Abstract
Objectives:
To assess pain relieving effects of an intensive exercise programme on a seated double-poling ergometer in individuals with spinal cord injury (SCI).
Setting:
Stockholm, Sweden.
Methods:
A total of 13 wheelchair-dependent individuals with a thoracic or lumbar SCI were recruited to a 10-week training period (three times weekly) assessing the effects of regular training on upper-body strength, aerobic and mechanical power, and crossover effects on functional performance, as well as cardiovascular risk factors. Eight of the participants reported pain and were included in this exploratory pain protocol and assessed using the International SCI Basic Pain Data set, the Wheelchair Users’ Shoulder Pain Index and International SCI Quality of Life Basic Data set.
Results:
For those with neuropathic pain, median pain intensity ratings decreased from 5 on a 0–10 numerical rating scale at base-line to 3 at the end of study, and four of seven participants reported an improvement on the Patient Global Impression of Change scale. For those with musculoskeletal pain (n=5), median pain intensity ratings improved from 4 at baseline to 0 at the end of study. All but one rated no musculoskeletal pain at all at the end of study and number of days with pain per week decreased from 5.5 to 0.7. None of the participants developed pain, because of overuse during the training period and few reported unwanted side effects.
Conclusion:
Considering its promising effects and safety, an intensive exercise programme can be tried for treating musculoskeletal pain and also neuropathic pain following SCI.
Similar content being viewed by others
Introduction
Pain following spinal cord injury (SCI) is a common consequence, with a high incidence of both musculoskeletal and neuropathic pain.1 Treatment of long-lasting pain, especially of neuropathic origin, is difficult with limited effects on intensity reduction. Mainly pharmacological treatments are recommended,2 but have limited efficacy and are often associated with adverse events, which limit compliance. Patient preference is for the non-pharmacological treatments3 for which reason it is important to study alternatives to drug treatment.
A large controlled study on the effects of an exercise/movement intervention for SCI-related shoulder pain4 reported significant improvements in pain as assessed with a single-item visual analogue scale and using the Wheelchair User's Shoulder Pain Index (WUSPI). Similar positive findings have been reported earlier in studies assessing the effects of different exercise programmes for SCI-related shoulder pain.5, 6, 7 The effects of exercise on overall pain (non-specified type or duration) have been assessed in two studies,8, 9 where small reductions in pain intensity ratings were reported.
No study has to our knowledge assessed the effects of an exercise programme on any type of neuropathic pain. However, a few rodent studies have reported effects of treadmill training and swimming10, 11, 12 in neuropathic pain of central and peripheral origin where signs of neuropathic pain were reduced after the training period. These studies concluded that exercise is helpful for neuropathic pain.
The present report is part of a larger study assessing the effects of regular training on upper-body strength, aerobic and mechanical power, and crossover effects on functional performance as well as cardiovascular risk factors in individuals, with SCI using a seated double-poling ergometer.13 The aim of this exploratory study was to assess the effects of intense regular exercise on both nociceptive and neuropathic pain in those individuals presenting with pain.
Methods
Study design
In all, 13 wheelchair-dependent individuals with thoracic or lumbar injury (paraplegia since more than 2 years) were recruited from a patients’ organisation. Participants were to be between 18 and 70 years of age without diagnosed cardiovascular or lung disease or other diseases (including cognitive impairments) interfering with an intensive training programme. Thirteen persons with an SCI, eight males and five females with a mean age of 47 years (s.d. 12.3), and an injury ranging from T5 to L1 were included in the study, which was approved by the Stockholm Regional Ethics Board. We certify that all applicable institutional and governmental regulations concerning the ethical use of human volunteers were followed during this research.
A custom-built seated double-poling ergometer modified for persons with motor impairments in the lower extremities was used in the study. Subjects trained on the double-poling ergometer three times per week during a 10-week period, in small supervised groups. Each session lasted ∼50 min and included a warm-up, four intervals of 6–7 min, followed by a cool-down. The intervals varied between 15 s–3 min with 15 s–1 min rest. The intensity of the intervals was determined to lead up to 70–100% of peak heart rate obtained during the initial maximal oxygen uptake test. If a higher peak heart rate was detected during training, the level of intensity was adjusted. Heart rate was measured with a standard heart rate watch (Polar RS 400, Electro OY, Finland). The intensity in this study was somewhat higher than previously recommended (50–80% maximum heart rate14). A total of 70–100% peak heart rate was used not only to optimise oxygen uptake training, but also to influence upper body strength by implementing a protocol in which participants were required to perform short, intensive double-poling intervals for 15 s, which corresponded to 8–15 poling cycles. These short intervals were alternated with longer intervals of 1 to 3 min with the purpose of increasing aerobic capacity.
During the first two weeks, subjects were taught double-poling technique and introduced to interval training. After the familiarisation the training intensity were progressively increased during the training period and a new programme was introduced every second week. The peak heart rate, distance and average intensity in each session were documented for each training session (a more detailed description of the exercise programme is found in Lindberg et al.15).
Pain protocol
Of the 13 individuals included in the double-poling ergometer study, 8 (62%) reported pain meeting the basic pain data set criteria (pain present one or more days during the previous seven) and were thus included in the pain protocol.
For assessing and classifying pain the International SCI Basic Pain Data set (ISCIPDS:B), was used.16 In this data set the three worst pain locations are described in detail, for example, localisation, type of pain, pain intensity (rated on a 0–10 numerical rating scale (NRS)), onset, temporal pattern and number of days with pain. The data set also comprises six pain interference items rated on a 0–6 NRS. Further the International SCI Quality of Life Basic Data set version 1.017 was included in the pain protocol. This Quality of Life (QoL) data set consists of three questions rated on a 0–10 NRS. At the end of study, the global pain-relieving effect was rated using the Patient Global Impression of Change scale (PGIC).18 The total pain relieving effect on all pain components as well as the effect on the neuropathic pain component(s) was rated using the PGIC. The WUSPI19 was used for assessing pain from the shoulder girdle in activity where 15 items are rated on a 0–10 visual analogue scale and summarised for total WUSPI score.
Participants in this study were assessed before starting the training programme and immediately after completion.
Statistics
This part of the original study was carried out as an exploratory study. The results are presented using descriptive statistics with numbers of observations presented together with median values and interquartile ranges (IQR) for categorical data and using mean and s.d. for numerical data. The exception is the WUSPI where visual analogue scale ratings are presented as mean values together with s.d. in line with original instructions.19
Results
Participants
Of the eight individuals included in the pain protocol, six were males and two females, mean age 50.5 years (s.d. 11, range 30–67) with mean time since injury of 17.8 years (s.d. 7.6, range 7–29). For more demographic data see Table 1.
The participants had a mean of 2.1 pain locations each. In the seven with neuropathic pain, 10 different pain locations were included and assessed. Seven of these were below the neurological level of lesion, and three at the neurological level of lesion. Most neuropathic pain problems started at the time of the injury (n=8), but in one participant it started five years post-injury and in one the duration was unknown (‘for many years’). Pain was either intermittent including paroxysms (n=4) or constant/continuous (n=6).
In the five participants with nociceptive musculoskeletal pain, six pain locations were included. The duration of their pain ranged from 8months to more than 10years, with unknown onset in one participant. The temporal pattern of pain was related to movement (n=3), lasted between one and 24 h (n=1) or was constant/continuous (n=2). Pain was localised to the shoulder girdle area in all five individuals, and in neck (n=1), elbow (n=2), forearm (n=2), wrist (n=2) and hand/fingers (n=1).
One patient had experienced nociceptive visceral pain located in the abdomen for many years. This was described as constant/continuous daily pain.
Of those individuals not included in the pain protocol, three reported intermittent musculoskeletal pain. These individuals were not included because their reports of pain were not covered by the inclusion criteria (pain during the previous 7 days). One of the three had recurrent low-back pain radiating into the legs, one recurrent ischial pain and pain from shoulders once or twice a month, and one recurrent shoulder pain when playing basketball.
Three participants were on analgesic drugs at baseline (opioids, n=2; nonsteroidal anti-inflammatory drugs, n=1) and one at the end of study (opioids).
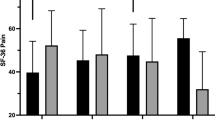
Pain intensity—neuropathic pain
Seven individuals reported in total 10 locations classified as neuropathic pain. Median intensity during the previous 7 days was 5 (range 1–7) on a 0–10 NRS at base-line and 3 (range 0–7) at the end of study (Figure 1). Number of days with pain was unaffected with a mean of 5.8 days (range 2–7 at baseline and 0–7 at the end of study). Six of the ten pain locations (in four of the seven individuals) reportedly decreased ⩾1.8 units (Figure 1).
Of the locations where pain was reported to decrease, five (of seven) were below the level of lesion and one (out of three) at the level of lesion.
Pain intensity—nociceptive pain
Five individuals were classified as having nociceptive musculoskeletal pain at six pain locations and one had nociceptive visceral pain. Median intensity ratings in those with musculoskeletal pain decreased from 4 at baseline (range 2–7) to 0 at the end of study (range 0–4). All but one participant rated no pain at all and one improved 2 units on the 0–10 NRS, Figure 2. Number of days with pain decreased from 5.5 (range 2–7) to 0.7 (range 0–4).
Nociceptive visceral pain increased from 1 at baseline to 5 at the end of study, reportedly unaffected by exercise. The neuropathic and the musculoskeletal pain intensity in the same individual decreased.
WUSPI
Five participants reported shoulder pain and were assessed using the WUSPI (Table 2). Total mean WUSPI score at baseline was 37 and at the end of study 18.
Patient global impression of change—PGIC
The PGIC was used to rate the global effect of the treatment period on all types of pain and on neuropathic pain separately.
For all types of pain all eight participants reported an improvement (from minimally—very much improved); one reported being very much improved, four much improved and three minimally improved. For those with neuropathic pain four of the seven participants (57%) reported an improvement; two being much improved and two minimally improved. Three reported no change.
Pain interference and QoL
Median ratings of pain interference decreased for three of the six items included in the pain interference scale: ratings on amount of satisfaction or enjoyment from family-related activities, interference in day-to-day activities, and interference with mood. All median ratings of QoL improved, especially satisfaction with physical health (Q2), which increased from 5 to 8 (Table 3).
Compliance and adverse events
None of the 13 participants included in the protocol dropped out of the study. All completed the 30 training sessions. None developed pain owing to overuse and none of those with neuropathic pain reported an increase in intensity. One participant (not included in the pain protocol) reported transient low-back pain owing to difficulties with finding a good sitting position in the double-poling ergometer.
Discussion
This exploratory study included eight individuals with pain (62% of the total sample), but as the effects of regular exercise on pain, especially on neuropathic pain, are poorly documented we believe that our findings are of much interest. Four of the five individuals with musculoskeletal pain reported having no problem with pain after the 30 training sessions and four of seven with neuropathic pain (six of ten pain locations) showed a clinically significant pain intensity reduction of ⩾1.8 units on a 0–10 NRS.20 All participants reported a favourable effect on their global pain using the PGIC and four of seven (57%) on their neuropathic pain. Considering the duration of neuropathic pain it is rather surprising that this amount of pain relief can be obtained after only 10 weeks of regular exercise. The results on neuropathic pain are particularly interesting since no studies on exercise for neuropathic pain in humans have been published to our knowledge; but rodent studies on signs of neuropathic pain confirm our findings.10, 11, 12 Aerobic exercise on a treadmill improved signs of peripheral neuropathic pain in rodents and the effect depended on exercise intensity, but not on frequency.12 In another study of signs of neuropathic pain in rats with spinal-cord contusion, treadmill training decreased allodynia, whereas swimming only had a transient effect.10 However, swimming was concluded to be beneficial for relieving signs of neuropathic pain in rodents with peripheral nerve injury.11 In all of these studies it seems like the intensity and the duration of the training period are important parameters for obtaining an effect on neuropathic pain. Unfortunately, we did not monitor pain relief over time in our study.
The amount of effect on neuropathic pain seen in our study is in line with the effects of anticonvulsant and antidepressant drugs studied for treating SCI neuropathic pain.21, 22 Thus, an intensive aerobic exercise programme could be considered also in individuals with SCI neuropathic pain.
The effects on musculoskeletal pain were less surprising, but still interesting, as our study assessed the effect of a combined aerobic and strengthening exercise programme as opposed to previous studies on shoulder pain, where focus has been mainly on strengthening exercises.4, 5 The fact that none of our participants developed pain during the training period, but instead improved, might be because of the interval-training programme design, with repeated breaks and safe movements between 80 degrees of flexion and 40 degrees of extension. Median value in pain intensity ratings decreased from 4 to 0 and number of days with pain the previous 7 days from 5.5 to 0.7 in our study. Mean WUSPI score decreased from 37 at baseline to 18 at the end of study, similar to others’ findings in exercise studies of SCI shoulder pain.5, 6, 7 The results of our and other studies5, 6, 7 show that an intense exercise programme for at least 10 weeks should be prescribed for musculoskeletal overuse syndromes as a supplement to, or instead of, a pharmacological approach, and should be evaluated before considering surgery.
We also found a small decrease in pain interference items (already relatively low at baseline) and an increase in ratings of QoL, especially on satisfaction with physical health, from a median of 5 to 8, a substantial increase reflecting satisfaction with the outcome. These results are supported by Hicks et al.8 in an RCT assessing long-term exercise training for overall pain as well as by studies on strengthening programmes for shoulder pain.4 We were surprised to find this amount of increase in satisfaction as baseline values were collected in the summer, at the end of vacation and then again in wintertime with much snow, limiting everyone in a wheelchair in their daily activities.
A limitation of this exploratory study was the low number of participants and the lack of control group with SCI, who were to take part in the tests and not in the training. However, it was decided early on not to attempt to recruit such a group based on the limited number of potential subjects and the additional difficulty in finding a group of persons with a sufficient match of critical variables with the experimental group. The exercise programme was designed and evaluated for assessing the effects on aerobic and mechanical power, and not primarily for pain, for which reason no general conclusions can be drawn from our study. Still, the results indicate that an intensive exercise programme can be of value for treating SCI neuropathic pain. They also highlight the importance of studying the effects in a large randomized controlled trial, with long-term follow-up. Exercise intensity, number of training sessions per week and length of training period are important parameters to monitor. Despite the lack of studies on exercise as treatment for SCI neuropathic pain, we recommend health-care staff to consider prescribing regular physical training for this group as it is a safe treatment option with many more advantages than just pain relief.
Data Archiving
There was no data to deposit.
References
Norrbrink Budh C, Lund I, Ertzgaard P, Holtz A, Levi R, Hultling C et al. Pain in a Swedish spinal cord injury population. Clinical Rehabilitation 2003; 17: 685–690.
Baastrup C, Finnerup NB . Pharmacological management of neuropathic pain following spinal cord injury. CNS Drugs 2008; 22: 455–475.
Heutink M, Post MW, Wollaars MM, van Asbeck FW . Chronic spinal cord injury pain: pharmacological and non-pharmacological treatments and treatment effectiveness. Disabil Rehabil 2011; 33: 433–440.
Mulroy SJ, Thompson L, Kemp B, Pate Hatchett P, Newsam CJ, Gutierrez Lupold D et al. Strengthening and optimal movements for painful shoulders (STOMPS) in chronic spinal cord injury; a randomized controlled trial. Phys Ther 2011; 91: 305–324.
Curtis KA, Tyner TM, Zachary L, Lentell G, Brink D, Didyk T et al. Effects of a standard exercise protocol on shoulder pain in long-term wheelchair users. Spinal Cord 1999; 37: 421–429.
Nawoczenski DA, Ritter-Soronen JM, Wilson CM, Howe BA, Ludewig PM . Clinical trial of exercise for shoulder pain in chronic spinal injury. Phys Ther 2006; 86: 1604–1618.
Nash MS, van de Ven I, van Elk N, Johnson BM . Effects of circuit resistance training on fitness attributes and upper-extremity pain in middle-aged men with paraplegia. Arch Phys Med Rehabil 2007; 88: 70–75.
Hicks AL, Martin KA, Ditor DS, Latimer AE, Craven C, Bugaresti J et al. Long-term exercise training in persons with spinal cord injury: effects on strength, arm ergometry performance and psychological well-being. Spinal Cord 2003; 41: 34–43.
Martin Ginis KA, Bugaresti J, Craven BC . Using exercise to enhance subjective well-being among people with spinal cord injury: the mediating influences of stress and pain. Rehabil Psychol 2003; 48: 157–164.
Hutchinson KJ, Gómez-Pinilla F, Crowe MJ, Ying Z, Basso DM . Three exercise paradigms differentially improve sensory recovery after spinal cord contusion in rats. Brain 2004; 127: 1403–1414.
Kuphal KE, Fibuch EE, Tylor BK . Extended swimming exercise reduces inflammatory and peripheral neuropathic pain in rodents. J Pain 2007; 8: 989–997.
Stagg NJ, Mata HP, Ibrahim MM, Henriksen EJ, Porreca F, Vanderah TW et al. Regular exercise reverses sensory hypersensitivity in a rat neuropathic pain model. Anasthes 2011; 114: 940–948.
Bjerkefors A, Tinmark F, Nilsson J, Arndt A . Seated double-poling ergometer performance of individuals with spinal cord injury—a new ergometer concept for standardized upper body exercise. Int J Sports Med (submitted).
Jacobs PL, Nash MS . Exercise recommendations for individuals with spinal cord injury. Sports Med 2004; 34: 727–751.
Lindberg T, Arndt A, Norrbrink C, Wahman K, Bjerkefors A . Effects of seated double-poling ergometer training on aerobic and mechanical power in individuals with spinal cord injury. J Rehab Med (submitted).
Widerström-Noga E, Biering-Sørensen F, Bryce T, Cardenas DD, Finnerup NB, Jensen MP et al. The international spinal cord injury pain basic data set. Spinal Cord 2008; 46: 818–823.
International spinal cord injury data sets—Quality of life basic data set (version 1.0) 1.0). www.iscos.org.uk. Retrieved August 2010.
Farrar JT, Young Jr JP, LaMoreaux L et al. Clinical importance of changes in chronic pain intensity measured on an 11-point numerical pain rating scale. Pain 2001; 94: 149–158.
Curtis KA, Roach KE, Applegate EB et al. Development of the Wheelchair User's Shoulder Pain Index (WUSPI). Paraplegia 1995; 33: 290–293.
Hanley MA, Jensen MP, Ehde DM et al. Clinically significant change in pain intensity rating in persons with spinal cord injury or amputation. Clin J Pain 2006; 22: 25–31.
Siddall PJ, Cousins MJ, Otte A, Griesing T, Chambers R, Murphy TK . Pregabalin in central neuropathic pain associated with spinal cord injury: a placebo-controlled trial. Neurology 2006; 67: 1792–1800.
Rintala DH, Holmes SA, Courtade D, Fiess RN, Tastard LV, Loubser PG . Comparison of the effectiveness of amitriptyline and gabapentin on chronic neuropathic pain in persons with spinal cord injury. Arch Phys Med Rehabil 2007; 88: 1547–1560.
Acknowledgements
The Swedish Association of Persons with Neurological Disabilities, the Promobilia Foundation and the Swedish National Centre for Research in Sports are greatly thanked for their contribution to this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Norrbrink, C., Lindberg, T., Wahman, K. et al. Effects of an exercise programme on musculoskeletal and neuropathic pain after spinal cord injury—results from a seated double-poling ergometer study. Spinal Cord 50, 457–461 (2012). https://doi.org/10.1038/sc.2011.160
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sc.2011.160
Keywords
This article is cited by
-
A Comparison of Neuropathic Pain Experiences Among Paralympic Versus Recreational Athletes with Spinal Cord Injury
Sports Medicine - Open (2023)
-
Hybrid high-intensity interval training using functional electrical stimulation leg cycling and arm ski ergometer for people with spinal cord injuries: a feasibility study
Pilot and Feasibility Studies (2022)
-
Long-term physical therapy for neuropathic pain after cervical spinal cord injury and resting state electroencephalography: a case report
Spinal Cord Series and Cases (2022)
-
The CanPain SCI clinical practice guidelines for rehabilitation management of neuropathic pain after spinal cord injury: 2021 update
Spinal Cord (2022)
-
Effects of transcranial direct current stimulation followed by exercise on neuropathic pain in chronic spinal cord injury: a double-blinded randomized controlled pilot trial
Spinal Cord (2021)