Abstract
1–4% of patients who undergo gastric biopsy have gastric polyps. These lesions may be true epithelial polyps, heterotopias, lymphoid tissue, or stromal lesions. Hyperplastic polyps, which arise in patients with underlying gastritis, and fundic-gland polyps, which are associated with PPI therapy, are the most common gastric polyps; however, prevalence varies widely relative to the local prevalence of Helicobacter pylori infection and use of PPI therapy. Some polyps have characteristic topography, size, and endoscopic appearance. Approximately 20% of biopsy specimens identified endoscopically as polyps have no definite pathological diagnosis. Evaluation of the phenotype of the gastric mucosa that surrounds a lesion will provide significant information crucial to the evaluation, diagnosis and management of a patient. The presence of a gastric adenoma should prompt the search for a coexistent carcinoma. The endoscopic characteristics, histopathology, pathogenesis, and management recommendations of polyps and common polypoid lesions in the stomach are discussed in this Review.
Key Points
-
Multiple entities may present as a gastric polypoid lesion, and many have subtle yet characteristic endoscopic features
-
In Western countries, fundic-gland polyps are now more common than hyperplastic polyps, resulting from the increase in PPI therapy and decrease in gastritis associated with Helicobacter pylori infection
-
Biopsy specimens of the gastric mucosa adjacent to a lesion are extremely important in establishing an etiology when hyperplastic polyps, adenomas, and carcinoids are present
-
Surveillance is indicated in patients with polyposis syndromes and adenomas; patients with gastrointestinal stromal tumors and carcinoids may be followed up endoscopically, but management approach should be tailored to each individual
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout








Similar content being viewed by others
References
Park, D. Y. & Lauwers, G. Y. Gastric polyps: classification and management. Arch. Pathol. Lab. Med. 132, 633–640 (2008).
Ming, S. C. The classification and significance of gastric polyps. Monogr. Pathol. 18, 149–175 (1977).
Stolte, M. Clinical consequences of the endoscopic diagnosis of gastric polyps. Endoscopy 27, 32–37 (1995).
Stolte, M. et al. Frequency, location, and age and sex distribution of various types of gastric polyp. Endoscopy 26, 659–665 (1994).
Archimandritis, A. et al. Gastric epithelial polyps: a retrospective endoscopic study of 12974 symptomatic patients. Ital. J. Gastroenterol. 28, 387–390 (1996).
Morais, D. J. et al. Gastric polyps: a retrospective analysis of 26,000 digestive endoscopies. Arq. Gastroenterol. 44, 14–17 (2007).
Nakamura, T. & Nakano, G. Histopathological classification and malignant change in gastric polyps. J. Clin. Pathol. 38, 754–764 (1985).
Farinati, F. et al. Early and advanced gastric cancer in the follow-up of moderate and severe gastric dysplasia patients. A prospective study. I. G. G. E. D.—-Interdisciplinary Group on Gastric Epithelial Dysplasia. Endoscopy 25, 261–264 (1993).
Lauwers, G. Y. & Srivastava, A. Gastric preneoplastic lesions and epithelial dysplasia. Gastroenterol. Clin. North Am. 36, 813–829 (2007).
Carmack, S. W. et al. The current spectrum of gastric polyps: a one-year national study of over 120,000 patients. Am. J. Gastroenterol. (in press).
Bertoni, G. et al. Dysplastic changes in gastric fundic gland polyps of patients with familial adenomatous polyposis. Ital. J. Gastroenterol. Hepatol. 31, 192–197 (1999).
Bianchi, L. K. et al. Fundic gland polyp dysplasia is common in familial adenomatous polyposis. Clin. Gastroenterol. Hepatol. 6, 180–185 (2008).
Attard, T. M. et al. Multicenter experience with upper gastrointestinal polyps in pediatric patients with familial adenomatous polyposis. Am. J. Gastroenterol. 99, 681–686 (2004).
Fossmark, R. et al. Serum gastrin and chromogranin A levels in patients with fundic gland polyps caused by long-term proton-pump inhibition. Scand. J. Gastroenterol. 43, 1–5 (2007).
Kim, J. S. et al. Spontaneous resolution of multiple fundic gland polyps after cessation of treatment with omeprazole. Korean J. Gastroenterol. 51, 305–308 (2008).
el-Zimaity, H. M. et al. Fundic gland polyps developing during omeprazole therapy. Am. J. Gastroenterol. 92, 1858–1860 (1997).
Raghunath, A. S. et al. Review article: the long-term use of proton-pump inhibitors. Aliment. Pharmacol. Ther. 22 (Suppl. 1), 55–63 (2005).
Declich, P. et al. Fundic gland polyps and PPI: the Mozart effect of gastrointestinal pathology? Pol. J. Pathol. 57, 181–182 (2006).
Vieth, M. & Stolte, M. Fundic gland polyps are not induced by proton pump inhibitor therapy. Am. J. Clin. Pathol. 116, 716–720 (2001).
Abraham, S. C. et al. Sporadic fundic gland polyps with epithelial dysplasia: evidence for preferential targeting for mutations in the adenomatous polyposis coli gene. Am. J. Pathol. 161, 1735–1742 (2002).
Abraham, S. C. et al. Sporadic fundic gland polyps: common gastric polyps arising through activating mutations in the β-catenin gene. Am. J. Pathol. 158, 1005–1010 (2001).
Torbenson, M. et al. Sporadic fundic gland polyposis: a clinical, histological, and molecular analysis. Mod. Pathol. 15, 718–723 (2002).
Declich, P. et al. Fundic gland polyps: a not so innocuous entity worth a careful evaluation. Am. J. Gastroenterol. 93, 2641 (1998).
Dirschmid, K. et al. Why is the hyperplastic polyp a marker for the precancerous condition of the gastric mucosa? Virchows Arch. 448, 80–84 (2006).
Malaty, H. M. Epidemiology of Helicobacter pylori infection. Best Pract. Res. Clin. Gastroenterol. 21, 205–214 (2007).
Abraham, S. C. et al. Hyperplastic polyps of the stomach: associations with histologic patterns of gastritis and gastric atrophy. Am. J. Surg. Pathol. 25, 500–507 (2001).
Cerwenka, H. et al. Pyloric obstruction caused by prolapse of a hyperplastic gastric polyp. Hepatogastroenterology 49, 958–960 (2002).
Chen, H. W. et al. Gastric outlet obstruction due to giant hyperplastic gastric polyps. J. Formos. Med. Assoc. 104, 852–855 (2005).
Dixon, M. F. et al. Reflux gastritis: distinct histopathological entity? J. Clin. Pathol. 39, 524–530 (1986).
Genta, R. M. Differential diagnosis of reactive gastropathy. Semin. Diagn. Pathol. 22, 273–283 (2005).
Ljubicic, N. et al. The effect of eradicating Helicobacter pylori infection on the course of adenomatous and hyperplastic gastric polyps. Eur. J. Gastroenterol. Hepatol. 11, 727–730 (1999).
Ohkusa, T. et al. Disappearance of hyperplastic polyps in the stomach after eradication of Helicobacter pylori. A randomized, clinical trial. Ann. Intern. Med. 129, 712–715 (1998).
Lauwers, G. Y. et al. p53 expression in precancerous gastric lesions: an immunohistochemical study of PAb 1801 monoclonal antibody on adenomatous and hyperplastic gastric polyps. Am. J. Gastroenterol. 88, 1916–1919 (1993).
Nogueira, A. M. et al. Microsatellite instability in hyperplastic and adenomatous polyps of the stomach. Cancer 86, 1649–1656 (1999).
Murakami, K. et al. p53, but not c-Ki-ras, mutation and down-regulation of p21WAF1/CIP1 and cyclin D1 are associated with malignant transformation in gastric hyperplastic polyps. Am. J. Clin. Pathol. 115, 224–234 (2001).
Yao, T. et al. Malignant transformation of gastric hyperplastic polyps: alteration of phenotypes, proliferative activity, and p53 expression. Hum. Pathol. 33, 1016–1022 (2002).
Hattori, T. Morphological range of hyperplastic polyps and carcinomas arising in hyperplastic polyps of the stomach. J. Clin. Pathol. 38, 622–630 (1985).
Zea-Iriarte, W. L. et al. Carcinoma in gastric hyperplastic polyps. A phenotypic study. Dig. Dis. Sci. 41, 377–386 (1996).
Yoshihara, M. et al. Correlation of ratio of serum pepsinogen I and II with prevalence of gastric cancer and adenoma in Japanese subjects. Am. J. Gastroenterol. 93, 1090–1096 (1998).
Laxen, F. et al. Gastric polyps; their morphological and endoscopical characteristics and relation to gastric carcinoma. Acta Pathol. Microbiol. Immunol. Scand. [A]. 90, 221–228 (1982).
Abraham, S. C. et al. Genetic alterations in gastric adenomas of intestinal and foveolar phenotypes. Mod. Pathol. 16, 786–795 (2003).
Hirota, W. K. et al. ASGE guideline: the role of endoscopy in the surveillance of premalignant conditions of the upper GI tract. Gastrointest. Endosc. 63, 570–580 (2006).
Dunlop, M. G. Guidance on gastrointestinal surveillance for hereditary non-polyposis colorectal cancer, familial adenomatous polypolis, juvenile polyposis, and Peutz–Jeghers syndrome. Gut 51 (Suppl. 5), V21–V27 (2002).
Hizawa, K. et al. Juvenile polyposis of the stomach: clinicopathological features and its malignant potential. J. Clin. Pathol. 50, 771–774 (1997).
Johnson, G. K. et al. Cronkite–Canada syndrome: gastrointestinal pathophysiology and morphology. Gastroenterology 63, 140–152 (1972).
Hizawa, K. et al. Gastrointestinal manifestations of Cowden's disease. Report of four cases. J. Clin. Gastroenterol. 18, 13–18 (1994).
Jagelman, D. G. et al. Upper gastrointestinal cancer in familial adenomatous polyposis. Lancet 1, 1149–1151 (1988).
Offerhaus, G. J. et al. The risk of upper gastrointestinal cancer in familial adenomatous polyposis. Gastroenterology 102, 1980–1982 (1992).
Giardiello, F. M. et al. Very high risk of cancer in familial Peutz–Jeghers syndrome. Gastroenterology 119, 1447–1453 (2000).
McGrath, D. R. & Spigelman, A. D. Preventive measures in Peutz–Jeghers syndrome. Fam. Cancer 1, 121–125 (2001).
Giardiello, F. M. & Trimbath, J. D. Peutz–Jeghers syndrome and management recommendations. Clin. Gastroenterol. Hepatol. 4, 408–415 (2006).
Howe, J. R. et al. The risk of gastrointestinal carcinoma in familial juvenile polyposis. Ann. Surg. Oncol. 5, 751–756 (1998).
Ward, E. M. & Wolfsen, H. C. Pharmacological management of Cronkhite–Canada syndrome. Expert Opin. Pharmacother. 4, 385–389 (2003).
Wirtzfeld, D. A. et al. Hamartomatous polyposis syndromes: molecular genetics, neoplastic risk, and surveillance recommendations. Ann. Surg. Oncol. 8, 319–327 (2001).
Hasegawa, T. et al. CD34 expression by inflammatory fibroid polyps of the stomach. Mod. Pathol. 10, 451–456 (1997).
Puri, A. S. et al. Giant inflammatory fibroid polyp of stomach causing massive upper gastrointestinal bleeding. Indian J. Gastroenterol. 10, 23–24 (1991).
Allibone, R. O. et al. Multiple and recurrent inflammatory fibroid polyps in a Devon family ('Devon polyposis syndrome'): an update. Gut 33, 1004–1005 (1992).
Pantanowitz, L. et al. Inflammatory fibroid polyps of the gastrointestinal tract: evidence for a dendritic cell origin. Am. J. Surg. Pathol. 28, 107–114 (2004).
Schildhaus, H. U. et al. Inflammatory fibroid polyps harbour mutations in the platelet-derived growth factor receptor α (PDGFRA) gene. J. Pathol. 216, 176–182 (2008).
Paikos, D. et al. Inflammatory fibroid polyp or Vanek's tumour. Dig. Surg. 24, 231–233 (2007).
Miettinen, M. & Lasota, J. Gastrointestinal stromal tumors—definition, clinical, histological, immunohistochemical, and molecular genetic features and differential diagnosis. Virchows Arch. 438, 1–12 (2001).
Nilsson, B. et al. Gastrointestinal stromal tumors: the incidence, prevalence, clinical course, and prognostication in the preimatinib mesylate era—a population-based study in western Sweden. Cancer 103, 821–829 (2005).
Kawanowa, K. et al. High incidence of microscopic gastrointestinal stromal tumors in the stomach. Hum. Pathol. 37, 1527–1535 (2006).
DeMatteo, R. P. et al. Two hundred gastrointestinal stromal tumors: recurrence patterns and prognostic factors for survival. Ann. Surg. 231, 51–58 (2000).
Demetri, G. D. et al. NCCN Task Force report: management of patients with gastrointestinal stromal tumor (GIST)—update of the NCCN clinical practice guidelines. J. Natl Compr. Canc. Netw. 5 (Suppl. 2), 1–9 (2007).
Hueman, M. T. & Schulick, R. D. Management of gastrointestinal stromal tumors. Surg. Clin. North Am. 88, 599–614 (2008).
Nilsson, B. et al. Adjuvant imatinib treatment improves recurrence-free survival in patients with high-risk gastrointestinal stromal tumours (GIST). Br. J. Cancer 96, 1656–1658 (2007).
Gilligan, C. J. et al. Gastric carcinoid tumors: the biology and therapy of an enigmatic and controversial lesion. Am. J. Gastroenterol. 90, 338–352 (1995).
Kloppel, G. et al. The gastroenteropancreatic neuroendocrine cell system and its tumors: the WHO classification. Ann. NY Acad. Sci. 1014, 13–27 (2004).
Kloppel, G. et al. Pathology and nomenclature of human gastrointestinal neuroendocrine (carcinoid) tumors and related lesions. World J. Surg. 20, 132–141 (1996).
Rindi, G. et al. ECL cell tumor and poorly differentiated endocrine carcinoma of the stomach: prognostic evaluation by pathological analysis. Gastroenterology 116, 532–542 (1999).
Rindi, G. et al. Gastric carcinoids and neuroendocrine carcinomas: pathogenesis, pathology, and behavior. World J. Surg. 20, 168–172 (1996).
Borch, K. et al. Gastric carcinoids: biologic behavior and prognosis after differentiated treatment in relation to type. Ann. Surg. 242, 64–73 (2005).
Modlin, I. M. et al. Gastric carcinoids. The Yale experience. Arch. Surg. 130, 250–255 (1995).
Schindl, M. et al. Treatment of gastric neuroendocrine tumors: the necessity of a type-adapted treatment. Arch. Surg. 136, 49–54 (2001).
Yi, S. Y. Dyslipidemia and H. pylori in gastric xanthomatosis. World J. Gastroenterol. 13, 4598–4601 (2007).
Lin, P. Y. et al. Gastric xanthelasma in hyperplastic gastric polyposis. Arch. Pathol. Lab. Med. 113, 428–430 (1989).
El-Serag, H. B. et al. Prevalence and determinants of histological abnormalities of the gastric cardia in volunteers. Scand. J. Gastroenterol. 42, 1158–1166 (2007).
Polkowski, W. et al. Intestinal and pancreatic metaplasia at the esophagogastric junction in patients without Barrett's esophagus. Am. J. Gastroenterol. 95, 617–625 (2000).
Christodoulidis, G. et al. Heterotopic pancreas in the stomach: a case report and literature review. World J. Gastroenterol. 13, 6098–6100 (2007).
Ormarsson, O. T. et al. Diagnosis and treatment of gastric heterotopic pancreas. World J. Surg. 30, 1682–1689 (2006).
Ayantunde, A. A. et al. Symptomatic pyloric pancreatic heterotopia: report of three cases and review of the literature. Med. Sci. Monit. 12, CS49–CS52 (2006).
Chetty, R. & Weinreb, I. Gastric neuroendocrine carcinoma arising from heterotopic pancreatic tissue. J. Clin. Pathol. 57, 314–317 (2004).
ASGE guideline: the role of endoscopy in the surveillance of premalignant conditions of the upper GI tract. National Guidelines Clearinghouse [online] (2009).
Acknowledgements
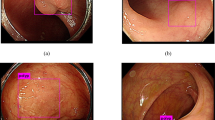
We would like to thank Dr A. Horiuchi, Showa Inan General Hospital, Komagane, Japan for providing the endoscopic photographs of a gastric adenoma (Figure 3a) and a gastric carcinoid (Figure 6a). Charles P. Vega, University of California, Irvine, CA, is the author of and is solely responsible for the content of the learning objectives, questions and answers of the Medscape-accredited continuing medical education activity associated with this article.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Rights and permissions
About this article
Cite this article
Carmack, S., Genta, R., Graham, D. et al. Management of gastric polyps: a pathology-based guide for gastroenterologists. Nat Rev Gastroenterol Hepatol 6, 331–341 (2009). https://doi.org/10.1038/nrgastro.2009.70
Published:
Issue Date:
DOI: https://doi.org/10.1038/nrgastro.2009.70
This article is cited by
-
Gastric villous adenoma: a case report and review of the literature
Journal of Medical Case Reports (2023)
-
Image-enhanced endoscopy for real-time differentiation between hyperplastic and fundic gland polyps in the stomach
Indian Journal of Gastroenterology (2022)
-
Polyps of Fundic Glands—a Second Glance
Current Treatment Options in Gastroenterology (2022)
-
Current Management of Benign Epithelial Gastric Polyps
Current Treatment Options in Gastroenterology (2017)
-
Gastric polyps diagnosed by double-contrast upper gastrointestinal barium X-ray radiography mostly arise from the Helicobacter pylori-negative stomach with low risk of gastric cancer in Japan
Gastric Cancer (2017)