Key Points
-
The pancreatic β-cell is a key regulator of glucose homeostasis, sensing blood glucose levels after a meal and secreting insulin appropriately.
-
Loss of β-cell number and function feature prominently in both type 1 and type 2 diabetes.
-
Promoting β-cell regeneration, survival or function, especially with small molecules, may prove to be an effective strategy for treating diabetes.
-
β-cell regeneration can be accomplished by stimulating the division of existing β-cells. It will be important, however, to induce proliferation in a cell-specific manner to avoid oncogenic transformation.
-
Another mechanism for β-cell regeneration is through cellular reprogramming. Such transformations can occur from stem-cell-like populations (directed differentiation) or from other terminally differentiated cell types (transdifferentiation).
-
Prevention or slowing of β-cell death in the first place may avoid the loss of β-cell mass that enables the transition from insulin resistance to overt diabetes.
-
Promoting glucose-dependent induction of insulin secretion would restore hormone levels following β-cell death. Compounds exist to enhance insulin secretion, but many are not glucose-dependent.
-
Technical challenges to identifying novel compounds include a lack of many good human cell lines and the development of sophisticated techniques to measure β-cell function and number for high-throughput screening.
Abstract
Diabetes is a leading cause of morbidity and mortality worldwide, and predicted to affect over 500 million people by 2030. However, this growing burden of disease has not been met with a comparable expansion in therapeutic options. The appreciation of the pancreatic β-cell as a central player in the pathogenesis of both type 1 and type 2 diabetes has renewed focus on ways to improve glucose homeostasis by preserving, expanding and improving the function of this key cell type. Here, we provide an overview of the latest developments in this field, with an emphasis on the most promising strategies identified to date for treating diabetes by targeting the β-cell.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
Ashcroft, F. M. & Rorsman, P. Diabetes mellitus and the beta cell: the last ten years. Cell 148, 1160–1171 (2012).
Bluestone, J. A., Herold, K. & Eisenbarth, G. Genetics, pathogenesis and clinical interventions in type 1 diabetes. Nature 464, 1293–1300 (2010).
Butler, A. E. et al. Beta-cell deficit and increased beta-cell apoptosis in humans with type 2 diabetes. Diabetes 52, 102–110 (2003).
Ferrannini, E. The stunned beta cell: a brief history. Cell. Metab. 11, 349–352 (2010).
Samuel, V. T. & Shulman, G. I. Mechanisms for insulin resistance: common threads and missing links. Cell 148, 852–871 (2012).
Talchai, C., Lin, H. V., Kitamura, T. & Accili, D. Genetic and biochemical pathways of beta-cell failure in type 2 diabetes. Diabetes Obes. Metab. 11 (Suppl. 4), 38–45 (2009).
Dupuis, J. et al. New genetic loci implicated in fasting glucose homeostasis and their impact on type 2 diabetes risk. Nature Genet. 42, 105–116 (2010).
Scott, R. A. et al. Large-scale association analyses identify new loci influencing glycemic traits and provide insight into the underlying biological pathways. Nature Genet. 44, 991–1005 (2012). This landmark meta-analysis of >130,000 individuals identifies 53 genetic variants affecting glycaemic traits such as insulin secretion, and finds that many of these genetic variantsalso influence the risk of developing type 2 diabetes.
Sladek, R. et al. A genome-wide association study identifies novel risk loci for type 2 diabetes. Nature 445, 881–885 (2007).
Strawbridge, R. J. et al. Genome-wide association identifies nine common variants associated with fasting proinsulin levels and provides new insights into the pathophysiology of type 2 diabetes. Diabetes 60, 2624–2634 (2011).
Meier, J. J. et al. Beta-cell replication is the primary mechanism subserving the postnatal expansion of beta-cell mass in humans. Diabetes 57, 1584–1594 (2008).
Papa, F. R. Endoplasmic reticulum stress, pancreatic beta-cell degeneration, and diabetes. Cold Spring Harb. Perspect. Med. 2, a007666 (2012).
Eizirik, D. L. & Darville, M. I. Beta-cell apoptosis and defense mechanisms: lessons from type 1 diabetes. Diabetes 50 (Suppl. 1), 64–69 (2001).
Collombat, P. et al. The ectopic expression of Pax4 in the mouse pancreas converts progenitor cells into alpha and subsequently β cells. Cell 138, 449–462 (2009). This important study shows that α-cells can be reprogrammed to β-cells in vivo after the overexpression of PAX4.
Zhou, Q., Brown, J., Kanarek, A., Rajagopal, J. & Melton, D. A. In vivo reprogramming of adult pancreatic exocrine cells to β-cells. Nature 455, 627–632 (2008). This study shows that acinar tissue can be reprogrammed to β-cells in vivo after the overexpression of PDX1, NGN3 and MAFA.
Juhl, C. B. et al. Acute and short-term administration of a sulfonylurea (gliclazide) increases pulsatile insulin secretion in type 2 diabetes. Diabetes 50, 1778–1784 (2001).
Reers, C. et al. Impaired islet turnover in human donor pancreata with aging. Eur. J. Endocrinol. 160, 185–191 (2009).
Keenan, H. A. et al. Residual insulin production and pancreatic β-cell turnover after 50 years of diabetes: Joslin Medalist Study. Diabetes 59, 2846–2853 (2010). This investigation of islet samples from donors with type 1 diabetes reveals the existence of residual β-cells, even after decades of autoimmune diabetes, and gives rise to the promise that β-cell regeneration may be possible.
Cozar-Castellano, I. et al. Molecular control of cell cycle progression in the pancreatic β-cell. Endocr. Rev. 27, 356–370 (2006).
Heit, J. J., Karnik, S. K. & Kim, S. K. Intrinsic regulators of pancreatic β-cell proliferation. Annu. Rev. Cell Dev. Biol. 22, 311–338 (2006).
Lee, Y. C. & Nielsen, J. H. Regulation of beta cell replication. Mol. Cell Endocrinol. 297, 18–27 (2009).
Krishnamurthy, J. et al. p16INK4a induces an age-dependent decline in islet regenerative potential. Nature 443, 453–457 (2006).
Kohler, C. U. et al. Cell cycle control of β-cell replication in the prenatal and postnatal human pancreas. Am. J. Physiol. Endocrinol. Metab. 300, E221–E230 (2011).
Georgia, S. & Bhushan, A. p27 regulates the transition of β-cells from quiescence to proliferation. Diabetes 55, 2950–2956 (2006).
Kushner, J. A. et al. Cyclins D2 and D1 are essential for postnatal pancreatic β-cell growth. Mol. Cell. Biol. 25, 3752–3762 (2005).
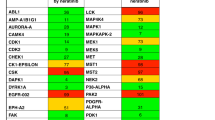
Fiaschi-Taesch, N. M. et al. Induction of human β-cell proliferation and engraftment using a single G1/S regulatory molecule, cdk6. Diabetes 59, 1926–1936 (2010). This analysis of cell-cycle regulators in human β-cells shows that selective proliferation of β-cells can be induced by the expression of CDK6.
Fiaschi-Taesch, N. M. et al. Human pancreatic β-cell G1/S molecule cell cycle atlas. Diabetes 62, 2450–2459 (2013).
Fiaschi-Taesch, N. M. et al. Cytoplasmic-nuclear trafficking of G1/S cell cycle molecules and adult human β-cell replication: a revised model of human beta-cell G1/S control. Diabetes 62, 2460–2470 (2013).
Rieck, S. & Kaestner, K. H. Expansion of β-cell mass in response to pregnancy. Trends Endocrinol. Metab. 21, 151–158 (2010).
Parsons, J. A., Brelje, T. C. & Sorenson, R. L. Adaptation of islets of Langerhans to pregnancy: increased islet cell proliferation and insulin secretion correlates with the onset of placental lactogen secretion. Endocrinology 130, 1459–1466 (1992).
Chen, G. et al. Molecular mechanism of pancreatic β-cell adaptive proliferation: studies during pregnancy in rats and in vitro. Endocrine 39, 118–127 (2011).
Tamura, K. et al. Stress response gene ATF3 is a target of c-myc in serum-induced cell proliferation. EMBO J. 24, 2590–2601 (2005).
Kim, H. et al. Serotonin regulates pancreatic beta cell mass during pregnancy. Nature Med. 16, 804–808 (2010).
Gylfe, E. Serotonin as marker for the secretory granules in the pancreatic beta-cell. Acta Physiol. Scand. Suppl. 452, 125–128 (1977).
Butler, A. E. et al. Adaptive changes in pancreatic beta cell fractional area and beta cell turnover in human pregnancy. Diabetologia 53, 2167–2176 (2010).
Michael, M. D. et al. Loss of insulin signaling in hepatocytes leads to severe insulin resistance and progressive hepatic dysfunction. Mol. Cell 6, 87–97 (2000).
El Ouaamari, A. et al. Liver-derived systemic factors drive β cell hyperplasia in insulin-resistant states. Cell Rep. 3, 401–410 (2013).
Salpeter, S. J. et al. Systemic regulation of the age-related decline of pancreatic β-cell replication. Diabetes 62, 2843–2848 (2013).
Yi, P., Park, J. S. & Melton, D. A. Betatrophin: a hormone that controls pancreatic β cell proliferation. Cell 153, 747–758 (2013).
Chen, H. et al. Polycomb protein Ezh2 regulates pancreatic β-cell Ink4a/Arf expression and regeneration in diabetes mellitus. Genes Dev. 23, 975–985 (2009).
Zeng, N. et al. Pten controls β-cell regeneration in aged mice by regulating cell cycle inhibitor p16ink4a. Aging Cell 12, 1000–1011 (2013).
Bernal-Mizrachi, E. et al. Defective insulin secretion and increased susceptibility to experimental diabetes are induced by reduced Akt activity in pancreatic islet β cells. J. Clin. Invest. 114, 928–936 (2004).
Holst, L. S. et al. Protein kinase B is expressed in pancreatic β cells and activated upon stimulation with insulin-like growth factor I. Biochem. Biophys. Res. Commun. 250, 181–186 (1998).
Liu, W., Chin-Chance, C., Lee, E. J. & Lowe, W. L. Jr. Activation of phosphatidylinositol 3-kinase contributes to insulin-like growth factor I-mediated inhibition of pancreatic β-cell death. Endocrinology 143, 3802–3812 (2002).
Tuttle, R. L. et al. Regulation of pancreatic β-cell growth and survival by the serine/threonine protein kinase Akt1/PKBalpha. Nature Med. 7, 1133–1137 (2001).
Vetere, A. & Wagner, B. K. Chemical methods to induce beta-cell proliferation. Int. J. Endocrinol. 2012, 925143 (2012).
Shen, W. et al. Small-molecule inducer of β cell proliferation identified by high-throughput screening. J. Am. Chem. Soc. 135, 1669–1672 (2013).
Annes, J. P. et al. Adenosine kinase inhibition selectively promotes rodent and porcine islet β-cell replication. Proc. Natl Acad. Sci. USA 109, 3915–3920 (2012).
Andersson, O. et al. Adenosine signaling promotes regeneration of pancreatic β cells in vivo. Cell. Metab. 15, 885–894 (2012).
Oh, S. M. et al. Ebp1 sumoylation, regulated by TLS/FUS E3 ligase, is required for its anti-proliferative activity. Oncogene 29, 1017–1030 (2010).
Squatrito, M., Mancino, M., Donzelli, M., Areces, L. B. & Draetta, G. F. EBP1 is a nucleolar growth-regulating protein that is part of pre-ribosomal ribonucleoprotein complexes. Oncogene 23, 4454–4465 (2004).
Andres, C. M. & Fox, I. H. Purification and properties of human placental adenosine kinase. J. Biol. Chem. 254, 11388–11393 (1979).
Rovira, M. et al. Chemical screen identifies FDA-approved drugs and target pathways that induce precocious pancreatic endocrine differentiation. Proc. Natl Acad. Sci. USA 108, 19264–19269 (2011).
Jacovetti, C. et al. MicroRNAs contribute to compensatory β cell expansion during pregnancy and obesity. J. Clin. Invest. 122, 3541–3551 (2012).
Lynn, F. C. et al. MicroRNA expression is required for pancreatic islet cell genesis in the mouse. Diabetes 56, 2938–2945 (2007).
Joglekar, M. V., Joglekar, V. M. & Hardikar, A. A. Expression of islet-specific microRNAs during human pancreatic development. Gene Expr. Patterns 9, 109–113 (2009).
Poy, M. N. et al. A pancreatic islet-specific microRNA regulates insulin secretion. Nature 432, 226–230 (2004).
Guay, C., Roggli, E., Nesca, V., Jacovetti, C. & Regazzi, R. Diabetes mellitus, a microRNA-related disease? Transl. Res. 157, 253–264 (2011).
Lovis, P., Gattesco, S. & Regazzi, R. Regulation of the expression of components of the exocytotic machinery of insulin-secreting cells by microRNAs. Biol. Chem. 389, 305–312 (2008).
Wang, Y., Liu, J., Liu, C., Naji, A. & Stoffers, D. A. MicroRNA-7 regulates the mTOR pathway and proliferation in adult pancreatic β-cells. Diabetes 62, 887–895 (2013).
Bravo-Egana, V. et al. Quantitative differential expression analysis reveals miR-7 as major islet microRNA. Biochem. Biophys. Res. Commun. 366, 922–926 (2008).
Correa-Medina, M. et al. MicroRNA miR-7 is preferentially expressed in endocrine cells of the developing and adult human pancreas. Gene Expr. Patterns 9, 193–199 (2009).
van de Bunt, M. et al. The miRNA profile of human pancreatic islets and beta-cells and relationship to type 2 diabetes pathogenesis. PLoS ONE 8, e55272 (2013).
Chaparro, R. J., Burton, A. R., Serreze, D. V., Vignali, D. A. & DiLorenzo, T. P. Rapid identification of MHC class I-restricted antigens relevant to autoimmune diabetes using retrogenic T cells. J. Immunol. Methods 335, 106–115 (2008).
DiLorenzo, T. P. & Serreze, D. V. The good turned ugly: immunopathogenic basis for diabetogenic CD8+ T cells in NOD mice. Immunol. Rev. 204, 250–263 (2005).
Concannon, P., Rich, S. S. & Nepom, G. T. Genetics of type 1A diabetes. N. Engl. J. Med. 360, 1646–1654 (2009).
Santin, I. & Eizirik, D. L. Candidate genes for type 1 diabetes modulate pancreatic islet inflammation and beta-cell apoptosis. Diabetes Obes. Metab. 15 (Suppl. 3), 71–81 (2013).
Cardozo, A. K. et al. IL-1β and IFN-γ induce the expression of diverse chemokines and IL-15 in human and rat pancreatic islet cells, and in islets from pre-diabetic NOD mice. Diabetologia 46, 255–266 (2003).
Pearl-Yafe, M. et al. Pancreatic islets under attack: cellular and molecular effectors. Curr. Pharm. Des. 13, 749–760 (2007).
Yoon, J. W. & Jun, H. S. Autoimmune destruction of pancreatic beta cells. Am. J. Ther. 12, 580–591 (2005).
Bobbala, D. et al. Interleukin-15 plays an essential role in the pathogenesis of autoimmune diabetes in the NOD mouse. Diabetologia 55, 3010–3020 (2012).
Monti, P. et al. Islet transplantation in patients with autoimmune diabetes induces homeostatic cytokines that expand autoreactive memory T cells. J. Clin. Invest. 118, 1806–1814 (2008).
Varanasi, V., Avanesyan, L., Schumann, D. M. & Chervonsky, A. V. Cytotoxic mechanisms employed by mouse T cells to destroy pancreatic β-cells. Diabetes 61, 2862–2870 (2012).
Thomas, H. E., Trapani, J. A. & Kay, T. W. The role of perforin and granzymes in diabetes. Cell Death Differ. 17, 577–585 (2010).
Eizirik, D. L. & Mandrup-Poulsen, T. A choice of death — the signal-transduction of immune-mediated β-cell apoptosis. Diabetologia 44, 2115–2133 (2001).
Allison, J., Thomas, H. E., Catterall, T., Kay, T. W. & Strasser, A. Transgenic expression of dominant-negative Fas-associated death domain protein in β cells protects against Fas ligand-induced apoptosis and reduces spontaneous diabetes in nonobese diabetic mice. J. Immunol. 175, 293–301 (2005).
Kawasaki, E., Abiru, N. & Eguchi, K. Prevention of type 1 diabetes: from the view point of beta cell damage. Diabetes Res. Clin. Pract. 66 (Suppl. 1), 27–32 (2004).
McKenzie, M. D. et al. Proapoptotic BH3-only protein Bid is essential for death receptor-induced apoptosis of pancreatic β-cells. Diabetes 57, 1284–1292 (2008).
Cardozo, A. K. et al. A comprehensive analysis of cytokine-induced and nuclear factor-κB-dependent genes in primary rat pancreatic β-cells. J. Biol. Chem. 276, 48879–48886 (2001).
Cnop, M. et al. Mechanisms of pancreatic beta-cell death in type 1 and type 2 diabetes: many differences, few similarities. Diabetes 54 (Suppl. 2), 97–107 (2005). This classic review describes the differences in the pathophysiology of type 1 and type 2 diabetes.
Moore, F. et al. STAT1 is a master regulator of pancreatic β-cell apoptosis and islet inflammation. J. Biol. Chem. 286, 929–941 (2011).
Barthson, J. et al. Tumor necrosis factor-α and interferon-γ induce pancreatic β-cell apoptosis through STAT1-mediated Bim activation. J. Biol. Chem. 286, 39632–39643 (2011).
Ortis, F. et al. Induction of nuclear factor-κB and its downstream genes by TNF-α and IL-1β has a pro-apoptotic role in pancreatic β cells. Diabetologia 51, 1213–1225 (2008).
Holohan, C., Szegezdi, E., Ritter, T., O'Brien, T. & Samali, A. Cytokine-induced β-cell apoptosis is NO-dependent, mitochondria-mediated and inhibited by BCL-XL . J. Cell. Mol. Med. 12, 591–606 (2008).
Eldor, R. et al. Conditional and specific NF-κB blockade protects pancreatic β cells from diabetogenic agents. Proc. Natl Acad. Sci. USA 103, 5072–5077 (2006).
Lee, J. H. et al. Overexpression of SIRT1 protects pancreatic β-cells against cytokine toxicity by suppressing the nuclear factor-κB signaling pathway. Diabetes 58, 344–351 (2009).
Callewaert, H. I. et al. Deletion of STAT-1 pancreatic islets protects against streptozotocin-induced diabetes and early graft failure but not against late rejection. Diabetes 56, 2169–2173 (2007).
Kim, E. K. et al. Inhibitory effect of Artemisia capillaris extract on cytokine-induced nitric oxide formation and cytotoxicity of RINm5F cells. Int. J. Mol. Med. 19, 535–540 (2007).
Kim, E. K. et al. Coptidis rhizoma extract protects against cytokine-induced death of pancreatic β-cells through suppression of NF-κB activation. Exp. Mol. Med. 39, 149–159 (2007).
Menegazzi, M. et al. Protective effects of St. John's wort extract and its component hyperforin against cytokine-induced cytotoxicity in a pancreatic β-cell line. Int. J. Biochem. Cell Biol. 40, 1509–1521 (2008).
Song, M. Y. et al. Radix asari extract protects pancreatic β cells against cytokine-induced toxicity: implication of the NF-κB-iNOS signaling cascade. Int. J. Mol. Med. 20, 769–775 (2007).
Bonny, C., Oberson, A., Negri, S., Sauser, C. & Schorderet, D. F. Cell-permeable peptide inhibitors of JNK: novel blockers of β-cell death. Diabetes 50, 77–82 (2001).
Ablamunits, V. et al. Synergistic reversal of type 1 diabetes in NOD mice with anti-CD3 and interleukin-1 blockade: evidence of improved immune regulation. Diabetes 61, 145–154 (2012).
Sandberg, J. O., Andersson, A., Eizirik, D. L. & Sandler, S. Interleukin-1 receptor antagonist prevents low dose streptozotocin induced diabetes in mice. Biochem. Biophys. Res. Commun. 202, 543–548 (1994).
Moran, A. et al. Interleukin-1 antagonism in type 1 diabetes of recent onset: two multicentre, randomised, double-blind, placebo-controlled trials. Lancet 381, 1905–1915 (2013).
Cavelti-Weder, C. et al. Effects of gevokizumab on glycemia and inflammatory markers in type 2 diabetes. Diabetes Care 35, 1654–1662 (2012).
Larsen, C. M. et al. Interleukin-1-receptor antagonist in type 2 diabetes mellitus. N. Engl. J. Med. 356, 1517–1526 (2007).
Sloan-Lancaster, J. et al. Double-blind, randomized study evaluating the glycemic and anti-inflammatory effects of subcutaneous LY2189102, a neutralizing IL-1β antibody, in patients with type 2 diabetes. Diabetes Care 36, 2239–2246 (2013).
Larsen, L. et al. Inhibition of histone deacetylases prevents cytokine-induced toxicity in β cells. Diabetologia 50, 779–789 (2007).
Lewis, E. C. et al. The oral histone deacetylase inhibitor ITF2357 reduces cytokines and protects islet β-cells in vivo and in vitro. Mol. Med. 17, 369–377 (2010).
Patel, T., Patel, V., Singh, R. & Jayaraman, S. Chromatin remodeling resets the immune system to protect against autoimmune diabetes in mice. Immunol. Cell Biol. 89, 640–649 (2011).
Chou, D. H. et al. Inhibition of histone deacetylase 3 protects beta cells from cytokine-induced apoptosis. Chem. Biol. 19, 669–673 (2012).
Lundh, M. et al. Histone deacetylases 1 and 3 but not 2 mediate cytokine-induced beta cell apoptosis in INS-1 cells and dispersed primary islets from rats and are differentially regulated in the islets of type 1 diabetic children. Diabetologia 55, 2421–2431 (2012).
Chou, D. H. et al. Small-molecule suppressors of cytokine-induced β-cell apoptosis. ACS Chem. Biol. 5, 729–734 (2010).
Chou, D. H. et al. Synthesis of a novel suppressor of beta-cell apoptosis via diversity-oriented synthesis. ACS Med. Chem. Lett. 2, 698–702 (2011).
Scully, S. S. et al. Small-molecule inhibitors of cytokine-mediated STAT1 signal transduction in β-cells with improved aqueous solubility. J. Med. Chem. 56, 4125–4129 (2013).
Eizirik, D. L., Cardozo, A. K. & Cnop, M. The role for endoplasmic reticulum stress in diabetes mellitus. Endocr. Rev. 29, 42–61 (2008).
Wang, H., Kouri, G. & Wollheim, C. B. ER stress and SREBP-1 activation are implicated in β-cell glucolipotoxicity. J. Cell Sci. 118, 3905–3915 (2005).
Poitout, V. & Robertson, R. P. Glucolipotoxicity: fuel excess and β-cell dysfunction. Endocr. Rev. 29, 351–366 (2008).
Rhodes, C. J. Type 2 diabetes-a matter of β-cell life and death? Science 307, 380–384 (2005).
Robertson, R. P., Harmon, J., Tran, P. O. & Poitout, V. Beta-cell glucose toxicity, lipotoxicity, and chronic oxidative stress in type 2 diabetes. Diabetes 53 (Suppl. 1), 119–124 (2004).
Hotamisligil, G. S. Endoplasmic reticulum stress and the inflammatory basis of metabolic disease. Cell 140, 900–917 (2010).
Mussmann, R. et al. Inhibition of GSK3 promotes replication and survival of pancreatic beta cells. J. Biol. Chem. 282, 12030–12037 (2007).
Stukenbrock, H. et al. 9-cyano-1-azapaullone (cazpaullone), a glycogen synthase kinase-3 (GSK-3) inhibitor activating pancreatic β cell protection and replication. J. Med. Chem. 51, 2196–2207 (2008).
Wagman, A. S., Johnson, K. W. & Bussiere, D. E. Discovery and development of GSK3 inhibitors for the treatment of type 2 diabetes. Curr. Pharm. Des. 10, 1105–1137 (2004).
Lablanche, S. et al. Protection of pancreatic INS-1 β-cells from glucose- and fructose-induced cell death by inhibiting mitochondrial permeability transition with cyclosporin A or metformin. Cell Death Dis. 2, e134 (2011).
Cnop, M., Hannaert, J. C. & Pipeleers, D. G. Troglitazone does not protect rat pancreatic β cells against free fatty acid-induced cytotoxicity. Biochem. Pharmacol. 63, 1281–1285 (2002).
Finegood, D. T. et al. β-cell mass dynamics in Zucker diabetic fatty rats. Rosiglitazone prevents the rise in net cell death. Diabetes 50, 1021–1029 (2001).
Han, S. J. et al. Rosiglitazone inhibits early stage of glucolipotoxicity-induced beta-cell apoptosis. Horm. Res. 70, 165–173 (2008).
Higa, M. et al. Troglitazone prevents mitochondrial alterations, β cell destruction, and diabetes in obese prediabetic rats. Proc. Natl Acad. Sci. USA 96, 11513–11518 (1999).
Shimabukuro, M., Zhou, Y. T., Lee, Y. & Unger, R. H. Troglitazone lowers islet fat and restores beta cell function of Zucker diabetic fatty rats. J. Biol. Chem. 273, 3547–3550 (1998).
Weir, G. C., Cavelti-Weder, C. & Bonner-Weir, S. Stem cell approaches for diabetes: towards beta cell replacement. Genome Med. 3, 61 (2011).
Chen, S. et al. A small molecule that directs differentiation of human ESCs into the pancreatic lineage. Nature Chem. Biol. 5, 258–265 (2009). This study reports a screen for compounds that can induce the differentiation of mouse embryonic stem cells to pancreatic progenitors.
Tang, D. Q. et al. In vitro generation of functional insulin-producing cells from human bone marrow-derived stem cells, but long-term culture running risk of malignant transformation. Am. J. Stem Cells 1, 114–127 (2012).
Wang, Q. et al. Reprogramming of bone marrow-derived mesenchymal stem cells into functional insulin-producing cells by chemical regimen. Am. J. Stem Cells 1, 128–137 (2012).
Takahashi, K. & Yamanaka, S. Induction of pluripotent stem cells from mouse embryonic and adult fibroblast cultures by defined factors. Cell 126, 663–676 (2006).
Hou, P. et al. Pluripotent stem cells induced from mouse somatic cells by small-molecule compounds. Science 341, 651–654 (2013).
Kroon, E. et al. Pancreatic endoderm derived from human embryonic stem cells generates glucose-responsive insulin-secreting cells in vivo. Nature Biotech. 26, 443–452 (2008). This paper describesthe ex vivo generation of a β-cell population that can be transplanted into patients with diabetes, which would represent an important therapeutic advance in regenerative medicine. This study demonstrates the differentiation of human embryonic stem cells into β-cells and their use in mice.
Schulz, T. C. et al. A scalable system for production of functional pancreatic progenitors from human embryonic stem cells. PLoS ONE 7, e37004 (2012).
Wagner, B. K. Grand challenge commentary: chemical transdifferentiation and regenerative medicine. Nature Chem. Biol. 6, 877–879 (2010).
Spijker, H. S. et al. Conversion of mature human β-cells into glucagon-producing α-cells. Diabetes 62, 2471–2480 (2013).
Bramswig, N. C. et al. Epigenomic plasticity enables human pancreatic α to β cell reprogramming. J. Clin. Invest. 123, 1275–1284 (2013). This analysis of the epigenetic state of α- and β-cells suggests that there is a more bivalent state in α-cells, and points to histone methylation as a potential therapeutic target for cellular reprogramming.
Dorrell, C. et al. Isolation of mouse pancreatic alpha, beta, duct and acinar populations with cell surface markers. Mol. Cell Endocrinol. 339, 144–150 (2011).
Dorrell, C. et al. Transcriptomes of the major human pancreatic cell types. Diabetologia 54, 2832–2844 (2011).
Collombat, P. et al. Opposing actions of Arx and Pax4 in endocrine pancreas development. Genes Dev. 17, 2591–2603 (2003).
Al-Hasani, K. et al. Adult duct-lining cells can reprogram into β-like cells able to counter repeated cycles of toxin-induced diabetes. Dev. Cell 26, 86–100 (2013).
Yang, Y. P., Thorel, F., Boyer, D. F., Herrera, P. L. & Wright, C. V. Context-specific α- to-β-cell reprogramming by forced Pdx1 expression. Genes Dev. 25, 1680–1685 (2011).
Thorel, F. et al. Conversion of adult pancreatic α-cells to β-cells after extreme β-cell loss. Nature 464, 1149–1154 (2010).
Xu, X. et al. Beta cells can be generated from endogenous progenitors in injured adult mouse pancreas. Cell 132, 197–207 (2008).
Swales, N. et al. Plasticity of adult human pancreatic duct cells by neurogenin3-mediated reprogramming. PLoS ONE 7, e37055 (2012).
Kim, H. S. et al. Activin A, exendin-4, and glucose stimulate differentiation of human pancreatic ductal cells. J. Endocrinol. 217, 241–252 (2013).
Akinci, E., Banga, A., Greder, L. V., Dutton, J. R. & Slack, J. M. Reprogramming of pancreatic exocrine cells towards a beta (β) cell character using Pdx1, Ngn3 and MafA. Biochem. J. 442, 539–550 (2012).
Stumvoll, M., Goldstein, B. J. & van Haeften, T. W. Type 2 diabetes: principles of pathogenesis and therapy. Lancet 365, 1333–1346 (2005).
Barnett, A. H. et al. Key considerations around the risks and consequences of hypoglycaemia in people with type 2 diabetes. Int. J. Clin. Pract. 64, 1121–1129 (2010).
Bolen, S. et al. Systematic review: comparative effectiveness and safety of oral medications for type 2 diabetes mellitus. Ann. Intern. Med. 147, 386–399 (2007).
Matschinsky, F. M. & Ellerman, J. E. Metabolism of glucose in the islets of Langerhans. J. Biol. Chem. 243, 2730–2736 (1968).
Matschinsky, F. M. Assessing the potential of glucokinase activators in diabetes therapy. Nature Rev. Drug Discov. 8, 399–416 (2009).
Matschinsky, F. M. et al. Glucokinase activators for diabetes therapy: May 2010 status report. Diabetes Care 34 (Suppl. 2), 236–243 (2011).
Rees, M. G. & Gloyn, A. L. Small molecular glucokinase activators: has another new anti-diabetic therapeutic lost favour? Br. J. Pharmacol. 168, 335–338 (2013).
Briscoe, C. P. et al. Pharmacological regulation of insulin secretion in MIN6 cells through the fatty acid receptor GPR40: identification of agonist and antagonist small molecules. Br. J. Pharmacol. 148, 619–628 (2006).
Ahren, B. Islet G protein-coupled receptors as potential targets for treatment of type 2 diabetes. Nature Rev. Drug Discov. 8, 369–385 (2009). This is an excellent summary of our current understanding of GPCRs in the β-cell and the therapeutic implications of this important class of proteins.
Burant, C. F. et al. TAK-875 versus placebo or glimepiride in type 2 diabetes mellitus: a phase 2, randomised, double-blind, placebo-controlled trial. Lancet 379, 1403–1411 (2012).
Morris, A. P. et al. Large-scale association analysis provides insights into the genetic architecture and pathophysiology of type 2 diabetes. Nature Genet. 44, 981–990 (2012).
Saxena, R. et al. Large-scale gene-centric meta-analysis across 39 studies identifies type 2 diabetes loci. Am. J. Hum. Genet. 90, 410–425 (2012).
Zeggini, E. et al. Meta-analysis of genome-wide association data and large-scale replication identifies additional susceptibility loci for type 2 diabetes. Nature Genet. 40, 638–645 (2008).
Billings, L. K. & Florez, J. C. The genetics of type 2 diabetes: what have we learned from GWAS? Ann. NY Acad. Sci. 1212, 59–77 (2010). This is a concise overview of the findings emerging from human genetic studies of type 2 diabetes, highlighting the prominent role of the pancreatic β-cell in this disease.
Florez, J. C. Newly identified loci highlight beta cell dysfunction as a key cause of type 2 diabetes: where are the insulin resistance genes? Diabetologia 51, 1100–1110 (2008).
Voight, B. F. et al. Twelve type 2 diabetes susceptibility loci identified through large-scale association analysis. Nature Genet. 42, 579–589 (2010).
Wijesekara, N. et al. Beta cell-specific Znt8 deletion in mice causes marked defects in insulin processing, crystallisation and secretion. Diabetologia 53, 1656–1668 (2010).
Tamaki, M. et al. The diabetes-susceptible gene SLC30A8/ZnT8 regulates hepatic insulin clearance. J. Clin. Invest. 123, 4513–4524 (2013).
Nicolson, T. J. et al. Insulin storage and glucose homeostasis in mice null for the granule zinc transporter ZnT8 and studies of the type 2 diabetes-associated variants. Diabetes 58, 2070–2083 (2009).
Saxena, R. et al. Genome-wide association analysis identifies loci for type 2 diabetes and triglyceride levels. Science 316, 1331–1336 (2007).
Zeggini, E. et al. Replication of genome-wide association signals in UK samples reveals risk loci for type 2 diabetes. Science 316, 1336–1341 (2007).
Scott, L. J. et al. A genome-wide association study of type 2 diabetes in Finns detects multiple susceptibility variants. Science 316, 1341–1345 (2007).
Wei, F. Y. et al. Deficit of tRNALys modification by Cdkal1 causes the development of type 2 diabetes in mice. J. Clin. Invest. 121, 3598–3608 (2011).
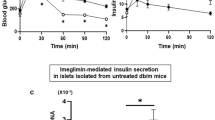
Wu, W. et al. Identification of glucose-dependant insulin secretion targets in pancreatic β cells by combining defined-mechanism compound library screening and siRNA gene silencing. J. Biomol. Screen. 13, 128–134 (2008).
Lee, J. A. et al. Open innovation for phenotypic drug discovery: the PD2 assay panel. J. Biomol. Screen. 16, 588–602 (2011).
Ku, G. M., Pappalardo, Z., Luo, C. C., German, M. S. & McManus, M. T. An siRNA screen in pancreatic beta cells reveals a role for Gpr27 in insulin production. PLoS Genet. 8, e1002449 (2012).
Hill, J. A. et al. A multi-parameter, high-content, high-throughput screening platform to identify natural compounds that modulate insulin and Pdx1 expression. PLoS ONE 5, e12958 (2010).
Kalisky, T., Blainey, P. & Quake, S. R. Genomic analysis at the single-cell level. Annu. Rev. Genet. 45, 431–445 (2011).
Tang, F., Lao, K. & Surani, M. A. Development and applications of single-cell transcriptome analysis. Nature Methods 8, S6–11 (2011).
Segal, D. J. & Meckler, J. F. Genome engineering at the dawn of the golden age. Annu. Rev. Genom. Hum. Genet. 14, 135–158 (2013).
Ravassard, P. et al. A genetically engineered human pancreatic β cell line exhibiting glucose-inducible insulin secretion. J. Clin. Invest. 121, 3589–3597 (2011). The lack of a human β-cell line has hampered advances in research, and the development of this research tool has thus been a major goal of the community. This study reports the development of a new glucose-responsive human β-cell line.
Holliday, N. D., Watson, S. J. & Brown, A. J. Drug discovery opportunities and challenges at G protein coupled receptors for long chain free fatty acids. Front. Endocrinol. 2, 112 (2011).
Martinez, A., Castro, A., Dorronsoro, I. & Alonso, M. Glycogen synthase kinase 3 (GSK-3) inhibitors as new promising drugs for diabetes, neurodegeneration, cancer, and inflammation. Med. Res. Rev. 22, 373–384 (2002).
Santin, I. et al. PTPN2, a candidate gene for type 1 diabetes, modulates pancreatic β-cell apoptosis via regulation of the BH3-only protein Bim. Diabetes 60, 3279–3288 (2011).
Yuan, Y. et al. A small-molecule inducer of PDX1 expression identified by high-throughput screening. Chem. Biol. 20, 1513–1522 (2013).
Acknowledgements
The authors would like to thank D. Altshuler and S. Schreiber for their ongoing support.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
B.K.W. is a co-founder of KDAc Therapeutics, which is focused on some of the principles outlined in this Review.
Supplementary information
Supplementary information S1 (table)
Human genetic loci linked to type 2 diabetes and the indicated associated traits. (PDF 219 kb)
Glossary
- Genome-wide association studies
-
(GWASs). Studies that examine the common genetic variants across case and control populations, and determine statistical correlation with a disease or phenotypic traits. GWASs can be conducted on complex genetic diseases, such as type 2 diabetes, as well as on traits such as fasting glucose levels or insulin secretion.
- Pancreatic β-cell mass
-
The β-cell population present in the pancreas that, under physiological conditions, results from the balance between growth (from replication, neogenesis and cell size) and cell death (from apoptosis, necrosis and autophagy).
- ER stress
-
A physiological event activated in response to an accumulation of unfolded or misfolded proteins in the lumen of the endoplasmic reticulum (ER). ER stress has two primary aims: to restore normal function of the cell by halting protein translation, and to activate the signalling pathways that lead to an increase in the production of the molecular chaperones involved in protein folding.
- Oxidative stress
-
The effect of an imbalance between the production of reactive oxygen species and the ability of biological systems to detoxify the reactive intermediates or to repair the resulting damage.
- Glucolipotoxicity
-
Elevated levels of glucose and fatty acids that contribute to β-cell dysfunction and death.
- Zucker diabetic fatty rats
-
A rat model of type 2 diabetes containing a mutation of the leptin receptor.
- Induced pluripotent stem cell
-
(iPSC). A type of pluripotent stem cell that can be generated directly from adult cells. Efforts to generate these cells have ranged from genetic to chemical, and combinations of both.
- Cellular transdifferentiation
-
The conversion of one terminally differentiated cell state to another. This process can also be thought of as a subset of cellular reprogramming, because cells can be reprogrammed by dedifferentiation followed by directed differentiation to a new cell state.
- Secretagogues
-
Stimuli that induce insulin secretion from β-cells. Secretagogues include small molecules, such as the sulphonylurea class of drugs, peptide growth factors and glucose itself.
- Glucose-stimulated insulin secretion
-
The process by which β-cells sense and secrete insulin in response to a glucose challenge. β-cells are uniquely engineered to carry out this role, and this function is considered the gold standard of β-cell identity. Glucose-stimulated insulin secretion involves specialized signalling pathways and secretion machinery. In many cases of partial cellular reprogramming, this function is the one that is not fully achieved.
- HOMA-B
-
Homeostatic model assessment of β-cell function. A method to estimate the steady-state β-cell function of an individual relative to a non-diabetic reference population, based on fasting measurements of plasma glucose and plasma insulin.
- HOMA-IR
-
Homeostatic model assessment of insulin resistance. A method to estimate the steady-state insulin resistance of an individual relative to a non-diabetic reference population, based on fasting measurements of plasma glucose and plasma insulin.
Rights and permissions
About this article
Cite this article
Vetere, A., Choudhary, A., Burns, S. et al. Targeting the pancreatic β-cell to treat diabetes. Nat Rev Drug Discov 13, 278–289 (2014). https://doi.org/10.1038/nrd4231
Published:
Issue Date:
DOI: https://doi.org/10.1038/nrd4231
This article is cited by
-
Discovery of IHMT-MST1-39 as a novel MST1 kinase inhibitor and AMPK activator for the treatment of diabetes mellitus
Signal Transduction and Targeted Therapy (2023)
-
MST1 deletion protects β-cells in a mouse model of diabetes
Nutrition & Diabetes (2022)
-
RNA aptamers specific for transmembrane p24 trafficking protein 6 and Clusterin for the targeted delivery of imaging reagents and RNA therapeutics to human β cells
Nature Communications (2022)
-
The Hippo kinase LATS2 impairs pancreatic β-cell survival in diabetes through the mTORC1-autophagy axis
Nature Communications (2021)
-
Therapeutic potentials of agonist and antagonist of adenosine receptors in type 2 diabetes
Reviews in Endocrine and Metabolic Disorders (2021)