Abstract
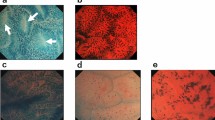
Despite advances in our knowledge of celiac disease, the most current and authoritative recommendations conclude that diagnosis requires at least four biopsy specimens to be taken from the duodenal area. These recommendations are based on the perception that classic endoscopic markers are not adequate to target biopsy sampling to sites of villous damage in the duodenum. In the past few years, newly developed procedures and technologies have improved endoscopic recognition of the duodenum. These advances make possible the real-time recognition of the duodenal villous pattern during an upper endoscopy procedure, and thereby have the potential to optimize diagnostic accuracy. It is, therefore, reasonable to hypothesize that upper endoscopy might have a more incisive role in the diagnosis of celiac disease than merely providing a means of obtaining biopsy specimens for histological analysis. This Review highlights the new technologies in the field of upper endoscopy that could be helpful for the diagnosis of celiac disease, including the water-immersion technique, chromoendoscopy, high-resolution magnification endoscopy, optimal band imaging, optical coherence tomography and confocal endomicroscopy.
Key Points
-
The gold standard for the diagnosis of celiac disease is the histological demonstration of characteristic pathological changes of the duodenal mucosa
-
The role of endoscopy is at present limited to obtaining a number of duodenal biopsies because of its low accuracy in predicting histological changes
-
Newly developed technologies in the field of gastrointestinal endoscopy make possible the real-time recognition of the duodenal villous pattern during upper endoscopy
-
Further investigations are needed to confirm encouraging preliminary reports of the use of newly developed endoscopic techniques in the diagnosis of celiac disease
-
The water-immersion technique, magnification endoscopy, optical band imaging, optical coherence tomography and confocal endomicroscopy demonstrate potential to have a more incisive role in the diagnosis of celiac disease
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
References
Green PH and Jabri B (2003) Coeliac disease. Lancet 362: 383–391
Mann JG et al. (1970) The subtle and variable clinical expressions of gluten-induced enteropathy (adult celiac disease, nontropical sprue): an analysis of twenty-one consecutive cases. Am J Med 48: 357–366
Rostom A et al. (2006) American Gastroenterological Association (AGA) Institute technical review on the diagnosis and management of celiac disease. Gastroenterology 131: 1981–2002
Rewers M (2005) Epidemiology of celiac disease: what are the prevalence, incidence, and progression of celiac disease. Gastroenterology 128 (Suppl 1): S47–S51
Dewar DH and Ciclitira PJ (2005) Clinical features and diagnosis of celiac disease. Gastroenterology 128 (Suppl 1): S19–S24
Green PH and Cellier C (2007) Celiac disease. N Engl J Med 357: 1731–1743
Marsh MN (1992) Gluten, major histocompatibility complex, and the small intestine: a molecular and immunobiologic approach to the spectrum of gluten sensitivity ('celiac sprue'). Gastroenterology 102: 330–354
Oberhuber G et al. (1999) The histopathology of celiac disease: time for a standardized report scheme for pathologists. Eur J Gastroenterol Hepatol 11: 1185–1194
Vogelsang H et al. (2001) Diagnostic duodenal bulb biopsy in celiac disease. Endoscopy 33: 336–340
Marsh MN and Crowe PT (1995) Morphology of the mucosal lesion in gluten sensitivity. Baillieres Clin Gastroenterol 9: 273–293
United European Gastroenterology (2001) When is a coeliac a coeliac? Report of a working group of the United European Gastroenterology Week in Amsterdam, 2001. Eur J Gastroenterol Hepatol 13: 1123–1128
Scott BB and Losowsky MS (1976) Patchiness and duodenal-jejunal variation of the mucosal abnormality in coeliac disease and dermatitis herpetiformis. Gut 17: 984–992
Bonamico M et al. (2004) Patchy villous atrophy of the duodenum in childhood celiac disease. J Pediatr Gastroenterol Nutr 38: 204–207
Manuel PD et al. (1979) Patchy enteropathy in childhood. Gut 20: 211–215
Ciclitira PJ et al. (1986) The effect of gluten on HLA-DR in the small intestinal epithelium of patients with coeliac disease. Clin Exp Immunol 63: 101–104
Ravelli A et al. (2005) Variability of histologic lesions in relation to biopsy site in gluten-sensitive enteropathy. Am J Gastroenterol 100: 177–185
Maurino E et al. (2003) Value of endoscopic markers in celiac disease. Dig Dis Sci 38: 2028–2033
Brocchi E et al. (2002) Endoscopic markers in adult coeliac disease. Digest Liver Dis 34: 177–182
Hopper AD et al. (2008) Patchy villous atrophy in adult patients with suspected gluten-sensitive enteropathy: is a multiple duodenal biopsy strategy appropriate?. Endoscopy 40: 219–225
Brocchi E et al. (1996) Unsuspected celiac disease diagnosed by endoscopic visualization of duodenal bulb micronodules. Gastrointest Endosc 44: 610–611
Cammarota G et al. (2007) Role of the “immersion technique” in diagnosing celiac disease with villous atrophy limited to the duodenal bulb. J Clin Gastroenterol 41: 571–575
Brocchi E et al. (1988) Endoscopic demonstration of loss of duodenal folds in the diagnosis of celiac disease. N Engl J Med 319: 741–744
Stevens FM and McCarthy CF (1976). The endoscopic demonstration of celiac disease. Endoscopy 8: 177–180
Corazza GR et al. (1990) Loss of duodenal folds allows diagnosis of unsuspected coeliac disease. Gut 31: 1080–1081
McIntyre AS et al. (1992) The endoscopic appearance of duodenal folds is predictive of untreated adult celiac disease. Gastrointest Endosc 38: 148–151
Smith AD et al. (1998) A prospective endoscopic study of scalloped folds and grooves in the mucosa of the duodenum as signs of villous atrophy. Gastrointest Endosc 47: 461–465
Magazzu G et al. (1994) Upper gastrointestinal endoscopy can be a reliable screening tool for celiac sprue in adults. J Clin Gastroenterol 19: 255–257
Dickey W and Hughes D (1999) Prevalence of coeliac disease and its endoscopic markers among patients having routine upper gastrointestinal endoscopy. Am J Gastroenterol 94: 2182–2186
Maurino E and Bai JC (2002) Endoscopic markers of celiac disease. Am J Gastroenterol 97: 760–761
Oxentenko AS et al. (2002) The insensitivity of endoscopic markers in celiac disease. Am J Gastroenterol 97: 933–938
Ravelli AM et al. (2001) Endoscopic features of celiac disease in children. Gastrointest Endosc 54: 736–742
Corazza GR et al. (1993) Scalloped duodenal folds in childhood celiac disease. Gastrointest Endosc 29: 543–545
Lecleire S et al. (2006) Endoscopic markers of villous atrophy are not useful for the detection of celiac disease in patients with dyspeptic symptoms. Endoscopy 38: 696–701
Bardella MT et al. (2000) Reevaluation of duodenal endoscopic markers in the diagnosis of celiac disease. Gastrointest Endosc 51: 714–716
Tursi A et al. (2002) Endoscopic features of celiac disease in adults and their correlation with age, histological damage, and clinical form of the disease. Endoscopy 34: 787–792
Shah VH et al. (2000) All that scallops is not celiac disease. Gastrointest Endosc 51: 717–720
Gasbarrini A et al. (2003) Lack of endoscopic visualization of intestinal villi with the “immersion technique” in overt atrophic celiac disease. Gastrointest Endosc 57: 348–351
Cammarota G et al. (2004) Reliability of the “immersion technique” during routine upper endoscopy for detection of abnormalities of duodenal villi in patients with dyspepsia. Gastrointest Endosc 60: 223–228
Cammarota G et al. (2007) A highly accurate method for monitoring histological recovery in patients with celiac disease on a gluten-free diet using an endoscopic approach that avoids the need for biopsy: a double-center study. Endoscopy 39: 46–51
Cammarota G et al.: The water-immersion technique during standard upper endoscopy may be useful to drive the biopsy sampling of duodenal mucosa in children with celiac disease. J Pediatr Gastroenterol Nutr, in press
Cammarota G et al. (2006) High accuracy and cost-effectiveness of a biopsy-avoiding endoscopic approach in diagnosing coeliac disease. Aliment Pharmacol Ther 23: 61–69
Lee SK and Green PH (2005) Endoscopy in celiac disease. Curr Opin Gastroenterol 21: 589–594
Wong Kee Song LM et al. for the ASGE Technology Committee (2007) Chromoendoscopy. Gastrointest Endosc 66: 639–649
Niveloni S et al. (1998) Usefulness of videoduodenoscopy and vital dye staining as indicators of mucosal atrophy of celiac disease: assessment of interobserver agreement. Gastrointest Endosc 47: 223–229
Rubio-Tapia A and Murray JA (2007) Novel endoscopic methods for the evaluation of the small-bowel mucosa. Gastrointest Endosc 66: 382–386
Bruno MJ (2003) Magnification endoscopy, high resolution endoscopy, and chromoscopy; towards a better optical diagnosis. Gut 52 (Suppl IV): S7–S11
Siegel LM et al. (1997) Combined magnification endoscopy with chromoendoscopy in the evaluation of patients with suspected malabsorption. Gastrointest Endosc 46: 226–230
Kiesslich R et al. (2003) Value of chromoendoscopy and magnification endoscopy in the evaluation of duodenal abnormalities: a prospective, randomized comparison. Endoscopy 35: 559–563
Badreldin R et al. (2005) How good is zoom endoscopy for assessment of villous atrophy in coeliac disease. Endoscopy 37: 994–998
Cammarota G et al. (2004) Direct visualization of intestinal villi by high-resolution magnifying upper endoscopy: a validation study. Gastrointest Endosc 60: 732–738
Cammarota G et al. (2005) High-resolution magnifying upper endoscopy in a patient with patchy celiac disease. Dig Dis Sci 50: 601–604
Banerjee R et al. (2007) Role of magnification endoscopy in the diagnosis and evaluation of suspected celiac disease: correlation with histology. Indian J Gastroenterol 26: 67–69
Lo A et al. (2007) Classification of villous atrophy with enhanced magnification endoscopy in patients with celiac disease and tropical sprue. Gastrointest Endosc 66: 377–382
Pohl J et al. (2007) Computed virtual chromoendoscopy: a new tool for enhancing tissue surface structures. Endoscopy 39: 80–83
Pohl J et al. (2007) Comparison of computed virtual chromoendoscopy and conventional chromoendoscopy with acetic acid for detection of neoplasia in Barrett's esophagus. Endoscopy 39: 594–598
Osawa H et al. (2008) Optimal band imaging system can facilitate detection of changes in depressed-type early gastric cancer. Gastrointest Endosc 67: 226–232
Pohl J et al. (2008) Computed virtual chromoendoscopy for classification of small colorectal lesions: a prospective comparative study. Am J Gastroenterol 103: 562–569
Cammarota G et al. (2008) Optimal band imaging system: a new tool for enhancing the duodenal villous pattern in celiac disease. Gastrointest Endosc 68: 352–357
van den Broek FJ et al. (2007) Review article: new developments in colonic imaging. Aliment Pharmacol Ther 26 (Suppl 2): S91–S99
Dekker E and Fockens P (2005) New imaging techniques at colonoscopy: tissue spectroscopy and narrow band imaging. Gastrointest Endosc Clin N Am 15: 703–714
Huang D et al. (1991) Optical coherence tomography. Science 254: 1178–1181
Tearney GJ et al. (1997) In vivo endoscopic optical biopsy with optical coherence tomography. Science 276: 2037–2039
Brand S et al. (2000) Optical coherence tomography in the gastrointestinal tract. Endoscopy 32: 796–803
Hsiung PL et al. (2005) Ultrahigh-resolution and 3-dimensional optical coherence tomography ex vivo imaging of the large and small intestines. Gastrointest Endosc 62: 561–574
Masci E et al. (2007) Pilot study on the correlation of optical coherence tomography with histology in celiac disease and normal subjects. J Gastroenterol Hepatol 22: 2256–2260
Odagi I et al. (2007) Examination of normal intestine using confocal endomicroscopy. J Gastroenterol Hepatol 22: 658–662
Hoffman A et al. (2006) Confocal laser endomicroscopy: technical status and current indications. Endoscopy 38: 1275–1283
Yoshida S et al. (2007) Optical biopsy of GI lesions by reflectance-type laser-scanning confocal microscopy. Gastrointest Endosc 66: 144–149
Sakashita M et al. (2003) Virtual histology of colorectal lesions using laser-scanning confocal microscopy. Endoscopy 35: 1033–1038
Nguyen NQ and Leong RWL (2008) Current application of confocal endomicroscopy in gastrointestinal disorders. J Gastroenterol Hepatol [10.1111/j.1440-1746.2008.05469.x]
Kiesslich R et al. (2006) In vivo histology of Barrett's oesophagus and associated neoplasia by confocal laser endomicroscopy. Clin Gastroenterol Hepatol 4: 979–987
Kiesslich R et al. (2004) Confocal laser endoscopy for diagnosing intraepithelial neoplasias and colorectal cancer in vivo. Gastroenterology 127: 706–713
Kiesslich R et al. (2007) Chromoscopy-guided endomicroscopy increases the diagnostic yield of intraepithelial neoplasia in ulcerative colitis. Gastroenterology 132: 874–882
Kakeji Y et al. (2006) Development and assessment of morphologic criteria for diagnosing gastric cancer using confocal endomicroscopy: an ex vivo and in vivo study. Endoscopy 38: 886–890
Polglase AL et al. (2005) A fluorescence confocal endomicroscope for in vivo microscopy of the upper- and the lower-GI tract. Gastrointest Endosc 62: 686–695
Zambelli A et al. (2007) Confocal laser endomicroscopy in celiac disease: description of findings in two cases. Endoscopy 39: 1018–1020
Trovato C et al. (2007) Celiac disease: in vivo diagnosis by confocal endomicroscopy. Gastrointest Endosc 65: 1096–1099
Cammarota G et al. (2008) The water immersion technique is easy to learn for routinely use during EGD for duodenal villous evaluation: a single centre 2-year experience. J Clin Gastroenterol [10.1097/MCG.0b013e318159c654]
Acknowledgements
Some of the material discussed in this Review is based on work supported in part by funds from the Italian Ministry for University, Scientific, and Technological Research.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Rights and permissions
About this article
Cite this article
Cammarota, G., Fedeli, P. & Gasbarrini, A. Emerging technologies in upper gastrointestinal endoscopy and celiac disease. Nat Rev Gastroenterol Hepatol 6, 47–56 (2009). https://doi.org/10.1038/ncpgasthep1298
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/ncpgasthep1298
This article is cited by
-
The potential role of optical biopsy in the study and diagnosis of environmental enteric dysfunction
Nature Reviews Gastroenterology & Hepatology (2017)
-
Celiac Disease or Non-Celiac Gluten Sensitivity? An Approach to Clinical Differential Diagnosis
American Journal of Gastroenterology (2014)
-
Évaluation endoscopique des patients atteints de maladie coeliaque
Acta Endoscopica (2014)
-
Detection of Villous Atrophy Using Endoscopic Images for the Diagnosis of Celiac Disease
Digestive Diseases and Sciences (2013)
-
Image-Enhanced Endoscopy with I-scan Technology for the Evaluation of Duodenal Villous Patterns
Digestive Diseases and Sciences (2013)