Abstract
The proteins encoded by the excision repair cross-complementing (ERCC) family are pivotal in DNA damage repair and maintaining genome stability. However, the precise role of the ERCC family in tumor prognosis and the effectiveness of immune checkpoint inhibitors (ICI) therapy remain uncertain. This study aimed to explore the connection between ERCC mutations and prognosis as well as the response to ICI. We observed that patients with ERCC mutations exhibited enhanced progression-free survival (PFS) and overall survival (OS) in two independent pan-cancer cohorts. Furthermore, this mutant subgroup showed higher tumor mutation burden (TMB) compared to the wild-type subgroup. Notably, ERCC mutations were associated with better OS (HR 0.54, 95% CI 0.42–0.70; P < 0.001) in pan-cancer patients who underwent ICI therapy (N = 1661). These findings were validated in a separate cohort, where patients in the ERCC mutant subgroup demonstrated improved clinical outcomes (HR 0.56, 95% CI 0.37–0.84; P = 0.03) and higher response rates (51.9% vs. 26.8%) than the wild-type subgroup. Further analysis revealed that patients with ERCC mutations displayed elevated tumor neoantigen burden (TNB) levels and increased infiltration of immune-response cells. Our study suggests that ERCC mutations are linked to enhanced immunogenicity and improved ICI efficacy, thus potentially serving as a biomarker for ICI therapy.
Similar content being viewed by others
Introduction
Immune checkpoint inhibitors (ICI) have shown significant improvements in clinical outcomes for patients with advanced or metastatic cancer1. ICI therapy is now a first-line treatment option for certain cancer types, such as metastatic melanoma, colorectal cancer, and non-small cell lung cancer (NSCLC)2. However, only a small proportion of patients respond positively to ICI therapy3. To identify patients who could potentially benefit from ICI treatment, the FDA has approved programmed death ligand-1 (PD-L1), high microsatellite instability (MSI-H), and tumor mutation burden (TMB) as biomarkers, but these are sometimes ineffective in predicting ICI responses. For instance, patients with negative PD-L1 or MSS status may still benefit from ICI treatment4,5. Additionally, researchers have identified tumor neoantigen load (TNB), intratumor heterogeneity, T cell-inflamed gene expression profile (GEP), and mutations in various cancer-related genes (such as TP53, PTPRT, KMT2 family, etc.) as supplementary predictors of ICI response6,7. Therefore, identifying biomarkers for ICI therapy is crucial for improving the efficiency of immunotherapy8.
Proteins encoded by the ERCC family (ERCC1, ERCC2, ERCC3, ERCC4, ERCC5, ERCC6, and ERCC8) are essential components of the complex nucleotide excision repair (NER) process9, playing a critical role in DNA damage repair and maintaining genome integrity10,11. For example, the proteins XPD and XPB, encoded by ERCC2 and ERCC3 respectively, act as helicase subunits of the transcription factor IIH (TFIIH) complex and are necessary for DNA damage verification12,13. After DNA damage verification, ERCC1 and XPF (encoded by ERCC4) form a heterodimer XPF-ERCC1, which, together with XPG (encoded by ERCC5), catalyzes the excision of DNA damage14. ERCC6 (also known as CSB) and ERCC8 (also known as CSA) are required for the assembly of the transcription-coupled NER machinery, which detects damage through its ability to sense transcription extension blockages15.
Numerous studies have suggested a close relationship between alterations in the ERCC family and the occurrence and development of cancer. For instance, several meta-analyses have demonstrated that single nucleotide polymorphisms of ERCC2, ERCC3, and ERCC4 are associated with the risk of skin, breast, and lung cancers16,17,18. Li et al. found that ERCC2 mutations increase cisplatin sensitivity in bladder cancer chemotherapy19, and studies by Stradella et al. showed that ERCC3 mutations may elevate the risk of breast and ovarian cancer20,21. Additionally, the expression level of ERCC family genes has been linked to cancer prognosis. For example, Zhao et al. discovered that the expression level of ERCC4 correlates with overall survival (OS) in ovarian and gastric cancers22,23. ERCC5 downregulation has been identified as a biomarker for ovarian cancer prognosis and a potential therapeutic target24. However, the association between ERCC family mutations and ICI therapy response remains uncertain.
In this study, we analyzed available mutation and clinical data from public databases. Our findings revealed that patients with ERCC family mutations had a favorable prognosis in pan-cancer patients. Moreover, patients with ERCC mutations showed a higher TNB and increased infiltration of immune-response cells. Associations between ERCC mutations and improved ICI response were identified in the pan-cancer cohort, particularly in melanoma and NSCLC. Our study suggests that ERCC mutations may serve as biomarkers for tumor prognosis and ICI therapy.
Results
ERCC family genes were recurrently mutated in multiple cancer types
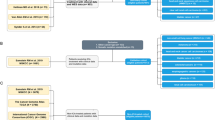
Figure 1 shows the flow chart of this study. Initially, we investigated the association between ERCC mutations and cancer prognosis in a pan-cancer cohort, using data from the cBioPortal database. Our focus was on four core cancer-related genes of the ERCC family (ERCC2, ERCC3, ERCC4, ERCC5), as they are frequently altered in various cancer types, and are part of the MSK-IMPACT panel25. The accumulated mutation frequency of the ERCC family exceeded 5% in seven cancer types (Fig. 2A), including uterine corpus endometrial carcinoma, melanoma, bladder urothelial carcinoma, stomach adenocarcinoma, colorectal adenocarcinoma, lung adenocarcinoma, lung squamous cell carcinoma. Interestingly, no hotspot mutations were observed in the ERCC family genes (Fig. 2B), indicating that the mutations are primarily loss-of-function mutations.
Frequency and mutation location of ERCC mutations among patients in the TCGA pan-cancer cohort are presented. (A) The frequency of ERCC mutations across 32 cancer types in patients who did not receive ICI therapy. (B) The information on protein domains and mutation locations for ERCC mutations. The color of the circle represents different non-silent mutation types. (C) The comparison of TMB between ERCC mutant and wild-type samples in pan-cancer. (D) The mutual exclusivity analysis reveals a tendency for co-occurrence of mutations among ERCC family genes.
Given that the ERCC family genes are primarily involved in DNA repair and play a crucial role in maintaining genome integrity, we sought to determine whether ERCC mutations are associated with TMB. As expected, the samples with ERCC mutations exhibited a higher TMB compared to the wild-type samples (Fig. 2C). Additionally, mutual exclusivity analysis on the cBioPortal database revealed a tendency for co-occurrence of mutations among ERCC family genes (Fig. 2D), emphasizing the relevance of mutations in these genes.
The relationship of ERCC mutations with the prognosis of cancer
The relationship between ERCC mutations and cancer prognosis was the next aspect of our investigation. For this analysis, we selected seven cancer types with a mutation frequency greater than 5% as cohort1 (Fig. 2A) to reduce background noise. The mutation frequencies were ranked as follows: ERCC5, ERCC2, ERCC4, and ERCC3 (Fig. 3A). Consistent with previous findings, cohort1 samples with ERCC mutations exhibited higher TMB than the wild-type samples (P < 10E−10, Fig. 3B). Furthermore, we divided patients into two subgroups based on ERCC mutation status: the ERCC mutant subgroup (ERCC-MT) and the ERCC wild-type subgroup (ERCC-WT). The results indicated that mutations in the ERCC family were associated with improved OS and progression-free survival (PFS) in pan-cancer patients (HR 0.75, 95% CI 0.62–0.91; P = 0.009; Fig. 3C; HR 0.82, 95% CI 0.68–0.98; P = 0.045; Fig. 3D). To validate these findings, we further analyzed an independent pan-cancer cohort (cohort2). The results showed that samples with ERCC mutations still had higher TMB (P < 10E−10, Fig. 3E), and patients in the ERCC-MT subgroup exhibited better clinical outcomes compared to the wild-type subgroup (HR 0.75, 95% CI 0.69–0.83; P < 0.001; Fig. 3F).
The impact of ERCC mutations on the survival outcomes of multiple cancer types was investigated. Firstly, we analysed the mutation patterns of ERCC family genes in seven cancer types, where the mutations exceeded 5% within the TCGA pan-cancer cohort (cohort1) (A). Next, we compared the TMB between the ERCC-mutant (ERCC-MT) subgroup and the ERCC-wildtype (ERCC-WT) subgroup in cohort1 (B). Subsequently, we assessed the overall survival (C) and progression-free survival (D) of patients in the ERCC-MT subgroup compared to the ERCC-WT subgroup in cohort1. Furthermore, we examined the TMB differences between the ERCC-MT subgroup and ERCC-WT subgroup in the MSK-MET pan-cancer cohort (cohort2) (E). Finally, we analysed the OS of patients in cohort2 based on ERCC mutation status (F).
ERCC mutations linked with improved ICI efficacy in multiple cancer types
Previous studies have demonstrated the association of certain cancer-related genes (e.g., PTPRT, MUC16, KMT2 family, FAT family genes etc.) with the response to ICI therapy26,27,28,29. Given the close involvement of ERCC family genes in DNA damage repair and the potential for ERCC mutations to result in higher TMB, we aimed to explore the relationship between ERCC mutations and ICI-treated response. To address this, we initially investigated the well-known pan-cancer cohort (cohort3, N = 1661) published by the MSKCC30. As anticipated, patients in the ERCC-MT subgroup exhibited a higher TMB than those in the wild-type subgroup (Fig. 4A). Moreover, the clinical outcome of patients in the ERCC-MT subgroup surpassed that of the ERCC-WT subgroup (HR 0.54, 95% CI 0.42–0.70; P < 0.001; Fig. 4B). Given that ERCC family genes are frequently mutated in melanoma and NSCLC, we further examined the impact of ERCC mutations on the prognosis of patients with melanoma and NSCLC within this cohort. The results revealed that patients in the ERCC-MT subgroup had more favorable survival outcomes compared to the ERCC-WT subgroup (HR 0.62, 95% CI 0.42–0.90; P = 0.035; Fig. 4C).
ERCC family mutations have been found to be associated with the clinical benefit of ICI therapy in various types of cancer. Here, we present the following analyses: (A) an evaluation of tumor mutational burden (TMB) between the ERCC-mutant (ERCC-MT) subgroup and ERCC-wild type (ERCC-WT) subgroup in cohort3. (B) Kaplan–Meier (KM) plot depicting the association of ERCC family mutations with the prognosis of patients in cohort3 who received ICI therapy. (C) KM plot focusing on melanoma and NSCLC patients in cohort3 who received ICI therapy. (D) Evaluation of TMB between the ERCC-MT subgroup and ERCC-WT subgroup in cohort4. (E) KM plot representing the survival outcomes of patients in cohort4 who received ICI therapy. (F) Clinical response analysis of patients in cohort4 who underwent ICI therapy.
To ascertain the impact of ERCC mutations on the efficacy of ICI, we conducted an analysis in an independent cohort comprising 459 patients with melanoma and NSCLC who received ICI treatment (cohort4). Our investigation revealed that patients in the ERCC-MT subgroup exhibited a higher TMB compared to those in the ERCC-WT subgroup (Fig. 4D). Additionally, we observed similar results in terms of ERCC mutations correlating with improved survival outcomes (HR 0.56, 95% CI 0.37–0.84; P = 0.03; Fig. 4E). Moreover, a notable increase in the proportion of patients with clinical responses (complete response or partial response) was also evident in the ERCC mutated subgroup (51.9% vs. 26.8%, Fisher exact test P = 0.005; Fig. 4F).
TNB and immune infiltration associated with ERCC mutations
Tumor neoantigens play a critical role in the recognition of cancer cells by the immune system as they represent neoepitopes presented on the cell membrane by tumor cells31,32,33. To explore the potential mechanisms underlying ERCC mutations, we conducted analyses of TNB and immunological factors. Remarkably, our findings revealed a significant association between ERCC mutations and higher TNB in the TCGA melanoma and NSCLC cohort (Fig. 5A), indicating a correlation with increased tumor immunogenicity. Even when we separately assessed the TNB of the TCGA-NSCLC and TCGA-melanoma cohorts, the ERCC-MT subgroup still exhibited significantly elevated TNB compared to the ERCC-WT subgroup (Both P < 0.05; Fig. 5B,C). Moreover, the CIBERSORT algorithm analysis demonstrated an enhanced infiltration of CD8+ T cells and other pro-inflammatory immunocytes (e.g., activated memory CD4+ T cells, M1 macrophages) in the ERCC-MT subgroup (Fig. 5D). These cell types are known to be positive factors in the context of ICI therapy34,35.
TNB and immune infiltration associated with ERCC mutations were evaluated as follows: (A) TNB comparison between the ERCC-MT subgroup and ERCC-WT subgroup in the TCGA NSCLC and Melanoma cohort; (B) TNB comparison between the ERCC-MT subgroup and ERCC-WT subgroup in the TCGA NSCLC cohort; (C) TNB comparison between the ERCC-MT subgroup and ERCC-WT subgroup in the TCGA Melanoma cohort; (D) Comparison of the infiltration scores of 22 immune cell types between the ERCC-MT and ERCC-WT subgroups (*p < 0.05; **p < 0.01; ***p < 0.001).
Discussion
ERCC family genes are known to play essential roles in the NER process and DNA damage repair36. Previous studies have suggested that ERCC genes may be involved in the tumorigenesis of various cancer types22,23. However, the relationship between ERCC genes and tumor prognosis has not been thoroughly investigated, and the association of ERCC mutations with ICI response remains uncertain. In this study, we observed recurrent mutations in ERCC genes in several cancer types, including melanoma, lung adenocarcinoma, lung squamous cell carcinoma, colorectal adenocarcinoma, and others. Interestingly, these mutations were found to be associated with a better prognosis in two independent pan-cancer cohorts. Additionally, ERCC mutations were linked to higher levels of TMB and TNB, indicating enhanced immunogenicity and potential favorable factors for ICI therapy. Notably, patients with ERCC mutations demonstrated improved clinical outcomes when treated with ICI, particularly those with melanoma and NSCLC.
We excluded ERCC1 from our analysis for two main reasons. Firstly, the MSK-IMPACT panels used in clinical immunotherapy studies typically include several hundred oncogenes, tumor suppressor genes, and members of pathways actionable by targeted therapies. However, ERCC1 was not part of all three different MSK-IMPACT panels (V1: 341 genes; V2: 410 genes; and V3: 468 genes), while ERCC2/3/4/5 were included in these panels30,37. Secondly, ERCC1 has a lower mutation frequency compared to other ERCC family genes. Similarly, we did not include ERCC6 and ERCC8 in our study for the same reasons.
In recent years, TMB has gained recognition as a promising biomarker for immunotherapy38,39. However, several limitations, such as the absence of a certain threshold, the cost of whole exome sequencing, and variations in sequencing platforms and analysis pipelines, have significantly impacted the clinical application of TMB40. In contrast, evaluating the mutation status of one or a few genes is more straightforward and cost-effective. ERCC mutation status can be determined through targeted region sequencing, reducing sequencing expenses and simplifying the assessment of TMB and immunotherapy efficacy. Several research groups are already exploring the feasibility of using a small number of genes as markers for immunotherapy. For instance, Rui-Hua Xu et al. demonstrated that patients with POLE or POLD1 mutations exhibited improved clinical outcomes with immunotherapy across various cancers41. Yue Yang et al. also revealed that the mutation status of MUC4, MUC16, and TTN was associated with the prognosis of gastric cancer and can be serve as a more economical and convenient marker for pan-cancer immunotherapy27.
The tumor microenvironment is another crucial factor associated with cancer prognosis and immunotherapy42,43. Previous studies have indicated that mutations in cancer-related genes may be correlated with the remodeling of the tumor microenvironment29,44. In this study, we observed that ERCC mutations were linked with increased infiltration of CD8+ T cells, along with other pro-inflammatory immunocytes (e.g., activated memory CD4+ T cells and M1 macrophages). These findings suggest that ERCC mutations are not only associated with heightened immunogenicity but may also contribute to a pro-inflammatory tumor microenvironment, which is more conducive to a positive response to ICI therapy.
This study has several limitations. Firstly, it is a retrospective study based on cohorts from previously published datasets, necessitating a prospective design for further validation. Secondly, the study includes several different cohorts comprising patients with different types and percentages of cancers. While these cohorts encompass several major cancer types (such as lung adenocarcinoma, lung squamous cell carcinoma, melanoma, colorectal adenocarcinoma, breast infiltrating ductal carcinoma, etc.), they may also introduce some bias in the data analysis. Additionally, the lack of experimental validation is another limitation.
In summary, through the integration of genomic alterations and clinical data, we have identified a potential association between ERCC mutations and the prognosis of multiple cancer types. Moreover, the mutation status of ERCC family genes is correlated with increased immunogenicity and improved clinical outcomes of ICI therapy, suggesting its potential as a biomarker for immunotherapy efficacy.
Materials and methods
Sample collection
Pan-cancer discovery cohort
The genomic alteration data (somatic mutations, including missense mutations, splice mutations, nonsense mutations, and indels) and clinical information on OS of TCGA samples across 32 cancer types were obtained by selecting “TCGA PanCancer Atlas Studies” from the cBioPortal database (https://www.cbioportal.org/, February 2022)45,46. Cohort1 (N = 3292) comprised seven cancer types with an ERCC family mutation frequency greater than 5%.
Pan-cancer validation cohort (cohort2)
A cohort consisting of 27 cancer types with over 25,000 samples from the Memorial Sloan Kettering—Metastatic Events and Tropisms (MSK-MET) dataset was used as a pan-cancer validation cohort (cohort2, N = 25,659)47.
Immunotherapy cohort
The somatic mutations and clinical annotation of ICI-treated pan-cancer data from 1661 patients (cohort3) at the Memorial Sloan-Kettering Cancer Center (MSKCC) were downloaded from the cBioPortal database (https://www.cbioportal.org/, February 2022)30. To further validate the predictive function of ERCC family mutations on ICI clinical response, we compiled a combined cohort of 459 ICI-treated patients (cohort4) from publicly available studies, comprising two cancer types: melanoma (N = 144)48, and NSCLC (N = 315)49,50. The clinical response information was obtained from the supplementary data of each study.
Acquisition of mutation burden and neoantigen burden
Tumor mutation burden (TMB) was defined as the log2 transformation of the total non-synonymous mutations per megabase for samples conducted with whole exome sequencing (cohort1, cohort4). For the MSKCC cohort (cohort2, cohort3) with target region sequencing, TMB data were obtained from the cBioPortal database. The neoantigen data of melanoma and NSCLC samples in the TCGA were acquired from the Cancer Immunome Atlas (TCIA, https://www.tcia.at/home) database.
Tumor-infiltrating immunocyte estimation
We utilized CIBERSORT to assess the abundance of 22 immunocyte subtypes, employing the LM22 signature51. The gene expression data of TCGA pan-cancer samples were obtained from the UCSC Xena database (https://toil-xena-hub.s3.us-east-1.amazonaws.com/download/tcga_RSEM_gene_tpm.gz). Subsequently, we used the gene expression data of NSCLC (containing lung adenocarcinoma and lung squamous cell carcinoma) and melanoma samples as inputs for the CIBERSORT algorithm.
Statistical analysis
The Wilcoxon test was employed to determine the significance of the TMB and TNB comparisons among different subgroups. Kaplan–Meier survival curves were utilized to statistically analyze the OS and PFS data, and the log-rank test was employed to calculate the P value between the various subgroups. All statistical calculations were conducted using the cBioportal online database or R software (version 4.2.1). Visualization was carried out using the survminer package (version 0.4.9), and the statistical analysis of survival data was performed using the Survival package (version 3.2-10).
Ethical approval
This study did not require ethical board approval because it did not contain human or animal trials.
Data availability
All data in this study were collected from the cBioPortal database (https://www.cbioportal.org), the UCSC Xena (https://pancanatlas.xenahubs.net), and TCIA database (https://www.tcia.at/home).
Abbreviations
- ICI:
-
Immune checkpoint inhibitors
- HR:
-
Hazard ratio
- TMB:
-
Tumor mutation burden
- TNB:
-
Tumor neoantigen burden
- ERCC:
-
Excision repair cross-complementing
- OS:
-
Overall survival
- PFS:
-
Progression-free survival
References
Pardoll, D. M. The blockade of immune checkpoints in cancer immunotherapy. Nat. Rev. Cancer 12(4), 252–264 (2012).
Bagchi, S., Yuan, R. & Engleman, E. G. Immune checkpoint inhibitors for the treatment of cancer: Clinical impact and mechanisms of response and resistance. Annu. Rev. Pathol. 16, 223–249 (2021).
Shi, F. et al. Sex disparities of genomic determinants in response to immune checkpoint inhibitors in melanoma. Front. Immunol. 12, 721409 (2021).
Carbone, D. P. et al. First-line nivolumab in stage IV or recurrent non-small-cell lung cancer. N. Engl. J. Med. 376(25), 2415–2426 (2017).
Hellmann, M. D., Ciuleanu, T.-E. & Paz-Ares, L. Nivolumab plus ipilimumab in lung cancer with a high tumor mutational burden. N. Engl. J. Med. 378(22), 2093–2104 (2018).
McGranahan, N., Furness, A. J. S. & Rosenthal, R. Clonal neoantigens elicit T cell immunoreactivity and sensitivity to immune checkpoint blockade. Science 351(6280), 1463–1469 (2016).
Cristescu, R. et al. Pan-tumor genomic biomarkers for PD-1 checkpoint blockade-based immunotherapy. Science 362(6411), eaar35593 (2018).
Jiang, T. et al. Comprehensive evaluation of NT5E/CD73 expression and its prognostic significance in distinct types of cancers. BMC Cancer 18(1), 267 (2018).
Marteijn, J. A., Lans, H., Vermeulen, W. & Hoeijmakers, J. H. Understanding nucleotide excision repair and its roles in cancer and ageing. Nat. Rev. Mol. Cell Biol. 15(7), 465–481 (2014).
Wakasugi, M., Reardon, J. T. & Sancar, A. The non-catalytic function of XPG protein during dual incision in human nucleotide excision repair. J. Biol. Chem. 272(25), 16030-4 (1997).
O’Donovan, A., Davies, A. A., Moggs, J. G., West, S. C. & Wood, R. D. XPG endonuclease makes the 3′ incision in human DNA nucleotide excision repair. Nature 371, 432–435 (1994).
Tapias, A. et al. Ordered conformational changes in damaged DNA induced by nucleotide excision repair factors. J. Biol. Chem. 279(18), 19074–19083 (2004).
Compe, E. & Egly, J. M. TFIIH: When transcription met DNA repair. Nat. Rev. Mol. Cell Biol. 13(6), 343–354 (2012).
Fagbemi, A. F., Orelli, B. & Schärer, O. D. Regulation of endonuclease activity in human nucleotide excision repair. DNA Repair (Amst) 10(7), 722–729 (2011).
van der Weegen, Y. et al. The cooperative action of CSB, CSA, and U`SA target TFIIH to DNA damage-stalled RNA polymerase II. Nat. Commun. 11(1), 2104 (2020).
Manuguerra, M. et al. XRCC3 and XPD/ERCC2 single nucleotide polymorphisms and the risk of cancer: A HuGE review. Am. J. Epidemiol. 164(4), 297–302 (2006).
Zhan, P. et al. ERCC2/XPD Lys751Gln and Asp312Asn gene polymorphism and lung cancer risk: A meta-analysis involving 22 case–control studies. J. Thorac. Oncol. 5(9), 1337–1345 (2010).
Sahaba, S. A. et al. The link of ERCC2 rs13181 and ERCC4 rs2276466 polymorphisms with breast cancer in the Bangladeshi population. Mol. Biol. Rep. 49(3), 1847–1856 (2022).
Li, Q. et al. ERCC2 helicase domain mutations confer nucleotide excision repair deficiency and drive cisplatin sensitivity in muscle-invasive bladder cancer. Clin. Cancer Res. 25(3), 977–988 (2019).
Stradella, A. et al. ERCC3, a new ovarian cancer susceptibility gene?. Eur. J. Cancer 141, 1–8 (2020).
Vijai, J. et al. A recurrent ERCC3 truncating mutation confers moderate risk for breast cancer. Cancer Discov. 6(11), 1267–1275 (2016).
Zhao, M. et al. Prognostic values of excision repair cross-complementing genes mRNA expression in ovarian cancer patients. Life Sci. 194, 34–39 (2018).
Luo, S. S., Liao, X. W. & Zhu, X. D. Prognostic value of excision repair cross-complementing mRNA expression in gastric cancer. Biomed Res. Int. 2018, 6204684 (2018).
Walsh, C. S. et al. ERCC5 is a novel biomarker of ovarian cancer prognosis. J. Clin. Oncol. 26(18), 2952–2958 (2008).
Zehir, A. et al. Mutational landscape of metastatic cancer revealed from prospective clinical sequencing of 10,000 patients. Nat. Med. 23(6), 703–713 (2017).
Zhang, P. & Huang, Y. Genomic alterations in KMT2 family predict outcome of immune checkpoint therapy in multiple cancers. J. Hematol. Oncol. 14(1), 39 (2021).
Yang, Y. et al. MUC4, MUC16, and TTN genes mutation correlated with prognosis, and predicted tumor mutation burden and immunotherapy efficacy in gastric cancer and pan-cancer. Clin. Transl. Med. 10(4), e155 (2020).
Zhang, R., Wu, H. X., Xu, M. & Xie, X. KMT2A/C mutations function as a potential predictive biomarker for immunotherapy in solid tumors. Biomark. Res. 8(1), 71 (2020).
Zhang, W. et al. Association of PTPRT mutations with immune checkpoint inhibitors response and outcome in melanoma and non-small cell lung cancer. Cancer Med. 11(3), 676–691 (2022).
Samstein, R. M. et al. Tumor mutational load predicts survival after immunotherapy across multiple cancer types. Nat. Genet. 51(2), 202–206 (2019).
Liang, Z. et al. The common neoantigens in colorectal cancer are predicted and validated to be presented or immunogenic. bioRxiv (2019).
Guo, Z. et al. Durable complete response to neoantigen-loaded dendritic-cell vaccine following anti-PD-1 therapy in metastatic gastric cancer. NPJ Precis. Oncol. 6(1), 34 (2022).
Chen, C. et al. A comprehensive survey of genomic alterations in gastric cancer reveals recurrent neoantigens as potential therapeutic targets. Biomed Res. Int. 2019, 2183510 (2019).
Zeng, D. et al. Macrophage correlates with immunophenotype and predicts anti-PD-L1 response of urothelial cancer. Theranostics 10(15), 7002–7014 (2020).
Liu, R. et al. Influence of tumor immune infiltration on immune checkpoint inhibitor therapeutic efficacy: A computational retrospective study. Front. Immunol. 12, 685370 (2021).
Yin, Z. et al. Association between polymorphisms in DNA repair genes and survival of non-smoking female patients with lung adenocarcinoma. BMC Cancer 9, 439 (2009).
Cheng, D. T. et al. Memorial Sloan Kettering-integrated mutation profiling of actionable cancer targets (MSK-IMPACT): A hybridization capture-based next-generation sequencing clinical assay for solid tumor molecular oncology. J. Mol. Diagn. 17(3), 251–264 (2015).
McGrail, D. J. et al. High tumor mutation burden fails to predict immune checkpoint blockade response across all cancer types. Ann. Oncol. 32(5), 661–672 (2021).
Cao, D., Xu, H., Xu, X., Guo, T. & Ge, W. High tumor mutation burden predicts better efficacy of immunotherapy: A pooled analysis of 103078 cancer patients. OncoImmunology 8(9), e1629258 (2019).
Addeo, A., Friedlaender, A., Banna, G. L. & Weiss, G. J. TMB or not TMB as a biomarker: That is the question. Crit. Rev. Oncol. Hematol. 163, 103374 (2021).
Wang, F., Zhao, Q. & Xu, R.-H. Evaluation of POLE and POLD1 mutations as biomarkers for immunotherapy outcomes. JAMA Oncol. 5(10), 1504–1506 (2019).
DeBerardinis, R. J. Tumor microenvironment, metabolism, and immunotherapy. N. Engl. J. Med. 382(9), 869–871 (2020).
Altorki, N. K. et al. The lung microenvironment: An important regulator of tumour growth and metastasis. Nat. Rev. Cancer 19(1), 9–31 (2019).
Zhang, W. et al. Favorable immune checkpoint inhibitor outcome of patients with melanoma and NSCLC harboring FAT1 mutations. NPJ Precis. Oncol. 6(1), 46 (2022).
Cerami, E. et al. The cBio cancer genomics portal: An open platform for exploring multidimensional cancer genomics data. Cancer Discov. 2(5), 401–404 (2012).
Gao, J. et al. Integrative analysis of complex cancer genomics and clinical profiles using the cBioPortal. Sci. Signal. 6(269), pl1 (2013).
Bastien, N. et al. Genomic characterization of metastatic patterns from prospective clinical sequencing of 25,000 patients. Cell 185(3), 563-575.e11 (2022).
Liu, D. et al. Integrative molecular and clinical modeling of clinical outcomes to PD1 blockade in patients with metastatic melanoma. Nat. Med. 25(12), 1916–1927 (2019).
Hellmann, M. D. et al. Genomic features of response to combination immunotherapy in patients with advanced non-small-cell lung cancer. Cancer Cell 33(5), 843-852.e4 (2018).
Hira, R. et al. Molecular determinants of response to anti-programmed cell death (PD)-1 and anti-programmed death-ligand 1 (PD-L1) blockade in patients with non-small-cell lung cancer profiled with targeted next-generation sequencing. J. Clin. Oncol. 36(7), 633–641 (2018).
Newman, A. M. et al. Robust enumeration of cell subsets from tissue expression profiles. Nat. Methods 12(5), 453–457 (2015).
Acknowledgements
This research was supported by the Open Fund Project of BGI-Shenzhen (BGIRSZ20200003), the Basic and Applied Basic Research Foundation of Guangdong Province under Grant No. 2022A1515111138, the UMHS-PUHSC Joint Institute Project [2019020(PUSH)-r1], the Shenzhen Science and Technology Project (JCYJ20180228175531145), the Shenzhen High-level Hospital Construction Fund, and the Peking University Shenzhen Hospital Scientific Research Fund KYQD2023229.
Author information
Authors and Affiliations
Contributions
C.C. and H.L. performed the statistical analysis and wrote the manuscript with Y.L.’s assistance. J.L. designed and provided financial support for the study. C.C. reviewed the manuscript and provided corrections.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Chen, C., Liu, H., Li, Y. et al. Association of ERCC family mutations with prognosis and immune checkpoint inhibitors response in multiple cancers. Sci Rep 13, 13925 (2023). https://doi.org/10.1038/s41598-023-40185-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-023-40185-7
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.