About three decades ago a British epidemiologist named David P. Strachan proposed a simple, if counterintuitive, idea to explain why hay fever, eczema and asthma had become increasingly common over the preceding century. Strachan linked rising rates of these allergic illnesses in the U.K. with improvements in living standards since the industrial revolution—in particular, a sharp drop in the number of infections experienced in early childhood. He surmised that exposure to bacteria and viruses in the first years of life (provided an infant survived them) somehow protected against these conditions showing up later.
Although Strachan’s original hunch, now commonly known as the hygiene hypothesis, concerned allergic disorders, researchers have since used its basic tenet—exposure, or lack thereof, to environmental influences—to explain historical increases in various other conditions as well. These include poliomyelitis, multiple sclerosis and type 1 diabetes. Numerous epidemiological surveys have revealed certain escalating disease patterns as industrialization spread from Europe to North America and beyond. Wherever the rate of childhood infections (and mortality) fell, the incidence of several previously rare illnesses started to rise—albeit not uniformly and not all at once.
Major polio outbreaks first began to appear in the late 1800s. The incidence of multiple sclerosis, in which the immune system attacks the protective covering around particular nerve cells, doubled in certain parts of the world in the second half of the 20th century. Type 1 diabetes, which occurs when the body mistakenly destroys cells in the pancreas that make the hormone insulin (which enables the body to use glucose for energy), started creeping up in the first half of the 1900s and rose dramatically in the 1950s.
On supporting science journalism
If you're enjoying this article, consider supporting our award-winning journalism by subscribing. By purchasing a subscription you are helping to ensure the future of impactful stories about the discoveries and ideas shaping our world today.
Exactly how early exposure to various viruses or bacteria can protect against the emergence of a number of seemingly unrelated illnesses remains unclear. Somehow the infections enable the developing body to learn how to deal with pathogens. Further, the absence of exposure to these microbes can prompt the body to attack itself. In particular, a substantial collection of research implicates a fairly large group of pathogens called enteroviruses in the surge of polio and type 1 diabetes.
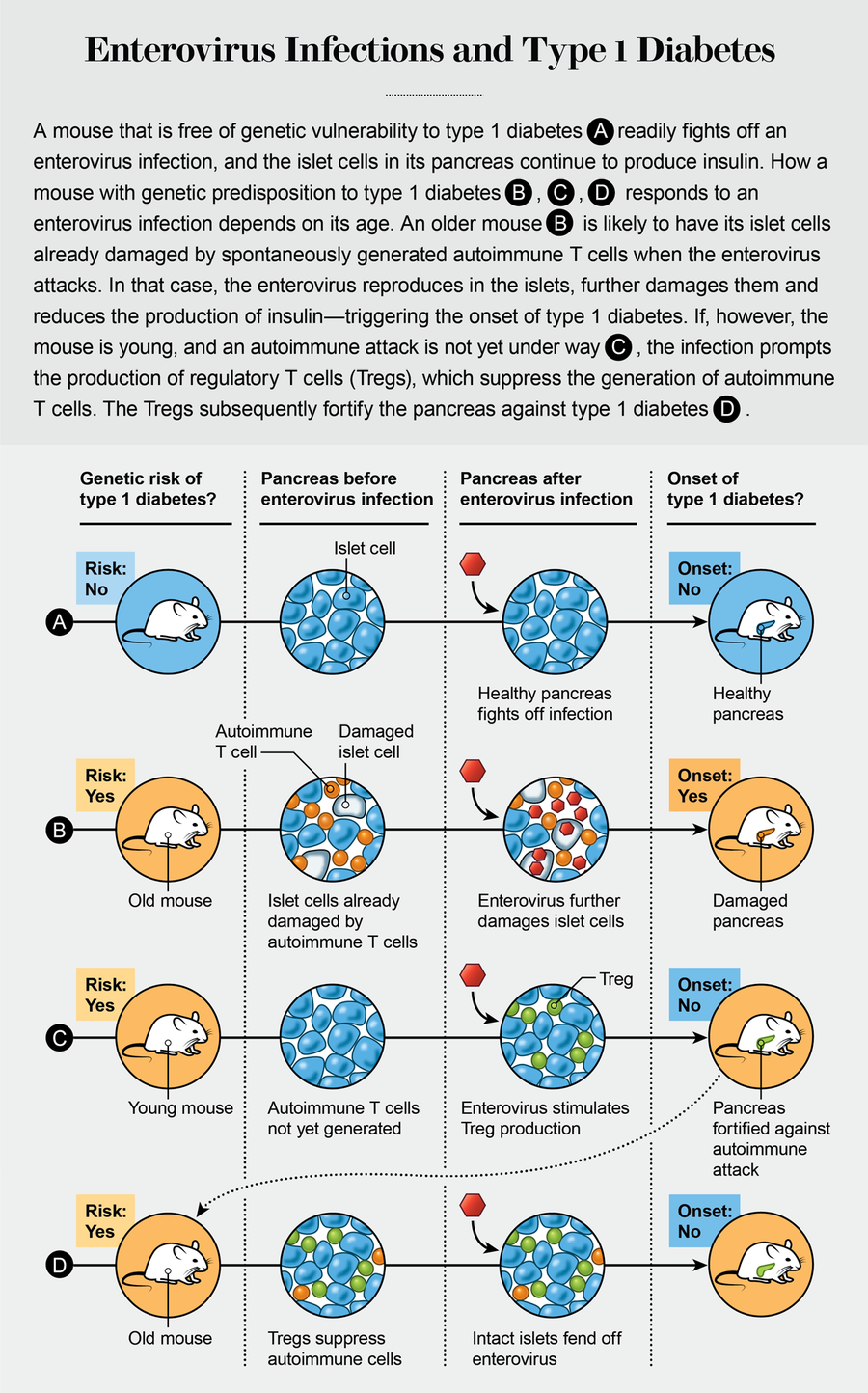
Unlike the far more common type 2 diabetes—often tied to weight gain in adulthood—type 1 diabetes usually strikes before the age of 20. Our experiments on mice that are prone to spontaneously acquiring type 1 diabetes have revealed a complex mechanism whereby the same strains of enteroviruses can either prevent or instigate the illness, depending on the age of the mouse when it is infected. Assuming our results are confirmed in humans, a vaccine based on a group of viruses commonly excreted in feces could potentially prevent type 1 diabetes in many individuals.
A Century of Clues
Our research began with a fundamental question, similar to the one Strachan had addressed: Why was type 1 diabetes so rare in the past and yet a scourge by the 1950s? In ancient times, Greek, Arab, Indian and Chinese physicians all described a rare cluster of symptoms—including rapid weight loss, abnormal thirst and urine that tasted sweet when sampled—that were almost certainly an outcome of type 1 diabetes. Extrapolating from individual hospital data, researchers calculate that about one or two in every 100,000 children under the age of 15 developed type 1 diabetes in the early 1900s. Today that number is closer to 20 per 100,000 children in parts of the U.S. and more than 60 per 100,000 in Finland. Disturbingly, these numbers continue to rise.
The increase has not been steady, however. After years of just creeping up in some countries, type 1 diabetes began to soar in the middle of the 20th century. Since then, epidemiologists have calculated an average annual increase of between 3 and 5 percent across the globe. Between 1998 and 2010 the incidence of type 1 diabetes jumped by a shocking 40 percent.
Such a steep rise in such a short time told us that we were not looking at a fundamental change in the human gene pool: DNA does not mutate that rapidly. A variety of different combinations of many genes profoundly increase the risk of an individual acquiring type 1 diabetes. As far as investigators can tell, however, the prevalence of these high-risk genetic profiles has not changed. Instead more and more people with a relatively low genetic predisposition to type 1 diabetes are now suffering from the ailment. Few cases can be linked solely to a genetic disorder. These and other findings, from scientists around the world, strongly suggest that newly emergent environmental factors must be at work.
Various possibilities have been considered over the years—and dismissed. Unlike type 2 diabetes, type 1 cannot be brought on by a person’s diet or other health-related habits. More intriguingly, several studies have determined that type 1 diabetes occurs more frequently the farther away one gets from the equator. Might a lack of vitamin D, which is easily produced by the body whenever it is in sunlight, account for such regional variation? That idea soon fell apart, however. Epidemiologists discovered, for instance, that some countries in the far north, such as Finland, had higher rates of type 1 diabetes in regions with more sunlight than in regions with less.
The bulk of the evidence points instead to a viral trigger—probably one or more viruses that occur in sewage or in contaminated drinking water. Numerous studies indicate that enteroviruses—so named because they are normally found in the intestine (énteron in ancient Greek)—are the culprits. (Indeed, no substantive data link any other kind of viral or environmental influences to the disease.) Some enteroviruses are able to replicate in the pancreas, inflaming areas adjacent to where the islet cells, which produce insulin, reside. The inflamed regions produce autoimmune T cells. In normal circumstances, our T cells protect the body against invaders. Autoimmune T cells, however, attack the body’s own islet cells, destroying their ability to produce insulin and thereby bringing on diabetes.
Researchers have counted more than 100 types of enteroviruses. No single type of enterovirus, however, seems solely responsible for detonating diabetes around the world. Rather scientists have identified a number of candidates, chief among them six enteroviruses called the Coxsackie B viruses, implicated in the precipitation of the ailment. And they do not understand exactly how such infections might provoke the body to attack itself. The process must be complex: epidemiological studies indicate that specific enteroviruses that appear to advance the disorder in some people apparently protect others from developing it in the first place.
Credit: Amanda Montañez
Dirty Water
As we evaluated the kinds of experiments that could potentially identify diabetes-causing enteroviruses, we sought clues in a different illness: polio. An often paralyzing childhood affliction, polio is caused by another class of enteroviruses, called polioviruses. These viruses seem to have been around for millennia: an ancient Egyptian stele (a relief carved in a stone slab), now in a Copenhagen museum, appears to depict a polio patient. The terrible condition they engender used to be quite rare, however, until the late 19th century, when sporadic and then annual epidemics suddenly began to occur. Polio killed tens of thousands of children and crippled millions more in the 20th century. As recently as 1988, polio crippled about 1,000 children a day. Thanks to a massive vaccination campaign, polio is now endemic in only two countries.
The hygiene hypothesis helps to explain this sudden surge in polio cases. It is easy to forget that many conveniences of contemporary life in the developed world are only about a century old. Before the widespread installation of municipal water supplies in Europe and North America, people drew water from wells, ponds or public fountains for all purposes, including drinking, bathing and washing clothes. Unsurprisingly, drinking water was often contaminated with human or animal waste. The paucity of running water and soap also meant that people could not be as strict about keeping their hands clean after going to the bathroom as they can be today. Consequently, the simple act of preparing a meal or shaking hands could spread germs far and wide.
Thus, nearly everyone, from early life onward, was exposed to polioviruses that had been passed into the environment from human feces. Newborns did not tend to develop the illness, however, because their mothers had developed immunity against the viruses and passed on protective antibodies to both the developing fetuses during pregnancy and the babies during nursing. As infants grew older and stopped nursing, and as maternal antibodies waned, young children began to make their own protective antibodies against the virus because of repeated exposures to it. So although polioviruses were almost ubiquitous, polio itself was uncommon because youngsters were first protected by the mothers’ antibodies and were subsequently protected by their own immune system.
This chain of protection, a part of human life for eons, began to break as human populations entered a “cleaner” world. A boy who might have been spared exposure to polioviruses could encounter them later in life, when he had no protective immunity. Such a chance encounter with poliovirus could then lead to paralytic polio—once in every 100 to 200 poliovirus infections. That is probably why President Franklin D. Roosevelt, for example, developed paralytic polio at the age of 39 while on vacation on an island in New Brunswick, Canada.
Despite polio’s grim legacy, we took some consolation from the fact that a vaccine for the viral infection that causes it had proved safe and immensely effective. If researchers can make a vaccine against one type of enterovirus, they should be able to make vaccines against others as well. And if experiments prove that enteroviruses cause type 1 diabetes, the discovery might point to a potential new treatment: namely, a vaccine against type 1 diabetes that would protect those at greatest risk from acquiring the viral infection in the first place.
(We can rule out poliovirus as a cause of type 1 diabetes. Although polio epidemics became commonplace in the 20th century, no parallel outbreaks of type 1 diabetes were observed. In addition, polio has been eradicated from countries where the incidence of type 1 diabetes continues to rise.)
To show that a virus causes a particular disease, one should begin by isolating the virus from the affected tissue. For type 1 diabetes, that is the pancreas. But safely sampling tissues from a human pancreas remains a surgical challenge—which is why such biopsies are seldom performed on people who are otherwise healthy. Furthermore, pinning down the exact moment when the body’s immune system starts attacking the pancreas and destroying the insulin-producing islet cells is extremely difficult. By the time it becomes clear that someone has type 1 diabetes, any signs of what may have been an active infection have usually disappeared.
Nevertheless, about 40 published reports convincingly link the presence of various enteroviruses to the onset of type 1 diabetes: either the virus or its genetic material was isolated from patients’ postmortem pancreatic tissues. And other studies have shown that some kind of enterovirus infection most likely plays a long-term role in the development of type 1 diabetes.
As it happens, a particular mouse strain, known as the nonobese diabetic (NOD) mouse, acquires type 1 diabetes on its own, without any intervention from investigators. (Curiously, NOD mice maintained in hygienic conditions acquire the disease much faster than those in dirty cages.) We hypothesized that NOD mice resemble humans with a genetic predisposition to type 1 diabetes. Furthermore, unlike most enteroviruses, the Coxsackie B viruses replicate well in mice and had already been linked to type 1 diabetes. All these factors made NOD mice the ideal model for exploring the relation between enteroviruses and type 1 diabetes.
In 2002 we deliberately infected very young NOD mice, otherwise held in sterile environments, with Coxsackie B viruses. We found that the animals were much less likely to develop type 1 diabetes as they aged, compared with uninfected control subjects. These results supported the hypothesis that early exposure to microbes offers a protective effect against developing type 1 diabetes. Intriguingly, that effect was not limited to specific types of Coxsackie B viruses, although some seemed to provide stronger protection than others. Experiments by virologist Heikki Hyöty of Tampere University in Finland and his colleagues have yielded similar outcomes.
We can think of three possible mechanisms by which exposure to enteroviruses when young might prevent the damaging impact of such infections later in life. First, an infection could trigger the development of protective antibodies against that specific type of enterovirus, so subsequent exposure to the same type would not result in disease. (This process mirrors the principle behind the poliovirus vaccines and many other viral vaccines we use today.) Second, because the Coxsackie B viruses are very similar, on a molecular level, to other enteroviruses, they may prompt the body to more rapidly mobilize adequate defenses, even to enteroviruses it has never encountered before. Third, an enterovirus infection may stimulate the production of regulatory immune cells called Tregs. These generally beneficial cells serve as a conscientious police force, suppressing autoimmune T cells that would otherwise harm the host.
To tease apart these diverse mechanisms, we decided to infect the mice at different ages and observe them for at least 30 weeks after the inoculation. After many years of experimentation, we discovered that infecting older NOD mice with Coxsackie B viruses increased, rather than decreased, their likelihood of developing type 1 diabetes. This finding contrasted sharply with what we had observed in young NOD mice.
We concluded that the pancreas had to be already inflamed—meaning that the insulin-producing islet cells had to be under attack by the mouse’s own autoimmune T cells to begin with—for an enterovirus to enter the islets and multiply, accelerating the onset of diabetes. In other words, a genetically induced autoimmune attack on the pancreas had to be underway before a Coxsackie B virus infection could hasten the onset of type 1 diabetes. The older the mouse and the worse the inflammation, the faster the illness would take hold—often resulting in full-blown diabetes in a day or two. (In contrast, older mice held in sterile environments developed diabetes weeks later.)
Studies by immunologist Matthias von Herrath of the La Jolla Institute for Immunology in California and his colleagues indicated that enterovirus infections early in life (before an autoimmune attack is launched) can stimulate the production of regulatory T cells, which persist into adulthood. The Tregs suppress the production of autoimmune T cells and thereby protect against type 1 diabetes. But if the pancreas is already inflamed with autoimmune T cells—as would naturally happen in older NOD mice—the virus is able to replicate, damaging the insulin-producing islet cells and precipitating diabetes. In other words, enteroviruses can either protect against or trigger type 1 diabetes in NOD mice, depending on the age at which the infection occurs.
Diabetes Vaccines
Assuming these observations in NOD mice reflect what occurs in humans with a genetic predisposition to type 1 diabetes, how might we exploit them to help such vulnerable individuals? Nobody wishes to return to the days of poor or no hygienic practices. But we should not have to. Based on our experience with poliovirus vaccines, we know that developing safe and effective enterovirus vaccines is feasible.
Generally, antiviral vaccines come in three versions: live but attenuated, killed and subunit. Live, attenuated vaccines were originally generated by passing the virus through cells or an animal host to weaken its ability to cause disease. Such vaccines are regarded as the most proficient at inducing immunity because the viruses replicate in the host and induce a normal immune response. But they can mutate rapidly into a pathogenic strain. Genetic engineering now enables specific areas of a virus’s genome to be altered or deleted to limit the likelihood of such reversion, but the risk remains. Killed vaccines inactivate viruses so that they cannot multiply, but they still induce a certain level of immunity in the host. Because the virus does not persist in the body, however, periodic revaccination is usually required. A subunit vaccine uses one or more parts of a virus that are known to stimulate an immune response to produce the desired type of immunity in the person vaccinated. In 2021 mRNA-based vaccines against SARS-CoV-2 were deployed to fight the COVID pandemic and showed excellent results, inducing protective immunity in those vaccinated. Given such success, this technology will, in the near future, be readily adapted to other vaccine targets such as human enteroviruses to prevent infections, as well as to potentially prevent type 1 diabetes.
The bulk of the evidence indicates that no single enterovirus or even a few enteroviruses are involved in the onset of type 1 diabetes throughout the world. Furthermore, the historical evidence indicates that type 1 diabetes was rare when exposure to numerous enteroviruses was a fact of life. We hypothesize, therefore, that vaccination with multiple types of enteroviruses should offer the most protection. Such an approach would simulate the way humans used to accumulate protective immunity to enteroviruses throughout history. The initial vaccine could be a killed-virus one for safely inducing immunity. Thereafter, either inactivated or highly attenuated vaccines could be used as booster doses.
We find it encouraging that a vaccine approach against type 1 diabetes is finally underway. Hyöty’s group is working with Finnish biopharma Vactech Oy, for which Hyöty is chair of the board, to develop a vaccine against a single type of Coxsackie B virus and has tested its ability to prevent type 1 diabetes in mice. Phase 1 clinical trials of this killed-virus vaccine in humans began in 2021. Testing it in children—to ensure safety, generation of a protective immune response to the enterovirus and protection from type 1 diabetes—will take upward of a decade. Given that numerous observations suggest that no single strain of enterovirus is involved with type 1 diabetes, we can only remain hopeful that this vaccine will significantly lower the incidence of the disease.
In addition, a remarkable variety of efforts are in the works to reverse type 1 diabetes after its onset. Investigator Paolo Fiorina of Boston Children’s Hospital and his colleagues have demonstrated that appropriately manipulated stem cells, when infused into mice, can sometimes reverse type 1 diabetes. Another group, led by Denise Faustman of the Massachusetts General Hospital Immunobiology Laboratory, is investigating the efficacy of the bacillus Calmette-Guérin (BCG) vaccine, normally used to prevent tuberculosis, in undoing the effects of type 1 diabetes. Several research groups in the U.S. and the U.K. have focused on immunization with proinsulin (a precursor of insulin) or the DNA that encodes for it. In particular, a 2017 report from a multi-investigator effort by Mark Peakman of King’s College London and his colleagues indicates that a protein fragment from proinsulin can induce beneficial responses in people newly diagnosed with type 1 diabetes.
Doctors in the U.S. alone diagnose 64,000 new cases of type 1 diabetes every year. We need to remember that a vaccine cannot entirely eradicate the disease: some cases seem to occur solely because of the patient’s genetic makeup. Refining treatments to improve the quality of life for individuals who can no longer make their own insulin remains important. Even if only a small fraction of participants in vaccine trials are protected from the disease, however, a significant number of people will have better lives. Given how fast the incidence of type 1 diabetes is increasing, the ability to make it as rare as it once was could benefit millions.
