Abstract
Safe and effective stroke prevention in atrial fibrillation (AF) is crucial as the number of patients with this condition continues to increase. Several novel oral anticoagulants are being developed as replacements for warfarin for this indication. Direct factor Xa inhibitors comprise the largest class of oral anticoagulants in development; the inhibition of factor Xa is recognized to be a promising target for therapeutic anticoagulation, partly because of its location in the coagulation cascade. Apixaban, betrixaban, edoxaban, and rivaroxaban are small-molecule, selective inhibitors that directly and reversibly bind to the active site of factor Xa. Their pharmacokinetic and pharmacodynamic profiles vary, which might allow patient-specific therapy. Several of these agents have been tested in clinical trials for various indications, including AF, with favorable results. In particular, apixaban and rivaroxaban have shown superiority and noninferiority, respectively, to warfarin in phase III clinical trials for stroke prevention in AF. These agents have also been shown to be safe in terms of bleeding risk. Despite these advantages, factor Xa inhibitors have several characteristics, such as potential interactions with other drugs (inhibitors of cytochrome P450 and P-glycoprotein) and the inability to reverse their anticoagulant effects, as well as concerns about poor patient compliance, which must be considered when initiating patients on a novel factor Xa inhibitor.
Key Points
-
Vitamin K antagonists, such as warfarin, are difficult to manage and, therefore, often underused for stroke prevention in patients with atrial fibrillation (AF)
-
Direct factor Xa inhibitors are the largest class of novel oral anticoagulants in development; several phase III clinical trials have been completed with these agents for stroke prevention in AF
-
In a phase III trial, rivaroxaban was noninferior to warfarin for the prevention of stroke or systemic embolism, without a significant difference in major bleeding
-
In a phase III trial, apixaban was superior to warfarin for the prevention of stroke or systemic embolism, with a significant decrease in major bleeding and all-cause mortality
-
Oral factor Xa inhibitors present several clinical challenges (inability to reverse their anticoagulant effects, poor patient compliance, and the need for monitoring), which must be considered when selecting therapy
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Miyasaka, Y. et al. Secular trends in incidence of atrial fibrillation in Olmstead County, Minnesota, 1980–2000, and implications on the projections for future prevalence. Circulation 114, 119–125 (2006).
Hylek, E. M. et al. Effect of intensity of oral anticoagulation on stroke severity and mortality in atrial fibrillation. N. Engl. J. Med. 349, 1019–1026 (2003).
Hart, R. G., Benavente, O., McBride, R. & Pearce, L. A. Antithrombotic therapy to prevent stroke in patients with atrial fibrillation: a meta-analysis. Ann. Intern. Med. 131, 492–501 (1999).
Waldo, A. L., Becker, R. C., Tapson, V. F. & Colgan, K. J. Hospitalized patients with atrial fibrillation and a high risk of stroke are not being provided with adequate anticoagulation. J. Am. Coll. Cardiol. 46, 1729–1736 (2005).
Ansell, J. et al. Pharmacology and management of the vitamin K antagonists: American College of Chest Physicians evidence-based clinical practice guidelines (8th edition). Chest 133 (Suppl. 6), 160S–198S (2008).
Singer, D. E. et al. Antithrombotic therapy in atrial fibrillation: American College of Chest Physicians evidence-based clinical practice guidelines (8th edition). Chest 133 (Suppl. 6), 546S–592S (2008).
Ogilvie, I. M., Newton, N., Welner, S. A., Cowell, W. & Lip, G. Y. H. Under use of oral anticoagulants in atrial fibrillation; a systematic review. Am. J. Med. 123, 638–645 (2010).
Wisler, J. W. & Becker, R. C. Oral factor Xa inhibitors for the long-term management of ACS. Nat. Rev. Cardiol. http://dx.doi.org/10.1038/nrcardio.2012.18.
Butenas, S. & Mann, K. G. Kinetics of human factor VII activation. Biochemistry 36, 1904–1910 (1996).
Alexander, J. H. & Singh, K. P. Inhibition of factor Xa: a potential target for the development of new anticoagulants. Am. J. Cardiovasc. Drugs 5, 279–290 (2005).
Eriksson, B. I., Quinlan, D. J. & Weitz, J. I. Comparative pharmacodynamics and pharmacokinetics of oral direct thrombin and factor Xa inhibitors in development. Clin. Pharmacokinet. 48, 1–22 (2009).
Bauer, K. A. New anticoagulants: anti IIa vs. anti Xa—is one better? J. Thromb. Thrombolysis 21, 67–72 (2006).
Rai, R., Sprengeler, P. A., Elrod, K. C. & Young, W. B. Perspectives on factor Xa inhibition. Curr. Med. Chem. 8, 101–119 (2001).
Kubitza, D., Becka, M., Wensing, G., Voith, B. & Zuehlsdorf, M. Safety, pharmacodynamics, and pharmacokinetics of BAY 59–7939—an oral, direct factor Xa inhibitor—after multiple dosing in healthy male subjects. Eur. J. Clin. Pharmacol. 61, 873–880 (2005).
Turpie, A. G. G. New oral anticoagulants in atrial fibrillation. Eur. Heart J. 29, 155–165 (2007).
Eriksson, B. I. et al. Rivaroxaban versus enoxaparin for thromboprophylaxis after hip arthroplasty. N. Engl. J. Med. 358, 2765–2775 (2008).
Kakkar, A. K. et al. Extended duration rivaroxaban versus short-term enoxaparin for the prevention of venous thromboembolism after total hip arthroplasty: a double-blind, randomized controlled trial. Lancet 372, 31–39 (2008).
Lassen, M. R. et al. Rivaroxaban versus enoxaparin for thromboprophylaxis after total knee arthroplasty. N. Engl. J. Med. 358, 2776–2786 (2008).
Turpie, A. G. G. et al. Rivaroxaban versus enoxaparin for thromboprophylaxis after total knee arthroplasty (RECORD 4): a randomized trial. Lancet 373, 1673–1680 (2009).
Turpie, A. G. G. et al. A pooled analysis of four pivotal studies of rivaroxaban for the prevention of venous thromboembolism after orthopedic surgery: effect on symptomatic venous thromboembolism, death, and bleeding [abstract 36]. Blood 112, 18–19 (2008).
Cohen, A. T. Rivaroxaban compared with enoxaparin for the prevention of venous thromboembolism in acutely ill medical patients. American Heart Association [online], (2011).
ROCKET AF study investigators. Rivaroxaban—once daily, oral, direct factor Xa inhibition compared with vitamin K antagonism for prevention of stroke and embolism trial in atrial fibrillation: rationale and design of the ROCKET AF study. Am. Heart J. 159, 340–347 (2010).
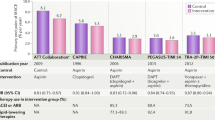
Patel, M. R. et al. Rivaroxaban versus warfarin in nonvalvular atrial fibrillation. N. Engl. J. Med. 365, 883–891 (2011).
US Department of Health and Human Sciences. FDA approves Xarelto to prevent stroke in people with common type of abnormal heart rhythm [online], (2011).
Fleming, T. R. & Emerson, S. S. Evaluating rivaroxaban for nonvalvular atrial fibrillation—regulatory considerations. N. Engl. J. Med. 365, 1557–1559 (2011).
Connolly, S. J. et al. Dabigatran versus warfarin in patients with atrial fibrillation. N. Engl. J. Med. 361, 1139–1151 (2009).
Lassen, M. et al. Apixaban or enoxaparin for thromboprophylaxis after knee replacement. N. Engl. J. Med. 361, 594–604 (2009).
Lassen, M. R., Gallus, A. S., Pineo, G. F. & Raskob, G. E. The ADVANCE 2 study: a randomized double-blind trial comparing apixaban with enoxaparin for thromboprophylaxis after total knee replacement [abstract]. J. Thromb. Haemost. 7 (Suppl. 2), LB-MO-005 (2009).
US National Library of Medicine. ClinicalTrials.gov [online], (2011).
US National Library of Medicine. ClinicalTrials.gov [online], (2012).
US National Library of Medicine. ClinicalTrials.gov [online], (2012).
US National Library of Medicine. ClinicalTrials.gov [online], (2010).
Ufer, M. Comparative efficacy and safety of the novel oral anticoagulants dabigatran, rivaroxaban and apixaban in preclinical and clinical development. Thromb. Haemost. 103, 572–585 (2010).
Connolly, S. J. et al. Apixaban in patients with atrial fibrillation. N. Engl. J. Med. 364, 806–817 (2011).
Lopes, R. D. et al. Apixaban for Reduction In Stroke and Other Thromboembolic Events in Atrial Fibrillation (ARISTOTLE) trial: design and rationale. Am. Heart J. 159, 131–139 (2010).
Granger, C. B. et al. Apixaban versus warfarin in patients with atrial fibrillation. N. Engl. J. Med. 365, 981–992 (2011).
Masumoto, H. et al. In vitro metabolism of edoxaban and the enzymes involved in the oxidative metabolism of edoxaban [online], (2012).
Eikelboom, J. W. & Weitz, J. I. New anticoagulants. Circulation 121, 1523–1532 (2010).
Fuji, T., Fujita, S., Tachibana, S. & Kawai, Y. Randomized, double blind, multi-dose efficacy, safety and biomarker study of the oral factor Xa inhibitor DU-176b compared with placebo for prevention of venous thromboembolism in patients after total knee arthroplasty [abstract]. Blood 112, a34 (2008).
Raskob, G. et al. Randomized, double blind, multi-dose trial of the oral factor Xa inhibitor DU-176b versus LMW heparin (dalteparin) for the prevention of venous thromboembolism after total hip replacement [abstract]. Eur. Heart J. 29 (Abstract Suppl.) a609 (2008).
Weitz J. L. et al. Randomized, parallel group, multicentre, multinational phase 2 study comparing edoxaban, an oral factor Xa inhibitor, with warfarin for stroke prevention in patients with atrial fibrillation. Thromb. Haemost. 104, 633–641 (2010).
Ruff, C. T. et al. Evaluation of the novel factor Xa inhibitor edoxaban compared with warfarin in patients with atrial fibrillation: Design and rationale for the Effective aNticoaGulation with factor xA next Generation in Atrial Fibrillation—Thrombolysis in Myocardial Infarction study 48 (ENGAGE AF-TIMI 48). Am. Heart J. 160, 635–641 (2010).
Ezekowitz, M. D. et al. A phase 2, randomized, parallel group, dose-finding, multicenter, multinational study of the safety, tolerability and pilot efficacy of three blinded doses of the oral factor Xa inhibitor betrixaban compared with open-label dose-adjusted warfarin in patients with non-valvular atrial fibrillation (EXPLORE-Xa) [online], (2010).
Khoo, C. W., Tay, K. H., Shantsila, E. & Lip, G. Novel oral anticoagulants. Int. J. Clin. Pract. 63, 630–641 (2009).
Portola Pharmaceuticals. PRT064445: FXa Inhibitor Antidote [online], (2011).
Janssen. Xarelto® (rivaroxaban) tablets, for oral use: prescribing information [online], (2011).
Gruber, A., Marzec, U. M., Buetehorn, U., Hanson, S. & Perzborn, E. Potential of activated prothrombin complex concentrate and activated factor VII to reverse the anticoagulant effects of rivaroxaban in primates [abstract 3825]. Blood 112, 1307 (2008).
Eerenberg, E. S. et al. Reversal of rivaroxaban and dabigatran by prothrombin complex concentrate: a randomized, placebo-controlled, crossover study in health subjects. Circulation 124, 1573–1579 (2011).
Lu, G. et al. Recombinant antidote for reversal of anticoagulation by factor Xa inhibitors [abstract 983]. Blood 112, 362 (2008).
Yasuda, K. et al. Interaction of cytochrome P450 3A inhibitors with P-glycoprotein. J. Pharm. Exp. Ther. 303, 323–332 (2002).
Lin, J. H., Yamazaki, M. Role of P-glycoprotein in pharmacokinetics: clinical implications. Clin. Pharmacokinet. 42, 59–98 (2003).
Walenga, J. M. & Adiguzel, C. Drug and dietary interactions of the new and emerging oral anticoagulants. Int. J. Clin. Pract. 64, 956–967 (2010).
Weitz, J. I., Hirsch, J. & Samama, M. M. New antithrombotic drugs: American College of Chest Physicians evidence-based clinical practice guidelines (8th edition). Chest 133 (Suppl. 6), 234S–256S (2008).
DiMatteo, M. R. et al. Patient adherence and medical treatment outcomes: a meta-analysis. Med. Care 40, 794–811 (2002).
Cramer, J. A. Partial medication compliance: the enigma in poor medical outcomes. Am. J. Manag. Care 1, 167–174 (1995).
Sullivan, S. D., Kreling, D. H., Hazlet, T. K. Noncompliance with medication regimens and subsequent hospitalizations: a literature analysis and cost of hospitalization estimate. J. Res. Pharm. Econ. 2, 19–33 (1990).
Dunbar-Jacob, J. et al. Adherence in chronic disease, in Annual Review of Nursing Research 18th edn (eds Fitzpatric, J. J. & Goeppinger, J.) 48–90 (Springer, New York, 2000).
Kimmel, S. E. et al. The influence of patient adherence on anticoagulation control with warfarin: results from the International Normalized Ratio Adherence and Genetics (IN-RANGE) Study. Arch. Intern. Med. 167, 229–235 (2007).
Ansell, J. E. Optimizing the efficacy and safety of oral anticoagulant therapy: high quality dose management, anticoagulation clinics, and patient self-management. Semin. Vas. Med. 3, 261–269 (2003).
Author information
Authors and Affiliations
Contributions
Both authors contributed substantially to researching this article, discussion of its content, and writing, reviewing, and editing the manuscript before submission.
Corresponding author
Ethics declarations
Competing interests
J. Ansell is, or has been, a consultant for Boehringer Ingelheim, Bristol–Myers Squibb, Daiichi Sankyo, and Janssen. K. P. Cabral declares no competing interests.
Rights and permissions
About this article
Cite this article
Cabral, K., Ansell, J. Oral direct factor Xa inhibitors for stroke prevention in atrial fibrillation. Nat Rev Cardiol 9, 385–391 (2012). https://doi.org/10.1038/nrcardio.2012.19
Published:
Issue Date:
DOI: https://doi.org/10.1038/nrcardio.2012.19
This article is cited by
-
Pleiotropic effects of NOACs with focus on edoxaban: scientific findings and potential clinical implications
Herzschrittmachertherapie + Elektrophysiologie (2023)
-
From basic science to life-saving therapy: the rationale, and drug discovery efforts that led to the direct factor Xa inhibitor eliquis
Journal of Thrombosis and Thrombolysis (2021)
-
Oral factor Xa inhibitors for the long-term management of ACS
Nature Reviews Cardiology (2012)