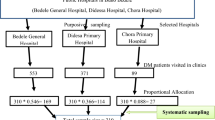
Between 2021 and 2022, a cross-sectional study was conducted on hypertensive patients aged 18 and older who were followed at primary health care facilities in Marrakech, were on pharmaceutical therapy for HBP for at least six months, and had agreed to participate in the study. Data collection was made by convenience sampling. a two-stage stratified survey was employed. Seventy percent of hypertensives resided in cities, whereas thirty percent lived in rural regions. To select the primary unit, which is the primary health care facilities, a first draw was made from the list of primary health care facilities supplied by the representative of the Ministry of Health and Social Protection of Marrakech. A second draw was made from the patients' order numbers to determine the secondary unit, which is the hypertensive patients. These order numbers were issued to patients when they arrived at primary health care facilities in order to control the flow of hypertensives during their follow-up. Pregnant women were not permitted to take part in the study.
Sample size
We determined our sample size based on a 50% estimated prevalence of self-reported depression, a 95% confidence interval, a 5% margin of error, a 20% non-response rate, and a cluster effect of two. The requisite number of patients was 922.
Data collection tool and procedure
A face-to-face questionnaire administered after a patient interview was used to collect sociodemographic and economic data, behavioral characteristics, level of knowledge about hypertension, clinical characteristics, antihypertensive treatment characteristics, and the relationship between the healthcare system, patient, and doctor. The questionnaire was given in arabic which is the main language spoken by Moroccan.
Operational definition
Self-reported depression assessment
The arabic translation version of Patient Health Questionnaire-9 (PHQ-9) was used to assess self-reported depression in hypertensive patients13. The PHQ-9 is made up of nine questions to which patients must respond: “never”, “several days”, “more than half the days” and “almost every day”. The following questions were asked: Over the last two weeks: How often do you feel little interest or pleasure in doing things? How often do you feel sad, depressed, or hopeless? How often do you find it difficult to fall or stay asleep, or sleep too much? How often do you feel tired or have low energy? How often do you have a poor perception of yourself—or do you think you are a loser or have not met your own or your family's expectations? How often do you struggle to concentrate on things like reading the newspaper or watching television? How often do you move or speak so slowly that others notice, or are you so restless that you move much more than usual? and How often have you thought you'd be better off dead, or that you'd be better off hurting yourself in some way? Each question was scored on a scale of zero to three. Zero for “never”, one for “several days”, two for “more than half the days” and three for “almost every day”. The sub-scores of the nine questions were put together to yield a total score that ranged from 0 to 27. The following is how the score was interpreted: A score of 0 to 4 indicated no or minimal symptoms; a score of 5 to 9 indicated mild symptoms; a score of 10 to 14 indicated moderate symptoms; a score of 15 to 19 indicated moderately severe symptoms; and a score of 20 to 27 indicated severe depressive symptoms. People who received a score of 5 or higher were deemed to have self-reported depression13,14.
Other variables
An electronic sphygmomanometer with an adjustable cuff (MicroLife Pro M with an accuracy of 3 mmHg) was used to measure blood pressure (BP). Blood pressure control was assessed using the criteria of the European Society of Arterial Hypertension and the European Society of Cardiology (ESH/ESC) recommendations15,16.
When patients reported receiving social support, social support was reported. When patients reported measuring their blood pressure outside of the primary health care facilities, self-monitoring was postponed. When patients claimed they had consumed tobacco or alcohol in the previous two months, it was reported. World Health Organization (WHO) criteria were used to determine overweight and obesity16,17. When patients experienced physical pain or discomfort, pain and physical discomfort were reported. When patients reported feeling limited in their mobility, restricted mobility was declared. When patients reported feeling stress, stress was declared. Patients reported a lack of autonomy when they felt a lack of autonomy.
Ethical consideration
Before beginning the survey, we made certain that it complied with the Helsinki Declaration. After informing them about the objective of the study and respecting their privacy and confidentiality, all participants provided written and informed consent. The ethical committee of Rabat's Faculty of Medicine and Pharmacy evaluated and approved the study protocol (#21/21).
Statistical analysis
All the data was imported into Excel and analyzed using Epi-info 7. Where applicable, continuous variables were presented as the mean and standard deviation. Numbers and percentages were used to express categorical variables. The Pearson chi-square test or, where applicable, Fisher's exact test was used to compare categorical variables. Where appropriate, continuous variables were compared using the ANOVA test or the Mann–Whitney test. The multiple logistic regression included all variables with a p value of less than 0.20 in the bivariate analysis. The selection of these variables was made by the manual purposeful selection method. The adjusted odds ratio (AOR) and its 95% confidence interval were used to determine the association between the risk factor and the presence of self-reported depression.
Results
Socio-demographic and economic characteristics
Table 1 summarizes the socio-demographic and economic characteristics of hypertensive patients. A total of 1053 patients were approached, with a self-reported depression prevalence of 56.1%. The patients' average age was 63.0 ± 9.9 years; 811 (77.0%) were women; 743 (70.6%) could not read or write; 962 (91.4%) were unemployed; and 728 (69.1%) had a monthly household income of less than $199.
Data on hypertension knowledge and behavioral characteristics
General knowledge on arterial hypertension was unsatisfactory in 1032 (98.0%) patients Table 2. Analysis of behavioral data showed that 284 (27.0%) were on a low-salty diet; 937 (89.0%) had stress; 746 (70.8%) had unsatisfactory physical activity; 669 (63.5%) were sedentary; 259 (24.6%) had difficulty following the low-salt diet; and 367 (34.8%) declared that they did not benefit from social support Table 2.
Clinical characteristics of hypertensive patients
Table 3 shows that 508 (48.2%) of hypertensive patients had a comorbidity; 458 (43.5%) had diabetes; 601 (57.1%) had a family history of arterial hypertension; 749 (71.1%) had uncontrolled arterial hypertension; 587 (55.8%) had pain and physical discomfort; and 843 (80.1%) were overweight or obese.
Characteristics related to treatment and the patient-doctor-healthcare system triad
Out of 1053 participants, 873 (82.9%) had a bad relationship with the healthcare system, 507 (48.1%) didn't think their doctor was willing to pay attention to their questions about their sickness, and 637 (60.5%) reported antihypertensive drugs non-availability at the primary health care facilities, 263 (25.0%) reported adverse effects of antihypertensive drugs, and 252 (23.9%) reported not buying antihypertensive drugs in case of stockout at the primary health care facilities Table 4.
Self-reported depression
Self-reported depression was expressed by 591 (56.1%) of the participants. They were 63.2 ± 9.5 years old on average, 508 (86.0%) were women, and 474 (80.2%) lived in cities Table 1. According to an analysis of behavioral and clinical data, 564 (53.6%) were stressed, 186 (31.5%) were on a reduced salt diet Table 2, 195 (42.2%) had a family history of arterial hypertension, and 406 (68.7%) were in pain or physical discomfort Table 3. In 515 (87.1%) participants, the interaction with the healthcare system was unsatisfactory Table 4.
According to the distribution of hypertensive patients by level of self-reported depression, 429 (40.7%) had mild self-reported depression, 130 (12.3%) had moderate self-reported depression, 29 (2.8%) had moderately severe self-reported depression, and 3 (0.3%) had severe self-reported depression, while 462 (43.9%) had no or minimal self-reported depression.
During the bivariate analysis, the p value was set at 0.20. As mentioned in Table 5, after bivariate analysis, these factors were associated with the presence of self-reported depression: female sex (p < 0.0001); being single compared to partnered (p < 0.0001); cannot read or write (p = 0.03); urban compared to rural (p < 0.0001); being unemployed (p = 0.01); low monthly income (p < 0.0001); high stress compared to low stress (p < 0.0001); moderate stress compared to low stress (p < 0.0001); unsatisfactory knowledge about preventive measures against HBP (p = 0.11); tobacco consumption (p = 0.0005); alcohol consumption (p = 0.10); unsatisfactory physical activity (p < 0.0001); sedentary (p = 0.0001); low-salt diet (p = 0.0002); non-consumption of five fruits and vegetables per day (p = 0.0001); lack of self-monitoring of blood pressure (p < 0.0001); lack of social support (p < 0.0001); presence of comorbidity (p < 0.0001); presence of diabetes (p < 0.0001); presence of dyslipidemia (p = 0.11); duration of hypertension greater than five years (p = 0.002); family history of arterial hypertension (p = 0.0001); uncontrolled blood pressure (p = 0.06); lack of autonomy (p = 0.0004); pain and physical discomfort (p < 0.0001); reduced mobility (p < 0.0001); overweight and obesity (p = 0.001); difficulty following a low-salty diet (p = 0.001); unsatisfactory relationship between the patient and the healthcare system (p < 0.0001); unsatisfactory doctor-patient relationship (p = 0.001); patients' perception of their doctor's lack of willingness to understand their concerns regarding their HBP (p < 0.0001); stock-out of antihypertensive drug at primary health care facilities (p < 0.0001); non-purchase by the patient of the antihypertensive drug in the event of a stock-out at the primary health care facilities (p < 0.0001); perception by the patient of having too much medicine to take (p = 0.03); perception that the drug has more adverse effects than benefits (p = 0.003) Table 5.
Multivariate analysis
After adjusting for the other variables, we identified the following factors as being associated with self-reported depression in hypertensive patients: high stress compared to low stress (Adjusted Odd Ratio of 10.5; 95% CI [5.63–19.75]); female sex (AOR of 4.1; 95% CI [2.45–6.88]); the low-salt diet (AOR of 3.1; 95% CI [1.28–7.37]); pain and physical discomfort (AOR of 2.9; 95% CI [2.08–3.99]); urban (AOR of 2.2; 95% CI [1.47–3.44]); moderate stress compared to low stress (AOR of 2.2; 95% CI [1.32–3.85]); lack of self-monitoring of arterial hypertension (AOR of 1.9; 95% CI [1.27–2.81]); unsatisfactory patient relationship with the healthcare system (AOR of 1.8; 95% CI [1.10–2.91]); family history of arterial hypertension (AOR of 1.6; 95% CI [1.16–2.22]); and perception that the drug has more adverse effects than benefits (AOR of 1.5; 95% CI [1.04–2.21]) Table 5.
Discussion
With a prevalence of 56.1%, the current study found a significant prevalence of self-reported depression. The frequency of self-reported depression ranged from 26.6 to 40.1% in countries with similar socio-demographic and economic characteristics to Morocco. Indeed, self-reported depression was 26.6% in a sample of 237 hypertensive patients in Nigeria in 201918. In Peru, the prevalence of self-reported depression was 34.9% among 10,566 participants in 201719. In Pakistan, the prevalence was 40.1% among 411 hypertensive patients in 201720. The prevalence of self-reported depression in hypertensive patients ranged from 37 to 58% in low-income nations. Between 2015 and 2016, 58.1% of 234 hypertensive patients in Andkhoy, Afghanistan, self-reported depression21. In Ethiopia, between 2019 and 2020, 37.8% of 407 hypertensive patients reported having depression22.
A meta-analysis of 41 studies conducted in high-income countries, such as China, revealed that self-reported depression was present in 28.5% of hypertensive patients23. Our study's high prevalence of self-reported depression could be explained by differences in environmental variables, genetics, or even sample size.
Female sex was associated with the presence of self-reported depression among hypertensives in our study. This identical finding has been reported in the literature20,22,24. This could be explained by hormonal variations between the sexes as well as psychosocial variables connected with feminine gender conceptions25. Indeed, parents engage with their child differently depending on whether it is a boy or a girl at birth. This affiliation with the feminine or masculine gender influences how adults perceive their own depression symptoms. Thus, because the masculine gender is associated with attributes such as emotional control and independence, men are much less likely to seek medical attention when they have symptoms of depression, whereas women, whose gender identity construction makes them more fragile than men, are more likely to consult when they are not feeling well.
Stress was associated with self-reported depression in our study. Patients' dissatisfaction with the healthcare system could explain this stress26, concerns of the problems that their disease may entail, and their low socioeconomic status, which is an impediment to proper hypertension control.
Salt is required for the maintenance of osmotic pressure, plasma and interstitial volumes, acid–base balance, cell electrical activity, and the cardiovascular system's reaction to endogenous vasopressors. To reduce blood pressure, the WHO advises a salt diet of fewer than 5 g per person27. Subjects with hypertension are subjected to a low-salt diet, which might cause the emergence of depressive symptoms, especially since the low-salty diet is a lifelong diet. This self-reported depression could be attributed primarily to the blandness of meals and patients' perceptions of being in control. In our study, being on a low-salty diet was associated with self-reported depression.
In our study, pain and physical discomfort in hypertensives were related to the prevalence of depression. This could occur as a result of feelings of worthlessness and powerlessness, as well as low self-esteem. According to the scientific literature, pain and depression have common processes. They have norepinephrine and serotonin neurotransmission. In depression, a decrease in these neurotransmitters may disrupt the functioning of inhibitory corticospinal pathways that modulate the activity of nociceptive neurons in the posterior horn, causing the patient to experience pain stimuli relevant to his organism's normal functioning28. Depression is also associated with cognitive and affective alterations, which can lead to an especially negative perception of body experiences. This is followed by a chain reaction of hypervigilance toward symptoms and avoidance of movement, which can lead to an amplification of pain perception29.
The presence of self-reported depression associated with urban areas in our study Indeed, living in an urban setting is a risk factor for mental health decline30. Factors such as a lack of green space and bodies of water, population density, and the frantic pace of urban life can all contribute to increased sensitivity to social stress and mental exhaustion31. In Europe and the United States, depression is 39% more common in urban areas than in rural areas32.
Self-monitoring of blood pressure enables people with hypertension to be empowered and regulate their blood pressure. Lack of self-monitoring was associated with self-reported depression in our study. This could be explained by patients' lack of motivation and denial of the disease, their inadequate awareness of arterial hypertension, their poor level of education, and the complexity of blood pressure measurement. Add to it a lack of social support from family, friends, and entourage.
In our study, an unsatisfactory relationship with the healthcare system was associated with self-reported depression. This would be related to the helplessness that hypertensive patients feel as a result of the lack of anti-hypertensive medicines at the primary health care facilities, which can last many months, the high cost of these drugs, and the low monthly income per household. This encourages consumers not to purchase medicine in the case of a stock shortage and leaves them concerned about their health as a result of the consequences that HBP might create if blood pressure levels are not controlled.
In our study, having a family history of arterial hypertension was associated with self-reported depression. This could be due to concerns about potential consequences such as strokes and myocardial infarction, as well as patients' disinterest in illness care.
In our work, the presence of self-reported depression was connected with the patient's assessment of the detrimental effects of antihypertensive medicines. This could be explained by the patient's lack of drive and anxiety about the disease's complications.
Limitations of the study
Our study was able to meet its objectives; however, certain limitations were present, such as the bias of prevarication encountered during the collection of economic and behavioral data and the cross-sectional design of the study, which makes it impossible to demonstrate a causal relationship between exposure and the occurrence of self-reported depression.
Although the study suggests a high prevalence of depression, possibly linked to the COVID-19 infection, this is not entirely accurate. Indeed, the period between 2021 and 2022 was characterized by a return to normal life.
Conclusion
Hypertensive patients are vulnerable when it comes to mental health issues. Our findings show an important prevalence of self-reported depression. Following these findings, it is suggested that mental health be included in the care and follow-up of hypertensive patients.
Data availability
All data generated or analyzed during this study are included in this published article.
References
Nations-Unies. Plus de 700 millions de personnes souffrent d’hypertension non traitée (OMS). https://news.un.org/fr/story/2021/08/1102342 (2021). Accessed 08 May 2023.
Kearney, P. M. et al. Global burden of hypertension: Analysis of worldwide data. Lancet 365, 217–223 (2005).
Essayagh, T. et al. Prevalence of uncontrolled blood pressure in Meknes, Morocco, and its associated risk factors in 2017. PLoS ONE 14, e0220710 (2019).
Organisation mondiale de la santé. Maladies cardiovasculaires. 2015 http://www.who.int/fr/news-room/fact-sheets/detail/cardiovascular-diseases-(cvds). Accessed 08 May 2023.
Essayagh, M., Essayagh, T. & Essayagh, S. Drug non-adherence in hypertensive patients in Morocco, and its associated risk factors. Eur. J. Cardiovasc. Nurs. https://doi.org/10.1093/eurjcn/zvaa002 (2020).
Ministère de la Santé, M. Enquête Nationale sur Les Facteurs de Risque Communs Des Maladies Non Transmissibles, 2017–2018, Maroc. https://www.sante.gov.ma/Publications/Etudes_enquete/Pages/default.aspx (2019). Accessed 08 May 2023.
Programme de Prévention et de Contrôle de l’hypertension Artérielle. (Service des maladies cardiovasculaires, Division des maladies non transmissibles, Direction d’épidémiologie et de lutte contre les maladies, 2017). Accessed 08 May 2023.
Abdisa, L., Letta, S. & Nigussie, K. Depression and anxiety among people with hypertension on follow-up in Eastern Ethiopia: A multi-center cross-sectional study. Front Psychiatry 13, 853551 (2022).
World Health Organization. Monitoring Mental Health Systems and Services in the WHO European Region: Mental Health Atlas, 2017. (2019).
Saboya, P. M. H. P., Zimmermann, P. R. & Bodanese, L. C. Association between anxiety or depressive symptoms and arterial hypertension, and their impact on the quality of life. Int. J. Psychiatry Med. 40, 307–320 (2010).
Haut-Commissariat-au Plan. Monographie générale de la région de Marrakech-Safi | Portail national des collectivités territoriales. (2020). Accessed 08 May 2023.
Ministère de la Santé, M. Santé en chiffres. https://www.sante.gov.ma/Documents/2023/03/Sante%20en%20chiffre%202021%20VF%20(1).pdf (2021). Accessed 08 May 2023.
AlHadi, A. N. et al. An arabic translation, reliability, and validation of Patient Health Questionnaire in a Saudi sample. Ann. Gen. Psychiatry 16, 1–9 (2017).
Kroenke, K., Spitzer, R. L. & Williams, J. B. W. The PHQ-9: Validity of a brief depression severity measure. J. Gen. Intern. Med. 16, 606 (2001).
Mancia, G. et al. 2013 ESH/ESC Guidelines for the management of arterial hypertension: the Task Force for the management of arterial hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). J. Hypertens. 31, 1281–1357 (2013).
Essayagh, F. et al. Disease burden among migrants in Morocco in 2021: A cross-sectional study. PLoS ONE 18, e0281129 (2023).
Word Health Organization. Obesity and overweight. https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight/. Accessed 08 May 2023.
Ademola, A. et al. Prevalence and determinants of depression among patients with hypertension: A cross-sectional comparison study in Ghana and Nigeria, Niger. J. Clin. Pract. 22, 558–565 (2019).
Valladares-Garrido, M. J. et al. Depression among Peruvian adults with hypertension and diabetes: Analysis of a national survey. Diabetes Metab. Syndrome Clin. Res. Rev. 14, 141–146 (2020).
Mahmood, S. et al. Prevalence and predictors of depression amongst hypertensive individuals in Karachi, Pakistan. Cureus 9, e1397 (2017).
Hamrah, M. S. et al. Anxiety and depression among hypertensive outpatients in Afghanistan: A cross-sectional study in Andkhoy City. Int. J. Hypertens 2018, 8560835 (2018).
Asmare, Y., Ali, A. & Belachew, A. Magnitude and associated factors of depression among people with hypertension in Addis Ababa, Ethiopia: A hospital based cross-sectional study. BMC Psychiatry 22, 1–8 (2022).
Li, Z. et al. Prevalence of depression in patients with hypertension: A systematic review and meta-analysis. Medicine 94, e1317 (2015).
Ashok, V. G. & Ghosh, S. S. Prevalence of depression among hypertensive patients attending a rural health centre in Kanyakumari. Natl. J. Community Med. 10, 172–175 (2019).
McHenry, J., Carrier, N., Hull, E. & Kabbaj, M. Sex differences in anxiety and depression: Role of testosterone. Front. Neuroendocrinol. 35, 42 (2014).
Essayagh, F. et al. The prevalence and risk factors for anxiety and depression symptoms among migrants in Morocco. Sci. Rep. 13, 3740 (2023).
Chatelanat, O., Pechère-Bertschi, A. & Ponte, B. Sensibilité au sel et hypertension artérielle. Rev. Med. Suisse 15, 1625–1628 (2019).
Stahl, S. M. Does depression hurt?. J. Clin. Psychiatry 63, 273–274 (2002).
Rentsch, D. et al. Douleurs chroniques et dépression: un aller-retour?. Rev. Med. Suisse 208, 1364–1369 (2009).
Blazer, D. et al. Psychiatric disorders. A rural/urban comparison. Arch. Gen. Psychiatry 42, 651–656 (1985).
Berman, M. G., Jonides, J. & Kaplan, S. The cognitive benefits of interacting with nature. Psychol. Sci. 19, 1207–1212 (2008).
Peen, J., Schoevers, R. A., Beekman, A. T. & Dekker, J. The current status of urban-rural differences in psychiatric disorders. Acta Psychiatr. Scand. 121, 84–93 (2010).
Author information
Authors and Affiliations
Contributions
F.Z.B., S.B., F.E., O.T., M.E., S.E., and T.E.: Conceptualization, methodology, investigation, analysis, project administration, validation, and writing original draft; A.A.N., M.A., A.L.: writing original draft.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Boukhari, F.Z., Belayachi, S., Essayagh, F. et al. Self-reported depression and its risk factors among hypertensive patients, Morocco: a cross-sectional study. Sci Rep 14, 11196 (2024). https://doi.org/10.1038/s41598-024-61390-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-61390-y
Keywords
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.