Abstract
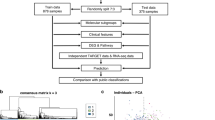
Medulloblastoma, the most common malignant paediatric brain tumour, is currently diagnosed and stratified using a combination of clinical and demographic variables. Recent transcriptomic approaches have demonstrated that the histological entity known as medulloblastoma is comprised of multiple clinically and molecularly distinct subgroups. The current consensus is that four defined subgroups of medulloblastoma exist: WNT, SHH, Group 3, and Group 4. Each subgroup probably contains at least one additional level of hierarchy, with some evidence for multiple subtypes within each subgroup. The demographic and clinical differences between the subgroups present immediate and pressing questions to be addressed in the next round of clinical trials for patients with medulloblastoma. Many of the genetically defined targets for rational medulloblastoma therapies are unique to a given subgroup, suggesting the need for subgroup-specific trials of novel therapies. The development of practical, robust and widely accepted subgroup biomarkers that are amenable to the conditions of a prospective clinical trial is, therefore, an urgent need for the paediatric neuro-oncology community. In this Review, we discuss the clinical implications of molecular subgrouping in medulloblastoma, highlighting how these subgroups are transitioning from a research topic in the laboratory to a clinically relevant topic with important implications for patient care.
Key Points
-
Medulloblastoma is no longer regarded as a single disease: at least four main subgroups—WNT, SHH, Group 3, and Group 4—are now accepted to exist
-
Each subgroup of medulloblastoma exhibits distinct patient demographics, underlying genomics, and transcriptomics, which leads to disparate clinical presentation
-
Patient subgroup status will become an integral component of prospective clinical trials, and will enable the use of treatment protocols that are rationally tailored towards each subgroup of the disease
-
Methods to verify patient subgroup affiliation will continue to evolve and become increasingly important as subgrouping of patients becomes routine in clinical practice
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout





Similar content being viewed by others
References
Rorke, L. B. The cerebellar medulloblastoma and its relationship to primitive neuroectodermal tumours. J. Neuropathol. Exp. Neurol. 42, 1–15 (1983).
Northcott, P. A., Rutka, J. T. & Taylor, M. D. Genomics of medulloblastoma: from Giemsa-banding to next-generation sequencing in 20 years. Neurosurg. Focus 28, E6 (2010).
Pietsch, T., Taylor, M. D. & Rutka, J. T. Molecular pathogenesis of childhood brain tumours. J. Neurooncol. 70, 203–215 (2004).
Yokota, N. et al. Identification of differentially expressed and developmentally regulated genes in medulloblastoma using suppression subtraction hybridization. Oncogene 23, 3444–3453 (2004).
Park, P. C. et al. Transcriptional profiling of medulloblastoma in children. J. Neurosurg. 99, 534–541 (2003).
Mainprize, T. G., Taylor, M. D. & Rutka, J. T. Pediatric brain tumours: a contemporary prospectus. Clin. Neurosurg. 47, 259–302 (2000).
Taylor, M. D., Mainprize, T. G. & Rutka, J. T. Molecular insight into medulloblastoma and central nervous system primitive neuroectodermal tumor biology from hereditary syndromes: a review. Neurosurgery 47, 888–901 (2000).
Bayani, J. et al. Molecular cytogenetic analysis of medulloblastomas and supratentorial primitive neuroectodermal tumours by using conventional banding, comparative genomic hybridization, and spectral karyotyping. J. Neurosurg. 93, 437–448 (2000).
Packer, R. J. Medulloblastoma. J. Neurosurg. 103, 299–300 (2005).
Packer, R. J., Rood, B. R. & MacDonald, T. J. Medulloblastoma: present concepts of stratification into risk groups. Pediatr. Neurosurg. 39, 60–67 (2003).
Packer, R. J. Childhood medulloblastoma: progress and future challenges. Brain Dev. 21, 75–81 (1999).
Packer, R. J. et al. Outcome for children with medulloblastoma treated with radiation and cisplatin, CCNU, and vincristine chemotherapy. J. Neurosurg. 81, 690–698 (1994).
Johnson, D. L. et al. Quality of long-term survival in young children with medulloblastoma. J. Neurosurg. 80, 1004–1010 (1994).
Packer, R. J. & Finlay, J. L. Medulloblastoma: presentation, diagnosis and management. Oncology 2, 35–45, 48–9 (1988).
Packer, R. J., Sutton, L. N., D'Angio, G., Evans, A. E. & Schut, L. Management of children with primitive neuroectodermal tumours of the posterior fossa/medulloblastoma. Pediatr. Neurosci. 12, 272–282 (1985).
Massimino, M. et al. Childhood medulloblastoma. Crit. Rev. Oncol. Hematol. 79, 65–83 (2011).
Rutkowski, S. et al. Medulloblastoma in young children. Pediatr. Blood Cancer 54, 635–637 (2010).
Rutkowski, S. Current treatment approaches to early childhood medulloblastoma. Expert Rev. Neurother. 6, 1211–1221 (2006).
Rutkowski, S. et al. Treatment of early childhood medulloblastoma by postoperative chemotherapy alone. N. Engl. J. Med. 352, 978–986 (2005).
Partap, S. et al. Medulloblastoma incidence has not changed over time: a CBTRUS study. J. Pediatr. Hematol. Oncol. 31, 970–971 (2009).
Curran, E. K., Le, G. M., Sainani, K. L., Propp, J. M. & Fisher, P. G. Do children and adults differ in survival from medulloblastoma? A study from the SEER registry. J. Neurooncol. 95, 81–85 (2009).
Fisher, P. G., Burger, P. C. & Eberhart, C. G. Biologic risk stratification of medulloblastoma: the real time is now. J. Clin. Oncol. 22, 971–974 (2004).
Raabe, E. H. & Eberhart, C. G. High-risk medulloblastoma: does cmyc amplification overrule histopathology? Pediatr. Blood Cancer 54, 344–345 (2010).
Eberhart, C. G. et al. Histopathological and molecular prognostic markers in medulloblastoma: cmyc, Nmyc, TrkC, and anaplasia. J. Neuropathol. Exp. Neurol. 63, 441–449 (2004).
Finkelstein-Shechter, T. et al. Atypical teratoid or rhabdoid tumours: improved outcome with high-dose chemotherapy. J. Pediatr. Hematol. Oncol. 32, e182–e186 (2010).
Biegel, J. A. et al. Mutations of the INI1 rhabdoid tumor suppressor gene in medulloblastomas and primitive neuroectodermal tumours of the central nervous system. Clin. Cancer Res. 6, 2759–2763 (2000).
Rorke, L. B., Packer, R. J. & Biegel, J. A. Central nervous system atypical teratoid/rhabdoid tumours of infancy and childhood: definition of an entity. J. Neurosurg. 85, 56–65 (1996).
Rorke, L. B., Packer, R. & Biegel, J. Central nervous system atypical teratoid/rhabdoid tumours of infancy and childhood. J. Neurooncol. 24, 21–28 (1995).
Biegel, J. A., Rorke, L. B. & Emanuel, B. S. Monosomy 22 in rhabdoid or atypical teratoid tumours of the brain. N. Engl. J. Med. 321, 906 (1989).
Lafay-Cousin, L. et al. Central nervous system atypical teratoid rhabdoid tumours: the Canadian Paediatric Brain Tumour Consortium experience. Eur. J. Cancer 48, 353–359 (2011).
Finkelstein-Shechter, T. et al. Atypical teratoid or rhabdoid tumours: improved outcome with high-dose chemotherapy. J. Pediatr. Hematol. Oncol. 32, e182–e186 (2010).
Taylor, M. D. et al. Familial posterior fossa brain tumours of infancy secondary to germline mutation of the hSNF5 gene. Am. J. Hum. Genet. 66, 1403–1406 (2000).
Wang, Y. et al. Embryonal tumor with abundant neuropil and true rosettes (ETANTR) with a focal amplification at chromosome 19q13.42 locus: further evidence of two new instances in China. Neuropathology 31, 639–647 (2011).
Ferri Niguez, B. et al. Embryonal tumor with abundant neuropil and true rosettes (ETANTR): a new distinctive variety of pediatric PNET: a case-based update. Childs Nerv. Syst. 26, 1003–1008 (2010).
Li, M. et al. Frequent amplification of a chr19q13.41 microRNA polycistron in aggressive primitive neuroectodermal brain tumours. Cancer Cell 16, 533–546 (2009).
Pfister, S. et al. Novel genomic amplification targeting the microRNA cluster at 19q13.42 in a pediatric embryonal tumor with abundant neuropil and true rosettes. Acta Neuropathol. 117, 457–464 (2009).
McManamy, C. S. et al. Nodule formation and desmoplasia in medulloblastomas-defining the nodular/desmoplastic variant and its biological behavior. Brain Pathol. 17, 151–164 (2007).
Rutkowski, S. et al. Survival and prognostic factors of early childhood medulloblastoma: an international meta-analysis. J. Clin. Oncol. 28, 4961–4968 (2010).
Garre, M. L. et al. Medulloblastoma variants: age-dependent occurrence and relation to Gorlin syndrome-a new clinical perspective. Clin. Cancer Res. 15, 2463–2471 (2009).
Stearns, D. et al. cMyc overexpression causes anaplasia in medulloblastoma. Cancer Res. 66, 673–681 (2006).
Golub, T. R. et al. Molecular classification of cancer: class discovery and class prediction by gene expression monitoring. Science 286, 531–537 (1999).
Pomeroy, S. L. et al. Prediction of central nervous system embryonal tumour outcome based on gene expression. Nature 415, 436–442 (2002).
Al-Halabi, H. et al. Preponderance of sonic hedgehog pathway activation characterizes adult medulloblastoma. Acta Neuropathol. 121, 229–239 (2011).
Buonamici, S. et al. Interfering with resistance to smoothened antagonists by inhibition of the PI3K pathway in medulloblastoma. Sci. Transl. Med. 2, 51ra70 (2010).
Cho, Y. J. et al. Integrative genomic analysis of medulloblastoma identifies a molecular subgroup that drives poor clinical outcome. J. Clin. Oncol. 29, 1424–30 (2011).
Ellison, D. W. et al. Medulloblastoma: clinicopathological correlates of SHH, WNT, and non-SHH/WNT molecular subgroups. Acta Neuropathol. 121, 381–396 (2011).
Ellison, D. W. et al. Definition of disease-risk stratification groups in childhood medulloblastoma using combined clinical, pathologic, and molecular variables. J. Clin. Oncol. 29, 1400–1407 (2011).
Ellison, D. W. et al. β-catenin status predicts a favorable outcome in childhood medulloblastoma: the United Kingdom Children's Cancer Study Group Brain Tumour Committee. J. Clin. Oncol. 23, 7951–7957 (2005).
Gibson, P. et al. Subtypes of medulloblastoma have distinct developmental origins. Nature 468, 1095–1099 (2010).
Kool, M. et al. Molecular subgroups of medulloblastoma: an international meta-analysis of transcriptome, genetic aberrations, and clinical data of WNT, SHH, Group 3, and Group 4 medulloblastomas. Acta Neuropathol. 123, 473–484 (2012).
Korshunov, A. et al. Biological and clinical heterogeneity of MYCN-amplified medulloblastoma. Acta Neuropathol. 123, 515–527 (2012).
Northcott, P. A. et al. Medulloblastoma comprises four distinct molecular variants. J. Clin. Oncol. 29, 1408–1414 (2011).
Northcott, P. A. et al. Multiple recurrent genetic events converge on control of histone lysine methylation in medulloblastoma. Nat. Genet. 41, 465–472 (2009).
Remke, M. et al. Adult medulloblastoma comprises three major molecular variants. J. Clin. Oncol. 29, 2717–2723 (2011).
Rudin, C. M. et al. Treatment of medulloblastoma with hedgehog pathway inhibitor GDC-0449. N. Engl. J. Med. 361, 1173–1178 (2009).
Taylor, M. D. et al. Molecular subgroups of medulloblastoma: the current consensus. Acta Neuropathol. 123, 465–472 (2011).
Thompson, M. C. et al. Genomics identifies medulloblastoma subgroups that are enriched for specific genetic alterations. J. Clin. Oncol. 24, 1924–1931 (2006).
Yauch, R. L. et al. Smoothened mutation confers resistance to a Hedgehog pathway inhibitor in medulloblastoma. Science 326, 572–574 (2009).
Kool, M. et al. Integrated genomics identifies five medulloblastoma subtypes with distinct genetic profiles, pathway signatures and clinicopathological features. PLoS ONE 3, e3088 (2008).
Northcott, P. A. et al. Pediatric and adult sonic hedgehog medulloblastomas are clinically and molecularly distinct. Acta Neuropathol. 122, 231–240 (2011).
Remke, M. et al. FSTL5 is a marker of poor prognosis in non-WNT/non-SHH medulloblastoma. J. Clin. Oncol. 29, 3852–3861 (2011).
Taylor, M. D. et al. Molecular subgroups of medulloblastoma: the current consensus. Acta Neuropathol. 123, 465–472 (2012).
Hamilton, S. R. et al. The molecular basis of Turcot's syndrome. N. Engl. J. Med. 332, 839–847 (1995).
Zurawel, R. H., Chiappa, S. A., Allen, C. & Raffel, C. Sporadic medulloblastomas contain oncogenic β-catenin mutations. Cancer Res. 58, 896–899 (1998).
Yokota, N. et al. Role of Wnt pathway in medulloblastoma oncogenesis. Int. J. Cancer. 101, 198–201 (2002).
Goodrich, L. V., Milenkovic, L., Higgins, K. M. & Scott, M. P. Altered neural cell fates and medulloblastoma in mouse patched mutants. Science 277, 1109–1113 (1997).
Ng, D. et al. Retrospective family study of childhood medulloblastoma. Am. J. Med. Genet. A. 134, 399–403 (2005).
Taylor, M. D. et al. Mutations in SUFU predispose to medulloblastoma. Nat. Genet. 31, 306–310 (2002).
Slade, I. et al. Heterogeneity of familial medulloblastoma and contribution of germline PTCH1 and SUFU mutations to sporadic medulloblastoma. Fam. Cancer 10, 337–342 (2011).
Brugieres, L. et al. Incomplete penetrance of the predisposition to medulloblastoma associated with germ-line SUFU mutations. J. Med. Genet. 47, 142–144 (2010).
Pastorino, L. et al. Identification of a SUFU germline mutation in a family with Gorlin syndrome. Am. J. Med. Genet. A 149A, 1539–1543 (2009).
Taylor, M. D. et al. Failure of a medulloblastoma-derived mutant of SUFU to suppress WNT signaling. Oncogene 23, 4577–4583 (2004).
Rubin, J. B. & Rowitch, D. H. Medulloblastoma: a problem of developmental biology. Cancer Cell 2, 7–8 (2002).
Fernandez, L. A. et al. Oncogenic YAP promotes radioresistance and genomic instability in medulloblastoma through IGF2-mediated Akt activation. Oncogene 31, 1923–1937 (2012).
Fernandez, L. A. et al. YAP1 is amplified and up-regulated in hedgehog-associated medulloblastomas and mediates Sonic hedgehog-driven neural precursor proliferation. Genes Dev. 23, 2729–2741 (2009).
Fernandez, L. A., Northcott, P. A., Taylor, M. D. & Kenney, A. M. Normal and oncogenic roles for microRNAs in the developing brain. Cell Cycle 8, 4049–4054 (2009).
Northcott, P. A. et al. The miR-17/92 polycistron is up-regulated in sonic hedgehog-driven medulloblastomas and induced by N-myc in sonic hedgehog-treated cerebellar neural precursors. Cancer Res. 69, 3249–3255 (2009).
Hatton, B. A. et al. N-myc is an essential downstream effector of Shh signaling during both normal and neoplastic cerebellar growth. Cancer Res. 66, 8655–8661 (2006).
Browd, S. R. et al. N-myc can substitute for insulin-like growth factor signaling in a mouse model of sonic hedgehog-induced medulloblastoma. Cancer Res. 66, 2666–2672 (2006).
Kenney, A. M., Widlund, H. R. & Rowitch, D. H. Hedgehog and PI-3 kinase signaling converge on Nmyc1 to promote cell cycle progression in cerebellar neuronal precursors. Development 131, 217–228 (2004).
Kenney, A. M., Cole, M. D. & Rowitch, D. H. Nmyc upregulation by sonic hedgehog signaling promotes proliferation in developing cerebellar granule neuron precursors. Development 130, 15–28 (2003).
Uziel, T. et al. The miR-17∼92 cluster collaborates with the Sonic Hedgehog pathway in medulloblastoma. Proc. Natl Acad. Sci. USA 106, 2812–2817 (2009).
Pfaff, E. et al. TP53 mutation is frequently associated with CTNNB1 mutation or MYCN amplification and is compatible with long-term survival in medulloblastoma. J. Clin. Oncol. 28, 5188–5196 (2010).
Pfister, S. M. et al. Molecular diagnostics of CNS embryonal tumours. Acta Neuropathol. 120, 553–566 (2010).
Korshunov, A. et al. Adult and pediatric medulloblastomas are genetically distinct and require different algorithms for molecular risk stratification. J. Clin. Oncol. 28, 3054–3060 (2010).
Pfister, S. et al. Outcome prediction in pediatric medulloblastoma based on DNA copy-number aberrations of chromosomes 6q and 17q and the MYC and MYCN loci. J. Clin. Oncol. 27, 1627–1636 (2009).
Swartling, F. J. et al. Pleiotropic role for MYCN in medulloblastoma. Genes Dev. 24, 1059–1072 (2010).
Bunt, J. et al. Joint binding of OTX2 and MYC in promotor regions is associated with high gene expression in medulloblastoma. PLoS ONE 6, e26058 (2011).
Bunt, J. et al. OTX2 directly activates cell cycle genes and inhibits differentiation in medulloblastoma cells. Int. J. Cancer http://dx.doi.org/10.1002/ijc.26474.
Adamson, D. C. et al. OTX2 is critical for the maintenance and progression of Shh-independent medulloblastomas. Cancer Res. 70, 181–191 (2010).
de Haas, T. et al. OTX1 and OTX2 expression correlates with the clinicopathologic classification of medulloblastomas. J. Neuropathol. Exp. Neurol. 65, 176–186 (2006).
Di, C. et al. Identification of OTX2 as a medulloblastoma oncogene whose product can be targeted by all-trans retinoic acid. Cancer Res. 65, 919–924 (2005).
Boon, K., Eberhart, C. G. & Riggins, G. J. Genomic amplification of orthodenticle homologue 2 in medulloblastomas. Cancer Res. 65, 703–707 (2005).
Malkov, V. A. et al. Multiplexed measurements of gene signatures in different analytes using the Nanostring nCounter™ Assay System. BMC Res. Notes 2, 80 (2009).
Geiss, G. K. et al. Direct multiplexed measurement of gene expression with color-coded probe pairs. Nat. Biotechnol. 26, 317–325 (2008).
Northcott, P. A. et al. Rapid, reliable, and reproducible molecular sub-grouping of clinical medulloblastoma samples. Acta Neuropathol. 123, 615–626 (2011).
Kongkham, P. N. et al. The SFRP family of WNT inhibitors function as novel tumor suppressor genes epigenetically silenced in medulloblastoma. Oncogene 29, 3017–3024 (2010).
Nakahara, Y. et al. Genetic and epigenetic inactivation of Kruppel-like factor 4 in medulloblastoma. Neoplasia 12, 20–27 (2010).
Kongkham, P. N. et al. An epigenetic genome-wide screen identifies SPINT2 as a novel tumor suppressor gene in pediatric medulloblastoma. Cancer Res. 68, 9945–9953 (2008).
Kasuga, C. et al. Expression of MAGE and GAGE genes in medulloblastoma and modulation of resistance to chemotherapy. Laboratory investigation. J. Neurosurg. Pediatr. 1, 305–313 (2008).
Bertrand, K. C. et al. PCDH10 is a candidate tumour suppressor gene in medulloblastoma. Childs Nerv. Syst. 27, 1243–1249 (2011).
Parsons, D. W. et al. The genetic landscape of the childhood cancer medulloblastoma. Science 331, 435–439 (2011).
Milde, T. et al. HDAC5 and HDAC9 in medulloblastoma: novel markers for risk stratification and role in tumor cell growth. Clin. Cancer Res. 16, 3240–3252 (2010).
Bhatia, B. et al. Tuberous sclerosis complex suppression in cerebellar development and medulloblastoma: separate regulation of mammalian target of rapamycin activity and p27Kip1 localization. Cancer Res. 69, 7224–7234 (2009).
Garzia, L. et al. MicroRNA-199b-5p impairs cancer stem cells through negative regulation of HES1 in medulloblastoma. PLoS ONE 4, e4998 (2009).
Wu, X. et al. Clonal selection drives genetic divergence of metastatic medulloblastoma. Nature 482, 529–533 (2012).
Singh, S. K. et al. Identification of human brain tumour initiating cells. Nature 432, 396–401 (2004).
Fan, X. & Eberhart, C. G. Medulloblastoma stem cells. J. Clin. Oncol. 26, 2821–2827 (2008).
Wu, X., Northcott, P. A., Croul, S. & Taylor, M. D. Mouse models of medulloblastoma. Chin. J. Cancer 30, 442–449 (2011).
Pei, Y. et al. An animal model of MYC-driven medulloblastoma. Cancer Cell 21, 155–167 (2012).
Kawauchi, D. et al. A mouse model of the most aggressive subgroup of human medulloblastoma. Cancer Cell 21, 168–180 (2012).
Gilbertson, R. J. & Ellison, D. W. The origins of medulloblastoma subtypes. Annu. Rev. Pathol. 3, 341–365 (2008).
Yang, Z. J. et al. Medulloblastoma can be initiated by deletion of patched in lineage-restricted progenitors or stem cells. Cancer Cell 14, 135–145 (2008).
Oliver, T. G. et al. Loss of patched and disruption of granule cell development in a pre-neoplastic stage of medulloblastoma. Development 132, 2425–2439 (2005).
Wechsler-Reya, R. & Scott, M. P. The developmental biology of brain tumours. Annu. Rev. Neurosci. 24, 385–428 (2001).
Wechsler-Reya, R. J. & Scott, M. P. Control of neuronal precursor proliferation in the cerebellum by Sonic Hedgehog. Neuron 22, 103–114 (1999).
Hudson, T. J. et al. International network of cancer genome projects. Nature 464, 993–998 (2010).
Acknowledgements
M. D. Taylor is supported by a Clinician-Scientist Phase II award from the Canadian Institutes of Health Research. Research in the Taylor laboratory is funded by the Pediatric Brain Tumor Foundation and the NIH (R01CA148699). P. A. Northcott is supported by a Roman Herzog Postdoctoral Fellowship. We thank Susan Archer for technical writing assistance.
Author information
Authors and Affiliations
Contributions
P. A. Northcott and M. D. Taylor researched data for the article, provided substantial contributions to discussion of content, wrote the article, and contributed to review and editing of the manuscript before submission. A. Korshunov contributed to writing the article and to the review and editing of the manuscript before submission. S. M. Pfister reviewed and edited the manuscript before submission.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Rights and permissions
About this article
Cite this article
Northcott, P., Korshunov, A., Pfister, S. et al. The clinical implications of medulloblastoma subgroups. Nat Rev Neurol 8, 340–351 (2012). https://doi.org/10.1038/nrneurol.2012.78
Published:
Issue Date:
DOI: https://doi.org/10.1038/nrneurol.2012.78
This article is cited by
-
B7-H6 enhances F-actin rearrangement by targeting c-MYC activation to promote medulloblastoma migration and invasion
Medical Oncology (2023)
-
miRNA-211 maintains metabolic homeostasis in medulloblastoma through its target gene long-chain acyl-CoA synthetase 4
Acta Neuropathologica Communications (2023)
-
Radiomics signature for the prediction of progression-free survival and radiotherapeutic benefits in pediatric medulloblastoma
Child's Nervous System (2022)
-
G9a/EHMT2 is a Potential Prognostic Biomarker and Molecular Target in SHH Medulloblastoma
NeuroMolecular Medicine (2022)
-
Primary leptomeningeal medulloblastoma: a case-based review
Child's Nervous System (2022)