Abstract
In malaria epidemiology, interpolation frameworks based on available observations are critical for policy decisions and interpreting disease burden. Updating our understanding of the empirical evidence across different populations, settings, and timeframes is crucial to improving inference for supporting public health. Here, via individual-based modeling, we evaluate a large, multicountry, contemporary Plasmodium falciparum severe malaria dataset to better understand the relationship between prevalence and incidence of malaria pediatric hospitalizations - a proxy of malaria severe outcomes- in East-Africa. We find that life-long exposure dynamics, and subsequent protection patterns in children, substantially determine the likelihood of malaria hospitalizations relative to ongoing prevalence at the population level. Unsteady transmission patterns over a lifetime in children -increasing or decreasing- lead to an exponential relationship of hospitalization rates versus prevalence rather than the asymptotic pattern observed under steady transmission. Addressing this increase in the complexity of malaria epidemiology is crucial to update burden assessments via inference models that guide current and future policy decisions.
Similar content being viewed by others
Introduction
Assessing the burden of malaria life-threatening outcomes in populations at risk is a critically important step in evaluating and improving control efforts. Malaria mortality is challenging to measure accurately in the community1 but remains a fundamental component of statistical-based interpolation from prevalence estimates, resulting in high uncertainty2. Inference of disease burden has been approached with different grades of sophistication, ranging from purely data-driven fits to multi-level mechanistic microsimulations3,4,5,6. Independent of the complexity of the approach, the ability of a model to generate accurate, robust, and valid malaria disease outcomes using exposure predictors, such as prevalence, requires (1) high-quality data as input from real-world observations, and (2) a comprehensive understanding and identification of the key factors determining the relationship between exposure and clinical outcomes.
Severe, life-threatening malaria syndromes presenting to hospitals are a valuable proxy for malaria-related death among communities. High exposure rates in children at a very young age are known to offset the risk of severe clinical outcomes at older ages7. This leads to a characteristic asymptotic pattern between exposure and disease risk at the population level, consistent with consensual malaria theory and historical observations4,7,8,9. Recent work has assessed the empirical relationship between community prevalence and the risk of severe malaria syndromes, namely severe anemia, cerebral malaria, and respiratory distress among children in East Africa, based on the largest standardized Plasmodium falciparum malaria pediatric dataset available to date10. Findings show that the occurrence of these severe malaria outcomes in the population may relate differently to increasing community prevalence. Particularly, an asymptotic relationship was observed when predicting severe anemia over community prevalence, while an exponential relationship was favored when predicting a combined outcome comprising the three syndromes. Evaluating new sources of standardized data, such as this contemporary dataset, contextualized with historical sources of data9,11 improves our understanding of the accuracy, robustness, and validity of the inference frameworks.
Here, we use a previously validated multi-level individual-based malaria model12, OpenMalaria (https://github.com/SwissTPH/openmalaria/wiki), to systematically investigate clinical and epidemiological factors influencing the relationship between potentially life-threatening hospital malaria admissions among children upon a given observed community prevalence. We use community-based malaria hospitalization incidence rates in small catchment populations and adjusted for case under-ascertainment as an empirical proxy of the incidence of severe malaria outcomes. Our analysis framework interrogates standardized malaria data obtained in Sub-Saharan African time-sites within the 1990s throughout 20209,10,11,13, aiming to improve and update our understanding of the dynamics from P. falciparum malaria infection to the occurrence of severe outcomes in children.
Results
Malaria admissions were assembled from individual records of 21 hospitals representing 35 time-sites in Kenya, Uganda, and Tanzania, among children resident in specific catchment areas -within a defined distance radius from the hospital where surveillance took place- excluding urban settings where it was possible to estimate single-year censused population estimates. We assume that the hospitalization rates per time-site represent a lower limit of the hospitalization incidence and can be reasonably comparable when further adjusting for case ascertainment. Cases were included if malaria was the primary cause of hospitalization, and those with underlying conditions were excluded10,13. We further used data on malaria hospitalization incidence obtained with similar approaches between 1992 and 1997 at seven hospital time-site locations in Kenya, The Gambia, and Malawi9,11. This allows us to compare and interpret our findings with a dataset that has been classically used for informing malaria inference models4,8,14 aiming to estimate severe outcomes of malaria across populations.
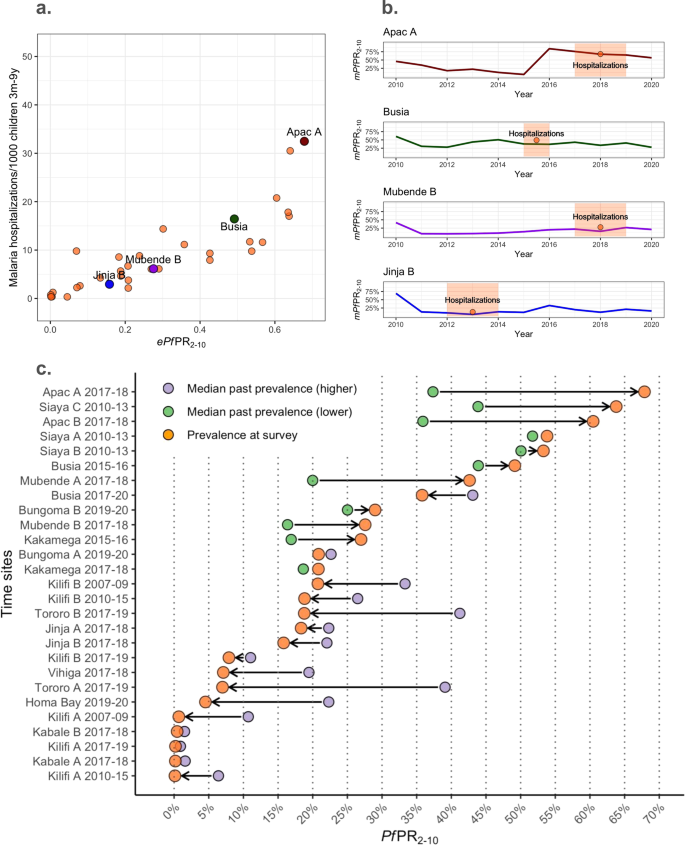
For each of the time-sites in the above datasets, the average number of hospitalizations due to malaria among children three months to 9 years old per 1000 children per year were paired with age-diagnostic method standardized community prevalence estimates, as empirical P. falciparum Parasite Rates among children 2–10 years old (ePf PR2–10). The data was obtained from community and school surveys undertaken during the period of hospital surveillance within the same catchment areas9,10,11. Further, we assessed the past exposure dynamics using catchment site-specific time-series of modeled age- and test-standardized parasite rates estimates, herein referred to as mPfPR2–10. For each time-site of the contemporary dataset, annual mPfPR2–10 estimates were obtained using a Bayesian hierarchical geospatial model detailed elsewhere13,15. In those time sites where modeled estimates were available for at least 7 past years (n = 27), and up to a maximum of 9 years, we computed the median mPfPR2–10 of the time series. We assume that the median prevalence across the past 7–9 years roughly represents the cumulative past transmission to which the population of children up to 10 years of age have been long-life, which can then be compared to the empirical prevalence at the time of the survey to evaluate the gap between past and present-day transmission
Visual inspection of the empirical relationship between prevalence and hospitalization rates for the 35 time-sites included in the contemporary dataset does not suggest an asymptotic relationship of malaria hospitalization incidence across the ePf PR2–10 range within the full dataset (Fig. 1a.). For illustration, we highlight four representative time-sites in Fig. 1a and alongside the mPfPR2–10 time-series of these time-sites for the years prior to the collection of the empirical data (Fig. 1b). Three major patterns of time-varying transmission are depicted, showing (1) a substantial increase in the mPfPR2–10(Apac A), (2) relative constant mPfPR2–10 (e.g, Busia) (3) steady increase (Mubende B) and 4) substantial decrease in the PfPR2–10(e.g., Jinja B). As depicted in Fig. 1c, there is substantial change between the ePf PR2–10 and the median value of the mPfPR2–10 over the previous years for each of the time-sites comparing at least seven years and up to ten years of modeled past exposure estimates. The difference between the ePf PR2–10 and the median value of past mPfPR2–10 can be interpreted as the gap in past exposure relative to ongoing exposure. For those time-sites at the higher end of the current ePfPR2–10 range (i.e., higher than the median empirical prevalence, 20%), exposure had primarily substantially increased or remained relatively stable (12 out of 14 sites). For those time sites at the lower end of the range (lower than 20%), exposure had decreased or remained relatively stable (13 out of 13 sites). All available mPfPR2–10 time series for the 35-time sites are shown in Fig. S113,15.
a The ePf PR2–10-severe malaria incidence empirical relationships highlighting four representative time-sites (red, green, purple, and blue colored dots) within all time-sites (orange dots). b Present day mPfPR2–10 over time in four representative time-sites (red, green, purple, and blue colored lines) and time-site ePf PR2–10 (orange) with highlighted time periods for which hospitalization incidence estimates were available for the empirical relations in (a). c Summarizing the prevalence trends over time estimated for each time-site as an increasing trend -when the estimated median mPfPR2–10 in the past 7 to 9 years is lower than the ePf PR2–10 at the time of assessment of severe outcomes incidence- or decreasing trend the estimated median mPfPR2–10 in the past 7–9 years is lower than the ePf PR2–10 at the time of assessment of severe outcomes incidence. The median past mPfPR2–10 per time-site is plotted as yellow (for those with increasing trends) or red (for those time-sites with reducing trends), and ePf PR2–10 per time-site is plotted in orange. Estimates have been computed among the 27-time sites with at least seven years of available past mPfPR2–10 estimates.
Understanding the complex relationship between malaria exposure, immunity, and clinical outcomes across populations and time requires causal analytical frameworks that (a) can combine empirical observations with theory (b) can address multiple interacting causal effects, threshold dynamics, and interference (c) have generally accepted principles to build the models, populate and calibrate their parameters and test their predictions for avoiding misspecification. Individual-based models are amongst the few modeling tools that fulfill these requirements1,2.
Open-Malaria (https://github.com/SwissTPH/openmalaria/wiki) is an multi-level individual-based model that includes several key features that allow to generate counterfactuals of the effect of malaria exposure on clinical disease under different scenarios of population structure, changing transmission, health-access, diagnostic thresholds, drug-efficacy, and other major malaria control and prevention interventions3. Random effects can be incorporated into the modeled processes and allow the inclusion of uncertainty and heterogeneity in the simulations. Relevant to our analyses, the framework encompasses submodels specifically parameterized to empirical data including (1) population structure4,5; (2) within-host dynamics of parasite burden and addressing the effect on single individuals of repeated infections in developing immunity and subsequent infections6,7,8; (3) disease progression6,7 and health-seeking behavior including rates of individuals accessing health services, as well as time to diagnostic and treatment4; (4) efficacy of case-management including diagnostic sensitivity and specificity, first- and second-line treatment effectiveness and efficacy of hospitalization4; and (5) the effect of age-structured comorbidities on severe malaria outcomes upon infection5. Further details are provided in the Supplementary Note 2.
We iteratively interrogated the data under different sets of plausible parameterizations of our individual-based model, hereafter referred to as scenario analysis. The scenario analysis explores hypotheses of the impact of well-known determinants on disease risk and changes in contemporary disease risk compared to historical observations, including the deployment and availability of artemisinin-derivatives in primary- and hospital-care, improved treatment adherence, the reduction in the occurrence and progression of malaria-associated comorbidities. In addition to addressing the detailed major key changes between the historical and contemporary datasets, we further address the life-long exposure dynamics evidenced by the modeled community prevalence estimates (Fig. 1b and Fig. S1). The risk of malaria disease outcomes, including those severe, depends on immunity, which in turn depends on previous exposure dynamics. We hypothesize that the year-to-year variability of PfPR could strongly influence the risk of hospitalization. Thus, we further assessed the impact of this variability on malaria exposure on the ongoing hospital admission risk estimated from our individual-based model scenarios. Here, we define steady exposure as the exposure of a specific population that does not change substantially over the years, and we define unsteady exposure as an exposure that shows substantial increasing or decreasing dynamics over time. We performed simulations that included generic step-up and step-down exposure dynamics with differences between pre- and intra-survey prevalence within the range of those observed empirically. Further details are found in the Supplementary Note 3. For each scenario analysis, we performed over 1000 individual-based simulations. We tested the model outputs—PfPR2–10 and incidence rate of malaria admissions—against three regression models, namely an intercept-only, a log-logistic, and a log-linear model, which was previously used to evaluate the prevalence-hospitalization relationship10.
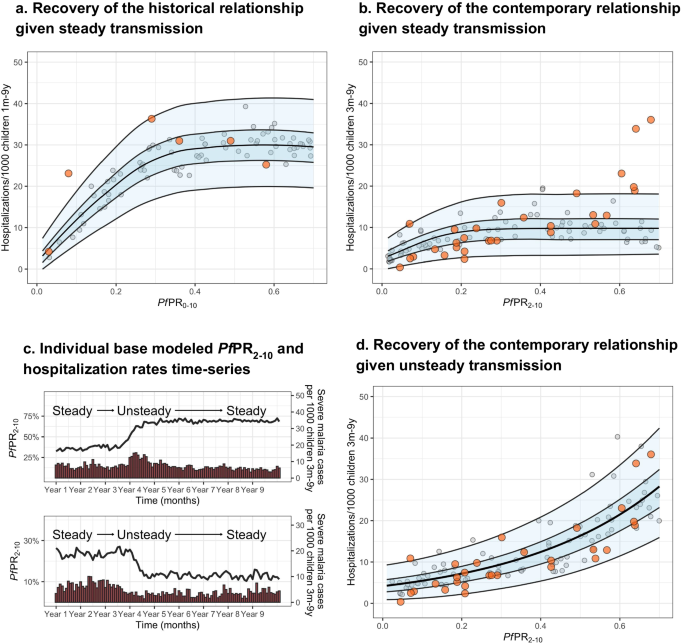
The historical dataset shows higher levels of hospitalization rates at similar prevalence, consistent with the expected reduction of comorbidities and improved management effectiveness in the contemporary dataset (Fig. 2 and Supplementary Note 5). Figure 2a, b shows (1) the historical (Fig. 2a) and contemporary (Fig. 2b) empirical estimates, (2) their respective time-frame-specific simulations under the assumption of steady exposure, and (3) the regression-based predicted relationship, shown as the median and 50% and 95% prediction intervals. For both the historical and the contemporary predictions, the log-logistic regression model provides a better fit to the model outputs, with the asymptote reaching around 60% and 40% PfPR2–10, respectively. However, while the prediction model based on steady transmission is consistent with the historical empirical data, it fails to recover the contemporary dataset relationship, with a substantial number of time-sites outlying from the predictions range, particularly for the highest ePf PR2–10 values (i.e., over 60%).
Showing the empirical PfPR2–10-hospitalization rates relationship obtained from a the historical dataset (orange dots), and b the contemporary dataset (orange dots) overlapping respective PfPR-hospitalization model-based estimates obtained through simulations consistent with steady transmission (gray dots, n = 100) and respective levels of health care access, treatment and comorbidities (b), and the best-fit model-based log-logistic regressions (median black line, blue ribbons 50% and 95% prediction intervals). c Representative simulation patterns of PfPR2–10 (black lines, increasing at the top and decreasing at the bottom) and subsequent malaria hospitalization incidence over time (red columns). d The empirical PfPR2–10-hospitalization rates relationship obtained from the contemporary dataset (orange dots) overlapping PfPR2–10-severity model-based estimates obtained through simulations scenarios consistent with time-varying exposure (gray dots, n = 100) and levels in health care access, treatment, and comorbidities, and the best-fit model-based log-linear regression (median black line, blue ribbons 50% and 95% prediction intervals).
Given that model predictions based on steady exposure do not capture the pattern of the empirical contemporary data, we further evaluated scenarios with unsteady past malaria transmission (either increasing or decreasing dynamics), and how these different trends affect the PfPR2–10-hospitalization rate incidence relationship. Specifically, we performed simulations that included step-up and step-down exposure dynamics with differences between pre- and intra-survey prevalence within the range of those observed empirically (see Methods). Simulations captured representative patterns of time-varying exposure, with decreasing, steady or increasing transmission before computing severe disease incidence (Fig. 2c) over the range of PfPR2–10 values. The best fit to a regression model is then obtained using the log-linear model (Fig. 2d). Based on performance metrics16, simulations under the assumption of unsteady patterns of past exposure predict the relationship of the contemporary dataset more accurately than those based on steady exposure. Further, modeled predictions under unsteady exposure show hospitalization rates in different age groups increase towards higher ePf PR2–10 in a similar way as observed in the empirical estimates (Fig. S2). However, this is opposite to the pattern in historical observations under steady state exposure; severe disease incidence among youngest children is typically higher in high transmission settings than in low transmission settings, whereas the opposite occurs among older children4,7,8,9. Consistent with these results, our model recovers more accurately the observed hospitalization age structure (Fig. S3, left column for representative time-sites) under the unsteady transmission assumption (Fig. S3, middle column) than under the steady-state assumption (Fig. S3, right column). Further, when assessing the model estimates of hospitalization risk later in time (i.e., allowing the scenarios to maintain a steady-state level transmission over 5 years), the prevalence-hospitalization rates relationship transitions to the asymptotic pattern expected for steady transmission (Fig. S4).
Discussion
Via scenario analysis, we have systematically evaluated the major clinical and epidemiological determinants influencing the occurrence of malaria hospitalization upon infection at the population level and thus proved a contemporary characterization of relationship trends and changes between malaria community prevalence and life-threatening disease risk in children. We found that the asymptotic relationship between prevalence and hospitalization disease risk, expected under a relatively steady transmission, is lost when children have been exposed to unstable, time-varying past malaria transmission. Overall, our analyses support the assumption that substantial fluctuations in malaria transmission over the years have led to a particular prevalence-hospitalization relationship observed among the East-African settings10, where increasing prevalence does not necessarily lead to saturating disease risk but increases toward the highest rates in an exponential manner. However, our analyses show that if transmission is further maintained at a steady-state level over sufficient time, disease risk would also eventually re-equilibrate back to the asymptotic relationship relative to the parasite rates (fig. S4). To date, inference frameworks aiming to estimate or predict severe outcomes of malaria used for policy decisions and public health action do not explicitly include past exposure as an independent variable5,17. Our analysis framework is capable of reconciling historical and contemporary observations encompassing three decades in sub-Saharan Africa and underscores the importance of taking the variability of past malaria exposure among children into account when predicting severe disease risk.
Our analyses have several limitations that need to be acknowledged. First, we use community-based hospitalization in non-urban settings as an empirical proxy of the incidence of severe outcomes of malaria. While these estimates could under- or over-estimate the true number of severe outcomes, the data was obtained aiming to standardized the under-ascertainment of cases, estimates would be affected by site specific treatment-seeking behaviors and therefore represent a lower limit for hospitalization rate at each time site. Also, the empirical contemporary dataset does not necessarily represent urban settings, where the referral pathways from infection to hospitalization might be more complex to understand or subject to other potential biases. Further, the curated data does not include cases where malaria was not the major syndrome for hospitalization. Our modeling approach allows access to health (i.e., access to diagnosis, treatment, and/or hospitalization) to randomly vary within the range of the rates estimated for the three countries, with sensitivity analysis showing that deviations from this assumption do not influence the overall relationship between prevalence and hospitalization. Nevertheless, if the data represents stronger deviations from these assumptions regarding case identification but remains relatively similar across time sites, the overall prevalence-severe disease trend will still hold. Second, the empirical PfPR estimates obtained through community and school surveys might not necessarily reflect the underlying prevalence dynamics for the full catchment population, given how heterogeneous malaria exposure can be at a very granular spatial level. However, we obtain a similar prevalence-hospitalization relationship using estimates computed using the geospatial model (see Section “Discussion”, Fig. S10), thus supporting the assumption of the empirical values being a representative summarizing value for the catchment populations. Also, the time series of PfPR values used to compute exposure steadiness can bear high uncertainty on the precise estimates. Nevertheless, given that we did not aim to replicate the prevalence changes over time but addressed this matter focusing on the relative change, our framework will remain well informed if the estimates approximate true trends. Third, our model OpenMalaria simulations are based on spatially homogeneous malaria transmission because the catchment populations in the empirical data are small. Assuming a heterogeneous transmission structure can affect the magnitude of the clinical outcomes, central estimates will not change18. Fourth, while parameterization of the hospitalization rates, efficacy of treatment, and comorbidities are consistent with the literature, for simplicity, we assumed similar ranges of values across time-sites with stochastic variation. In Supplementary Note 4, we provide an uncertainty analysis of these mechanistic parameters, showing that our results hold under no major deviations from tenable assumptions. Last, we have applied parametric regression models to simulation data, which likely misspecifies the mechanical interpretation of the model. Still, we believe this is justified given this approach was originally used to determine the empirical relationship10 and we aimed to replicate the trends under potential plausible mechanistic scenarios.
We have provided evidence that variation in malaria transmission and subsequent disease protection after life-long exposure can strongly influence severe disease risk estimates under otherwise equivalent ongoing force of transmission. Notably, frequent implementation and withdrawal of infection prevention strategies can strongly contribute to unsteady malaria exposure patterns and thus increase severe disease risk. Other potential sources of variability in the exposure include substantial movement of individuals from areas with different community prevalence (i.e., via increasing or reducing the overall population-level susceptibility to severe disease) or strong environmental changes influencing entomological inoculation rates such as urbanization or climatic drivers (i.e., prolonged drought or excessive rainfall).
Under constant, similar malaria exposure and health access rates, a population of children with higher immunity will substantially reduce their risk of severe malaria and, therefore, the number of severe cases. However, if malaria transmission has marked changes, either sudden reductions or increases, the resulting severe disease will be significantly lower or higher, respectively, than if the population had remained under constant transmission. This understanding is critical to evaluate the effects of interventions, and such mechanistic processes need to be included in future analytical approaches providing predictions of malaria disease burden. The processes that must be incorporated into disease burden estimates are best defined through differences in the age–structure patterns of the risk conditional to past exposure. For example, it is expected that following a strong reduction in malaria transmission, severe cases among age groups of children at a certain prevalence will be reduced earlier in time but will likely increase in later periods if malaria prevalence reaches steady levels. Similarly, the withdrawal of effective prevention and control strategies will lead to a higher number of severe cases than those expected when malaria prevalence has remained unchanged over time. In short, if past exposure and the dynamics described here are not accounted for in burden estimates, it will lead to long-term overestimation of severe malaria risk in places with recent effective interventions. And conversely, it will lead to long-term underestimation of severe malaria in places with deterioration of interventions. Finally, our findings underpin the need to build back rigorous clinical surveillance of severe malaria under the changing landscape of parasite exposure in Africa. It is striking that only two longitudinal clinical series exist since the launch of the Roll Back Malaria initiative in 200019,20.
Overall, our findings provide evidence that inference in malaria epidemiology, such as the generation of counterfactual scenarios with predictions on clinical outcomes for policy decisions, should account from now on past exposure and subsequent protection to avoid substantial bias in such risk predictions and highlight the increase in the complexity of malaria epidemiology arising from unsteady transmission dynamics.
Methods
Contemporary malaria hospitalization incidence data and paired community prevalence estimates
The contemporary P. falciparum malaria hospitalization incidence data has been obtained from 35 time-sites in Kenya (n = 18), Uganda (n = 14), and Tanzania (n = 3) between 2006 and 2020 and has been previously described elsewhere10. The data was collated from individual records of 21 hospitals, including hospitalized malaria cases in children resident in specific catchment areas within a 30 km range and excluding urban settings. Given potential differences in treatment-seeking behaviors at the different sites, the computed estimates represent the lower limit for hospitalization incidence, thus requiring further assumptions for adjusting to under ascertainment (see model parameterization in the Supplementary Text). for In the present analysis, cases were included if malaria was deemed the primary cause of hospitalization. Per each time-site, the number of hospitalizations among children 3 months to 9 years old per 1000 children per year was computed as a proxy of life-threatening disease incidence from the catchment population, obtained from census data and census data projections. Hospitalization data was paired with community surveys performed at the same periods of the hospital surveys for each time-site, adjusting for diagnostic accuracy (i.e., microscopy vs. rapid test) and standardized by computing the PfPR2–10 as described elsewhere21,22. Further details on hospitalization data, community prevalence, and estimates of hospital catchment population can be found in Supplementary Note 1.
Modeled community prevalence time-series
We assessed the past exposure dynamics using catchment site-specific time series of modeled age- and test-standardized parasite rates estimates, referred to as mPfPR2–1013,15. Modeled mPfPR2–10 estimates were explicitly obtained for each time-site catchment population using a geospatial model detailed elsewhere13,15, a Bayesian hierarchical geostatistical framework based on more than 180000 geo-coded empirical prevalence survey data points from East Africa, interpolated in time to 1 × 1 km resolutions using climatic and ecological covariates. For a set of sites (n = 11), annual mPfPR2–10 estimates are available since 2000, while for the rest (n = 15) available data begin in 2010. Time series of all the available mPfPR2–10 per site are shown in Fig. S1. Thus, for 27 out of the 35 present-day time sites, mPfPR2–10 time series included at least seven-time points of past annual estimates. Further, to estimate the gap between past and present transmission, we first computed the median value of the annual mPfPR2–10 time-series for each of the time-sites, under the assumption that it roughly represents the life-long transmission at which the surveyed population of children have been exposed in the previous years previous. This median mPfPR2–10 can then be compared to the empirical PfPR2–10 that is estimated at the time of surveying the malaria hospitalization incidence.
Historical malaria hospitalization incidence data and paired community prevalence estimates
As an alternative source of data, we analyzed a historical dataset obtained between 1992 and 1997, encompassing the relation between severe disease incidence measured as malaria hospitalization rates and the PfPR2–10 up to 70% and published elsewhere9. Similar inclusion and exclusion criteria had been used to obtain both datasets explicitly to allow comparison. Thus, comparable approaches to those used in the contemporary dataset were used to estimate malaria hospitalization incidence at six hospital time-site locations in The Gambia (n = 3), Kenya (n = 2), and Malawi (n = 1) and paired community prevalence estimates7,9,11. Further details can be found in Supplementary Note 1.
Agent-based model of malaria transmission, immunity, and disease dynamics
To recover the relationship between hospitalization rates and PfPR2–10, we used an individual-based model of P. falciparum malaria transmission and disease dynamics, OpenMalaria, previously described and calibrated elsewhere12. Briefly, OpenMalaria features within-host parasite dynamics, the progression of clinical disease, development of immunity, individual care-seeking behavior, vector exposure, and pharmaceutical and non-pharmaceutical antimalarial interventions at vector and human level (https://github.com/SwissTPH/openmalaria/wiki)14,23,24. The full model is calibrated to fit 23 parameters to 11 objectives representing different epidemiological outcomes, including age-specific prevalence and incidence patterns, age-specific mortality rates, and hospitalization rates, using a Bayesian optimization approach12. A detailed description of the model and references for the key technical details are provided in Supplementary Note 2.
Model parameterization on disease management, comorbidities, and health access
In order to compare model predictions to empirical data, we first parameterized several key inputs of the individual-based model to be consistent with both historical and contemporary datasets and the corresponding existing clinical and epidemiological knowledge, including different sets of variables addressing (a) the individual probability of malaria exposure per time-step to cover a range of PfPR2–10 up to 70%, (b) the effectiveness in malaria case management, including the rate of access of uncomplicated and severe malaria cases to health-care (i.e., rate of accurate diagnostic of true occurrence and subsequent timely treatment) and the efficacy of the available malaria drugs at each period (e.g., the efficacy of artemisinin derivatives combination therapies in clearing malaria), and (c) the co-occurrence of other diseases with influence on malaria that affect the severe progression of malaria across age-groups.
To evaluate the contemporary dataset, model parameterization for the main analysis was as follows: (1) PfPR2–10 estimates ranged up to 70%; (2) drug efficacy ranged between 85 and 100%25,26; (3) the rates of individuals suffering from malaria that required hospitalization who received diagnostic and treatment ranged from 60 to 90% while the rate of individuals with uncomplicated malaria accessing diagnostic and treatment ranged 20–60%27; and (4) co-occurrence of diseases contributing to malaria hospitalization was substantially reduced by 60–80% since the 1990s28,29,30. For (2–4), we parameterized the model by randomly sampling values from a uniform distribution defined by the respective ranges. Sensitivity analysis for these assumptions can be found in the Supplementary Note 3. To evaluate the historical dataset, we include the following: (1) PfPR2–10 estimates ranged up to 70% (2) first-line drug efficacy for uncomplicated malaria was negligible31; (3) access rates of malaria requiring hospitalization ranged from 40–60%8,32, and (4) co-occurrence of diseases contributing to malaria hospitalization approximated a hyperbolic decay distribution over age-groups8. Details on key model parameters and submodels are provided in Supplementary Note 3.
Time-varying malaria exposure on severity estimates
To evaluate how time-varying malaria exposure rates influence the ongoing PfPR2–10-hospitalization rates relationship, we produced a set of plausible malaria-transmission scenarios consistent with time-varying exposure as for those obtained from a Bayesian hierarchical geostatistical framework13,15 across all our time-sites. Particularly, we evaluated how a rapid reduction or increase of the PfPR2–10 level over 6 months (e.g., PfPR2–10 increasing from 10% to 70%) could affect the severe malaria incidence relative to a steady-state transmission assumption described before. This was performed by setting (1) the initial exposure rate (i.e., the individual probability of exposure to infectious bites pre-survey as a single rate over simulation time-steps), independent from (2) the final exposure rate (i.e., the probability of exposure during the survey period, also as a single rate over time steps). For simplicity, we set constant initial and final exposure rates. The relationship between the initial and final exposure rate was parameterized to reflect archetypical mPfPR2–10 patterns,—depicted in Fig. 1b—showing (1) a substantial increase in the mPfPR2–10 (e.g., Apac A), (2) relative constant mPfPR2–10 (e.g., Busia), and (3) substantial decrease in the PfPR2–10 (e.g., Jinja B). Thus, our definition of time-varying (unsteady) exposure comprises both substantial increasing and decreasing dynamics. For each time site with retrospective data encompassing at least 7 years, we computed the average mPfPR2–10 available up to 9 years prior to the date when the hospitalization data was available, used it as a proxy of the initial exposure rate, and computed the fold-change PfPR2–10. We then performed a local polynomial regression model to obtain predictions of the relationship between the final exposure rate and the corresponding relative change per time site. See fig. S5 in Supplementary depicting the relationship between the contemporary community prevalence as ePf PR2–10, and estimated relative change at survey computed from the median value of mPfPR2–10 of the past 7–9 years for each time-site. We then used these inputs of exposure to produce simulations using a combination of initial and final exposure rates to map a range of simulation-based PfPR2–10-hospitalization rates.
Scenario analysis to recover the empirical relationship
To evaluate under which scenarios OpenMalaria can recover the empirical prevalence-hospitalization, we implemented an iterative 4-step procedure to explore hypotheses of the impact of the determinants on disease risk and changes in disease risk—see sections above for details. The procedure is represented schematically in the Supplementary (Fig. S6). For each scenario analysis, we performed four iterative steps as follows:
-
1.
Using a high-performance computing framework (http://scicore.unibas.ch/) we performed 1000 population-level individual-based model simulations of malaria transmission at a steady-state (i.e., same entomological inoculation rate for each simulation) over long periods of time (i.e., over 90 years which ensures that lifelong malaria exposure has occurred all the generations evaluated prospectively); computing hospitalization rates among children 3 months- 9 years per 1000 persons-year across values of PfPR2–10 within the input range. In each of the simulations, we parameterized the model, mapping the range of values set up for the major epidemiological determinants described in the previous section, namely disease management (which includes rates and efficacy of diagnostic and treatment of severe and uncomplicated malaria) and co-occurrence of comorbidities. We set the parameters according to the empirical dataset we were evaluating (i.e., historical or contemporary). At the same time, we evaluated the model outcomes simulating steady and unsteady transmission.
-
2.
In order to assess how accurately the model simulations represent the empirical data, we evaluated the performance of two regression models to recover the prevalence-hospitalization relationship obtained via scenario analysis, namely a log-linear model and a log-logistic model. The approach was chosen to be consistent with the previous analysis framework of the contemporary dataset10, which analyses severe malaria syndrome-specific cases against prevalence. See Supplementary Note 3 for details on the regression models, model selection criteria, and computation of uncertainty estimates.
-
3.
We used the best-fit regression model among the above to evaluate how the modeling framework predicted the empirical ePf PR2–10-hospitalization incidence relationship. Specifically, we evaluated the accuracy of the model predictions using prediction performance metrics16 (see Supplementary Note 3 and Table S2).
-
4.
We updated model assumptions based on the evaluation above and reparametrized the scenario(/s) accordingly.
Evaluation of key assumptions for scenario modeling
To evaluate the robustness of the simulation-based predictions of the PfPR2–10-hospitalization relationship under time-varying exposure, we performed three major sensitivity analyses: (a) how increased or reduced rates of both uncomplicated case management and hospitalizations at the population level influence the severe disease incidence and prevalence relationship; (b) how the relationship changes over higher or lower drug efficacy estimates; (c) how changes on the incidence of comorbidities influence the severe disease risk. Details of the evaluation are provided in Supplementary Note 4 and Figs. S7 and S8.
The age structure of the severity estimates and the effect of time-varying malaria
Last, to assess if the model framework recovers hospitalization risk over different age groups, we compared both empirical and simulation-based estimates disaggregated by age. We performed the 4-steps iterative analysis described above for the contemporary dataset under the steady and time-varying transmission assumptions and evaluated the PfPR2–10-hospitalization relationship by age. More specifically, we computed hospitalization incidence over age groups at values of PfPR2–10 equal to those estimated in the for four representative time sites Apac A, Busia, Mubende B, and Jinja B. Further details on the age-structured analysis are provided in Supplementary Note 5.
Reporting summary
Further information on research design is available in the Nature Portfolio Reporting Summary linked to this article.
Data availability
Empirical contemporary data used in this analysis have been curated and uploaded to the Harvard Dataverse: https://dataverse.harvard.edu/dataset.xhtml?persistentId=doi:10.7910/DVN/XGDB3K. Correspondence and requests for materials should be addressed to the KEMRI Wellcome Data Governance Committee (dgc@kemri-wellcome.org). These data are available through a formal requesting process to the KEMRI Institutional Data Access/Ethics Committee. Guideline details can be found on the KEMRI Wellcome website: https://kemri-wellcome.org/about-us/#ChildVerticalTab_15.
Code availability
Model code, plotting code, and simulation data are available at https://github.com/PDeSalazarSwissTPH/SevereMalaria.
References
Snow, R. W. Sixty years trying to define the malaria burden in Africa: have we made any progress? BMC Med. 12, 227 (2014).
White, N. J., Day, N. P. J., Ashley, E. A., Smithuis, F. M. & Nosten, F. H. Have we really failed to roll back malaria? Lancet 399, 799–800 (2022).
Camponovo, F., Bever, C. A., Galactionova, K., Smith, T. & Penny, M. A. Incidence and admission rates for severe malaria and their impact on mortality in Africa. Malar. J. 16, 1 (2017).
Griffin, J. T. et al. Gradual acquisition of immunity to severe malaria with increasing exposure. Proc. Biol. Sci. 282, 20142657 (2015).
Weiss, D. J. et al. Mapping the global prevalence, incidence, and mortality of Plasmodium falciparum, 2000-17: a spatial and temporal modelling study. Lancet 394, 322–331 (2019).
Bhatt, S. et al. The effect of malaria control on Plasmodium falciparum in Africa between 2000 and 2015. Nature 526, 207–211 (2015).
Snow, R. & Marsh, K. The consequences of reducing transmission of Plasmodium falciparum in Africa. Adv. Parasitol. https://doi.org/10.1016/s0065-308x(02)52013-3 (2002).
Ross, A., Maire, N., Molineaux, L. & Smith, T. An epidemiologic model of severe morbidity and mortality caused by Plasmodium falciparum. Am. J. Trop. Med. Hyg. 75, 63–73 (2006).
Marsh, K. & Snow, R. W. Malaria transmission and morbidity. Parassitologia 41, 241–246 (1999).
Paton, R. S. et al. Malaria infection and severe disease risks in Africa. Science 373, 926–931 (2021).
Snow, R. W. et al. Relation between severe malaria morbidity in children and level of Plasmodium falciparum transmission in Africa. The Lancet https://doi.org/10.1016/s0140-6736(97)02038-2 (1997).
Reiker, T. et al. Emulator-based Bayesian optimization for efficient multi-objective calibration of an individual-based model of malaria. Nat. Commun. 12, 7212 (2021).
Kamau, A. et al. Malaria hospitalisation in East Africa: age, phenotype and transmission intensity. BMC Med. 20, 28 (2022).
Smith, T. et al. Mathematical modeling of the impact of malaria vaccines on the clinical epidemiology and natural history of Plasmodium falciparum malaria: overview. Am. J. Trop. Med. Hyg. 75, 1–10 (2006).
Alegana, V. A. et al. Plasmodium falciparum parasite prevalence in East Africa: Updating data for malaria stratification. PLOS Global Public Health https://doi.org/10.1371/journal.pgph.0000014 (2021).
Dziak, J. J., Coffman, D. L., Lanza, S. T., Li, R. & Jermiin, L. S. Sensitivity and specificity of information criteria. Brief. Bioinform. 21, 553–565 (2020).
World malaria report. https://www.who.int/teams/global-malaria-programme/reports/world-malaria-report-2023 (2023).
Penny, M. A. et al. Public health impact and cost-effectiveness of the RTS,S/AS01 malaria vaccine: a systematic comparison of predictions from four mathematical models. Lancet 387, 367–375 (2016).
Njuguna, P. et al. Observational study: 27 years of severe malaria surveillance in Kilifi, Kenya. BMC Med. 17, 124 (2019).
Guinovart, C. et al. The epidemiology of severe malaria at Manhiça District Hospital, Mozambique: a retrospective analysis of 20 years of malaria admissions surveillance data. Lancet Glob. Health 10, e873–e881 (2022).
Smith, D. L., Guerra, C. A., Snow, R. W. & Hay, S. I. Standardizing estimates of the Plasmodium falciparum parasite rate. Malar. J. 6, 1–10 (2007).
Mappin, B. et al. Standardizing Plasmodium falciparum infection prevalence measured via microscopy versus rapid diagnostic test. Malar. J. 14, 460 (2015).
Smith, T. et al. Towards a comprehensive simulation model of malaria epidemiology and control. Parasitology 135, 1507–1516 (2008).
Smith, T. et al. Ensemble modeling of the likely public health impact of a pre-erythrocytic malaria vaccine. PLoS Med. 9, e1001157 (2012).
World Health Organization. Guidelines for the Treatment of Malaria. (World Health Organization, 2010).
World Health Organization. Guidelines for the Treatment of Malaria. Third Edition. (World Health Organization, 2015).
The DHS Program. https://dhsprogram.com/methodology/survey-types/mis.cfm.
GBD 2016 Causes of Death Collaborators. Global, regional, and national age-sex specific mortality for 264 causes of death, 1980-2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet 390, 1151–1210 (2017).
Reiner, R. C. et al. Identifying residual hotspots and mapping lower respiratory infection morbidity and mortality in African children from 2000 to 2017. Nat. Microbiol. 4, 2310–2318 (2019).
Reiner, R. C. Jr et al. Variation in childhood diarrheal morbidity and mortality in Africa, 2000-2015. N. Engl. J. Med. 379, 1128–1138 (2018).
Amin, A. A. et al. The challenges of changing national malaria drug policy to artemisinin-based combinations in Kenya. Malar. J. 6, 72 (2007).
Goodman, C. A., Coleman, P. G. & Mills, A. Economic analysis of malaria control in sub-Saharan Africa. (Global Forum for Health Research, Geneva, 2000).
Acknowledgements
Calculations were performed at sciCORE (http://scicore.unibas.ch/) scientific computing center at the University of Basel. Funding: This study was partly funded by Bill & Melinda Gates Foundation (INV- 025569 to MAP) supporting M.A.P. and P.M.S. M.A.P. also received support via a Swiss National Science Foundation Professorship (PP00P3_203450 to M.A.P.); R.W.S. is supported under a Wellcome Trust Principal Research Fellowship (212176/Z/18/Z), which also provided support for A.K.; R.W.S., A.K. and S.A. are grateful for the support from the Wellcome Trust to the Core Award for the East Africa Major Overseas Program (203077/Z/16/Z). S.A. was supported by the CDC Foundation through funding from the World Health Organization for the RTS,S evaluation (project requisition number 2018/854999).
Author information
Authors and Affiliations
Contributions
Conceptualization: P.M.S., M.A.P., A.K., R.W.S.; methodology: P.M.S., M.A.P., R.W.S.; investigation: P.M.S., S.A., A.M., A.K., A.C., R.W.S., M.A.P.; visualization: P.M.S., M.A.P.; funding acquisition: M.A.P., R.W.S.; writing—original draft: P.M.S., M.A.P., R.W.S.; writing—review & editing: P.M.S., M.A.P., R.W.S., A.K., A.C., S.A., A.M.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics declaration
Kenya hospital surveillance: Kenya Medical Research Institute/ Scientific and Ethics Review Unit (KEMRI SERU) IRB numbers 1433, 3057, 3149; 1801, 2558, 2465, 3459, and 3771; Uganda hospital surveillance approved by the CDC as public health surveillance/non-research (NCEZID 031416), Tanzania hospital surveillance approved by the ethics committees of the National Institute for Medical Research, Tanzania, and the London School of Hygiene and Tropical Medicine. Kenya community parasite surveys KEMRI SERU IRB numbers 3149, 3592, 1801, 2558, 2675, 2801, and 3822; Uganda community prevalence surveys Vector Control Division Research Ethics Committee, MoH, Kampala: VCDREC/117.
Peer review
Peer review information
Nature Communications thanks the anonymous reviewers for their contribution to the peer review of this work. A peer review file is available.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
De Salazar, P.M., Kamau, A., Cavelan, A. et al. Severe outcomes of malaria in children under time-varying exposure. Nat Commun 15, 4069 (2024). https://doi.org/10.1038/s41467-024-48191-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41467-024-48191-7
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.