Abstract
The inclusion of sex as a biological variable in research is absolutely essential for improving our understanding of disease mechanisms contributing to risk and resilience. Studies focusing on examining sex differences have demonstrated across many levels of analyses and stages of brain development and maturation that males and females can differ significantly. This review will discuss examples of animal models and clinical studies to provide guidance and reference for the inclusion of sex as an important biological variable relevant to a Neuropsychopharmacology audience.
Similar content being viewed by others
INTRODUCTION
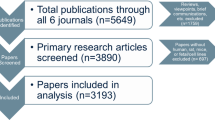
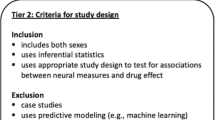
An appreciation for sex as a biological variable (SABV) in preclinical and clinical research is essential for our understanding of basic mechanisms contributing to disease risk and resilience, especially in cases where there are known sex differences in phenomenology, natural history, treatment, or severity. Studies focusing on examining sex differences have demonstrated across many levels of analyses and stages of brain development and maturation that males and females can differ significantly. From sex chromosomes that allow for disparities in gene dosage and regulatory mechanisms, to the important role of gonadal hormones across the life span, our appreciation for the unique and highly mechanistic insight that including SABV affords us has gained great attention. This review will provide general oversight as to animal models and clinical studies that have demonstrated novel outcomes because both sexes were examined across research areas and human health and disease relevant to a Neuropsychopharmacology audience. This is by no means a comprehensive review of all research in these areas, but rather a selection of appropriate and representative examples to provide guidance and reference for the inclusion of sex as an important biological variable. In addition, we have included several helpful out-takes as reference and citation for the ‘benefits of’ and the ‘how to’ complete studies in this area in preclinical and clinical research (Box 1; Figures 1 and 2). Finally, the role of developmental windows and changes across the life span to the contribution of sex differences in neuropsychiatric and cognitive disorders is highlighted where appropriate and in Figure 3.
How to examine menstrual cycle impact in human studies. Depicted is an idealized 28-day cycle, although studies for which menstrual cycle length is considered frequently include women with regular cycles from 25 to 34 days in length from day 1 (first day of menstrual flow) to day 1 (first day of menstrual flow) of the next cycle. If necessary, varying cycle lengths can be modified statistically to conform to a standardized 28-day cycle. However, the most straightforward way to assess changes in outcomes across the cycle or between phases is to target when a given women is likely to be in the hormonal and/or behavioral state of interest (Epperson et al, 2007; Comasco et al, 2014; Timby et al, 2016). Many women will have several days of spotting before experiencing a full flow. Whether investigators choose to consider any spotting as day 1 or onset of full flow as day 1 varies, but should remain consistent within a given study.
Sex differences in gonadal and pituitary hormones in middle- and late-aged adults. Data depicting general fluctuations in reproductive hormones across the life span from the typical age of late pre-menopause to the late post-menopause in women and age-matched men (Moroz and Verkhratsky, 1985; Liu et al, 2015). A rapid effect is indicated by two arrows. A slow or moderate effect on gonadal and pituitary hormones is indicated by one arrow.
Sex and gender differences across the life span. Based on preclinical and clinical research: (a) maternal and paternal life experience can impact fetal programming and offspring behavior in a sex-specific manner (Bale and Epperson, 2015; Rodgers and Bale, 2015). (b) Postpartum depression is associated with behavioral differences in female and male infants and young children (Azak, 2012; Kingston et al, 2012). (c) Neuropsychiatric conditions are more common among prepubertal males than prepubertal females. Limited early life stress may lead to resilience to depression among women (Zahn-Waxler et al, 2008). (d) Onset of sex differences in affective disorders and female-specific mood disorders at puberty. Ovarian hormones modulate brain neurochemistry, structure, and function (Shanmugan and Epperson, 2014; Hantsoo and Epperson, 2015). (e) Prenatal stress contributes to risk for diseases that exhibit sex differences across the life span (Goldstein et al, 2014). (f) Mid-life is associated with marked hormonal shifts for women, but not men. Estradiol effects on stress responses varies in pre- vs post-menopausal women (Dumas et al, 2012; Albert et al, 2015). (g) Females are at greater risk of dementia and adverse effects of many pharmacologic agents used in the treatment of adult disorders (Parekh et al, 2011; Franconi et al, 2012; Spoletini et al, 2012).
Defining Sex and Gender
Although all cells have a sex, designated by the presence and dosage of X or Y chromosomes, which in most cases will be XX (female) or XY (male), gender is a designated societal determinant and therefore traditionally described only in humans (Bachmann and Mussman, 2015). Of particular importance for this discussion, rodents do not have a gender. Discussed below are the primary contributions of gonadal hormones and sex chromosomes in organizing the sexually dimorphic brain, a key foundation throughout life where the internal and external environments can provoke phenotypic sex differences.
Importantly, the sexually dimorphic brain, similar to most sex differences, does not fall into a hard binary readout—but rather is on a continuum or spectrum with each cell and each brain region comprised of varying degrees of ‘male’ and ‘female’ (Hines, 2005; Joel and McCarthy, 2016). This is because the influences from very early neurodevelopmental time points, and perhaps even earlier than fertilization, are complex and multifaceted and frequently depend on the sex chromosome compliment of the individual or the sex of the parent contributing a given gene. Finally, the combination of genetic sex and gonadal hormones alone can produce a plethora of points at which subtle differences promote dramatic trajectory changes in development.
An example of this is from Catherine Dulac’s group in which they investigated the genetics of sex differences in the brain by comparing parent-of-origin allelic gene expression and found that imprinted genes inherited from maternal or paternal origin were dependent on the offspring sex as well (Gregg et al, 2010). Within the neuroendocrine hypothalamus, this study showed that there was an important interaction at the level of epigenetic modifications in controlling gene expression patterns between parent and offspring sex. At a very molecular level, this is an incredible example of where the same parents, the same environment, and the same gestational experience can yield significantly different outcomes in brain development that may then predict long-term sex differences in disease risk and resilience.
Also, critical to the discussion of sex and gender in the human laboratory is the interaction between an individual’s experiences, based upon society’s concept of their gender, and the developing central nervous system (Borchers and Gershwin, 2012; Springer et al, 2012). Examples of this phenomenon include opportunities for education and enrichment, exposures to particular types of trauma and injury, and access to and uptake of behavioral health treatment. It is well know that education is important to long-term cognitive health and although women in the United States now outnumber men with respect to graduate degrees, women in some communities are not encouraged to seek higher education and overall health status is adversely impacted (Hendi, 2015). Likewise, females are more likely than males to experience sexual abuse during critical periods of brain development and maturation, particularly during peri-adolescence when sub-cortical structures are vulnerable to insult (Felitti et al, 1998). Although gender differences in sports-related concussions vary by type of sport, females show higher rates of concussion than males in gender-comparable sports, and female sex is a risk factor for post-concussion neuropsychiatric sequelae (Marar et al, 2012; King, 2014). Finally, women are more likely than men to seek medical care and to be exposed to pharmacologic treatment, particularly psychotropic agents that may adversely impact neurological, cognitive, and sexual function (Whitley and Lindsey, 2009). These latter two examples of sports-related concussions and medication utilization are particularly relevant to the thesis of this review in that they illustrate how behavioral factors under the rubric of gender interact with sex with respect to health outcomes, suggesting that in clinical research the role of both gender and sex are frequently relevant.
The observation that female sex is a risk factor for a wide range of adverse drug reactions bears additional discussion given the readership and mission of this Journal with respect to pharmacology (Parekh et al, 2011; Franconi et al, 2012; Spoletini et al, 2012). Early limitations on recruitment of women to randomized clinical trials and the delay in considering SABV in drug studies have resulted in a number of cautionary tales. Findings from the Physicians’ Health Study that included over 20 000 male physicians studied in the 1980s, indicated that low-dose aspirin was associated with a reduced risk of myocardial infarction and a slight increased risk of stroke (1989). It was decades later that a follow-up study conducted in 39 000 female participants showed alarmingly disparate findings. In females, low-dose aspirin was associated with a greater risk of stroke with no overall effect on risk for myocardial infarction (Ridker et al, 2005). Although the 1993 NIH policy encouraging the inclusion of women in clinical trials has contributed to a more equal number of males and females in phase III trials, examination of medication efficacy and adverse drug reactions by sex are still lacking, leading to continued evidence of increased risk for women (Mazure and Jones, 2015). Referable to this point, in 2013 the FDA-approved labeling changes for dosing of zolpidem, a drug approved for the short-term treatment of insomnia decades earlier. The recommended starting dose was reduced in women, as metabolism of the drug is slower in females, leading to higher drug concentrations and morning drowsiness in women compared with men. In fact, governmental reports indicate that out of the 10 prescription drugs removed from the US market between 1997 and 2001, 8 were found to have greater adverse effects in women compared with men.
Although our understanding of SABV in many disease states has been hindered by factors from limited financial and physical resources to the belief that sex differences are not important or do not exist (Cahill, 2014), research examining how SABV applies to transgender populations is nonexistent for most medical conditions. Although this topic is of growing and critical importance, the current review focuses primarily on SABV in organisms/individuals for whom the gonadal hormonal milieu is consistent with their chromosomal sex.
Sex Differences Related to Sex Chromosomes and Hormones and the Importance of Timing
Importantly, the mammalian brain develops in the face of combined and opposing forces contributing to resiliency or vulnerability. The sexually dimorphic developing brain is organized in large part by developmental hormone exposure, with males experiencing elevated testosterone levels during the process of normal testes development, largely in utero, although the exact timing of this is species-dependent. Aromatization of this testosterone to estradiol in the brain drives masculinization, an active process affecting cell differentiation and connectivity in the brain in rodents (Figure 4; McCarthy, 1994; McCarthy, 2016). Estrogenic involvement in cell death and cell birth in the developing nervous system is a critical component in programming the sexually dimorphic brain, as is the epigenetic process of DNA methylation in feminization of the female brain (McCarthy et al, 2009; Nugent et al, 2015). Aromatization of testosterone to estradiol occurs in primates, including humans, but does not necessarily have a major role in masculinization of the primate brain. Instead, both testicular production of testosterone and intact androgen receptors are necessary to defeminize the human brain as evidenced by the feminine phenotype of XY individuals with complete androgen insensitivity syndrome and masculine phenotype of those with aromatase dysfunction (Imperato-McGinley et al, 1982; Grumbach and Auchus, 1999). Certainly, evidence in humans also suggests a strong correlation between fetal testosterone levels and steroidogenic activity with neurodevelopmental disease risk and adult cognitive and behavioral stress reactivity, supporting the importance of the processes involved in establishing the sexually dimorphic brain (Chura et al, 2010; Lombardo et al, 2012; Lombardo et al, 2012; Baron-Cohen et al, 2015). Programming of important regulatory brain regions, including the neuroendocrine hypothalamus, via such steroid hormone effects on cell migration patterns during early development likely also contributes to sex differences in how the individual responds to environmental perturbations throughout life (Bale et al, 2010).
Masculinization of the male brain. In most mammalian species, testosterone is produced by the testes during testes development in late gestation. The presence of testes results from the testis-determining factor, Sry, on the Y chromosome that determines the direction the bipotential gonad develops. Circulating testosterone enters the brain and is aromatized to estradiol during this critical organizational window. Estradiol produces hosts of cellular effects to then ‘masculinize’ the male brain.
In rodent models, studies have been able to manipulate this critical organizational window to mechanistically examine its importance in sex differences in long-term stress programming. For instance, adult sex differences in hippocampal expression of the glucocorticoid receptor, critical for the negative feedback and modulation of the HPA stress axis, was disrupted in females masculinized at birth by a single injection of testosterone, supporting the importance of the male testosterone surge in normal wiring of sex differences in stress pathways (Bingham and Viau, 2008; Goel and Bale, 2008; Goel et al, 2011). In addition to this early critical period of programming, the rise in gonadal hormones beginning in puberty interacts with these organizational changes and exerts modulatory actions on neurotransmitter systems critical in regulation of sex differences in stress responsivity. Ultimately then, this is an excellent example of how an important coordination must occur between organizational and activational periods of hormone exposure with additional factors from the sex chromosomes to orchestrate a ‘normal’ stress phenotype for each sex. Therefore, neuropsychiatric disease predisposition may result from a mismatch between these processes due to perturbations during early development (Karatsoreos and McEwen, 2013; Karatsoreos and McEwen, 2013; Pembrey et al, 2014).
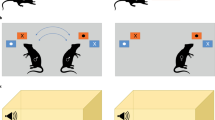
Not surprisingly, chromosomal sex also contributes to brain development in a hormone-independent manner. The four core genotype mice in which the testis-determining gene, Sry, has been removed from the Y chromosome and is now autosomal, are an interesting tool with which measured outcomes can differentiate sex chromosome complement from gonadal sex (Quinn et al, 2007; Arnold, 2009). The ‘four core genotypes’ refer to the production of mice that are one of four genotypes—XXsry, XX, XYsry, and XY. Studies using these mice have provided a unique and innovative strategy by which labs with interests from addiction to reproductive behaviors have been able to address important questions regarding sex differences independent of gonadal hormones. For example, Jane Taylor’s group, as discussed below, has used these mice to uncover a critical role of sex chromosomes in producing significant differences in food-reinforced habit formation and goal-directed behaviors dependent on the presence of two X chromosomes, and independent of gonadal hormone status (Quinn et al, 2007; Barker et al, 2010). Thus, from these animal studies, we learned that behaviors relevant to diseases such as addiction and obesity are affected by X-linked genes and can be independent of gonadal hormones. Such findings are critical to consider particularly in the context of hypogonadal states, which characterize the prepubertal and postmenopausal windows, or in the context of exogenous use of reproductive hormones that are inconsistent with the individual’s chromosomal sex.
Studies of individuals born with sex chromosome compliments that do not conform to XX or XY have informed our understanding of the individual role of the X and Y chromosome in human brain development. Neuroimaging studies comparing children in early puberty with Turner syndrome (XO) and Klinefelter’s syndrome (XXY) to age-matched controls, indicate a dose-dependency of the X chromosome to decreased parieto-occipital and increased temporo-insular gray matter volumes (Hong et al, 2014; Hong and Reiss, 2014). A similar study also reported smaller hippocampal volumes in XXY boys compared with age-matched controls (Rose et al, 2004). Interestingly, XYY karyotypes that do not present with a detectable phenotype have normal behavior and cognitive abilities, and normal serum testosterone levels, suggesting that, although the dosage of X-linked genes is important in normal development, this may not be the case for Y-linked genes. However, it should be noted that it is inherently difficult to completely dissect the gonadal hormone and sex chromosome effects on the developing brain as both XO and XXY children are also typically deficient in gonadal hormone production. Further, the testis-determining factor, Sry, as discussed above, is a Y chromosome gene and a necessary transcription factor for the bipotential gonad to develop into a testis, a necessity for testosterone production during neonatal and pubertal developmental organizational periods (Capel, 1998).
We know that the timing or ‘critical periods’ of brain development and maturation demarcate points where the plastic brain undergoes marked changes that can be distinctly feminine or masculine. It is within these sexually dimorphic nuclei that cells are increasing or decreasing in size, synapse and glia numbers changing, and dendritic spines sprouting at a rapid rate—all of which point to a robust and dynamic state. Therefore, sex-specific changes may present an opportunity where the normal trajectory becomes most vulnerable to influences that can be redirected or reprogrammed. For instance, in both humans and rodents, several brain regions involved in stress and corticotropin-releasing factor (CRF)-mediated HPA axis regulation and emotional affect, such as the prefrontal cortex (PFC), amygdala, and hippocampus undergo significant maturation during childhood and adolescence. These areas also demonstrate significant sex differences in both structure and function into adulthood, and may be related to varying rates of maturation between males and females.
Recent findings from the Philadelphia Neurodevelopmental Cohort reveal significant nonlinear effects of sex and age/pubertal development on cerebral perfusion with pre- and peri-adolescent females having lower cerebral blood flow (CBF), but by mid-adolescence (15–17 years old) males were lower, and by late-adolescence (17–22 years old) CBF in females began increasing with age (Satterthwaite et al, 2014). These sex differences in CBF were most pronounced in the default mode network, executive system, and regions critical to affective processing. CBF, a critical property of basic brain physiology, has been shown to vary by sex in older adults, is linked to regional brain metabolism, is altered by cognitive activity and load, and is abnormal in various neuropsychiatric conditions (reviewed by Satterthwaite et al (2014)). Sex differences in such a fundamental aspect of brain physiology emphasize the consideration not only of SABV but also of developmental trajectories when conducting human neuroimaging research. Reproductive hormones have pronounced impact on systemic and central vasculature and thus cerebral perfusion, which is particularly important in research focusing on CNS damage under conditions of ischemia (Sorensen et al, 2001). Considering the later end of the life span when cerebral vascular disease and risk for ischemia are more likely, McCollough, Arnold, and colleagues research using the four core genotype mouse model (described above) indicates that sex differences in ischemic stroke sensitivity is influenced primarily by circulating gonadal hormones, not sex chromosome compliment (Manwani et al, 2015). Estradiol supplementation was associated with robust CNS protection in an ischemic stroke model in females, while the effect was muted in males, suggesting that both organizational and activational effects of reproductive hormones should be considered under this context.
Similarly, structural neuroimaging studies in humans emphasize the importance of considering SABV and development when considering the integrity of critical limbic structures such as the amygdala, hippocampus, and PFC. Amygdala volume increases significantly more in adolescent boys, whereas hippocampal volume increases faster in girls, especially within the CA1 subfield (Satterthwaite et al, 2014). Moreover, the thinning of frontal cortical gray matter associated with adolescence occurs earlier in females, which may be related to an earlier onset of puberty. Interestingly, these same limbic and forebrain regions are also extremely sensitive to stress (McEwen and Morrison, 2013). As glucocorticoids are potent modulators of synaptic function and plasticity, it is likely that exposure to stressors during adolescence or impaired CRF pathway function could shape these limbic brain areas critical to emotionality, possibly in a sex-dependent manner given their different rates of maturation (Goel and Bale, 2009).
Unfortunately, little is known regarding the ability of stress across the pubertal transition to alter the developmental trajectory of these brain regions in males and females. In humans, studies have shown the impact of preadolescent stress as being particularly critical for adult right amygdala volumes, with adversity (abuse, neglect, and family stress) occurring at age 11 years, contributing to a 3.5-fold effect above adversity occurring at any other time from birth to 18 years of age (Pechtel et al, 2014). Numerous studies show that alterations in amygdala volume are related to negative emotionality (anxiety, depression, and neuroticism), which characterize psychiatric conditions for which there are prominent sex differences in prevalence, and natural history (Drevets et al, 2008; Mincic, 2015). Unfortunately, sex differences in these neuroimaging outcomes are understudied. As adolescence and young adulthood are periods of increased presentation of mental health disorders, including those that are female-specific such as premenstrual dysphoric disorder and catemenial epilepsy, it will be imperative to better identify and delineate interactions between adolescent brain maturation, environmental influences, and sex to identify points of vulnerability (Guille et al, 2008; Epperson et al, 2012). To do so, neuroimaging studies must have sufficient sample or effect sizes with respect to male and female participants or outcomes, respectively, to address these critical issues in normal and aberrant neurodevelopment. Similar to rodent studies, human subject investigations of stress effects on neurodevelopment would benefit from greater consideration of the context and timing of environmental perturbations.
Knowledge Gained by Including SABV in Studies of Neurodevelopment and Neuropsychiatric Disorders
Translation of many of these preclinical findings to human health and disease has been hindered for obvious reasons. Although not as mechanistically revealing, the Avon Longitudinal Study of Parents and Children (ALSPAC, n=14 551) initiated in the United Kingdom in 1999 has reported several sex differences with respect to maternal psychosocial distress (anxiety and perceived stress) during pregnancy effects on offspring behavior during infancy and childhood (prepubertal window), and at the age of 18 (Capron et al, 2015). Even when controlling for maternal postpartum affective state and obstetrical factors, maternal anxiety late in gestation was associated most robustly with hyperactivity/inattentiveness in boys and total behavioral/emotional problems in boys and girls assessed at 4 years of age (O'Connor et al, 2003). Later in development, sex differences with respect to maternal antenatal anxiety and cortisol awakening response in a subgroup (n=1000) of 15-year olds from this cohort were less prominent (O'Donnell et al, 2013). Interestingly, maternal, but not paternal, antenatal depression was associated with the increased risk of anxiety disorders at age 18 years among those individuals who remained in the ALSPAC (n=4303), suggesting specific effects of prenatal programming, in addition to environmental and genetic factors, for a neuropsychiatric condition that occurs two to three times more frequently in females than males (Capron et al, 2015).
Smaller studies focusing on brain imaging outcomes reveal that maternal report and neuroendocrine evidence of psychosocial distress during pregnancy is associated with increased right amygdala volume among female, but not male, offspring studied at 7 years of age. In this sample, amygdala volume mediated the relationship between levels of maternal cortisol during pregnancy and affective problems during childhood (Buss et al, 2012). Similarly, intergenerational transmission of parental experience of childhood adversity has been reported for both females and males in rodents and for female parents in humans (Moog et al, 2016). Maternal history of childhood trauma is associated with higher levels of placental corticotropin-releasing factor across pregnancy with a steeper rise in levels in the late second trimester to parturition.
Taken together, clinical and basic science research suggests that fetal exposure to environmental insults can alter the trajectory of brain development. Without consideration of offspring and parental sex, our understanding of the intergenerational transmission of life experiences would be greatly limited. We provide additional specific examples of the importance of considering SABV in our discussion of specific neuropsychiatric disorders below. It should also be considered here that it is also the case that even if studies including both males and females find no sex differences in their outcomes, sex differences can exist at many levels. Certainly, one can get to the same destination via different routes. For instance, in neuropsychiatric diseases such as autism, schizophrenia, or depression, although men and women may be given a similar diagnosis, there exist significant sex differences in overall rates, timing of onset, symptom presentation, and treatment efficacy (Heim and Nemeroff, 1999; Heim and Nemeroff, 2001; Sanchez et al, 2001; Goldstein et al, 2002; Heim et al, 2004; Bale, 2006; Brown and Susser, 2008; Bale, 2009; Brown et al, 2009; Heim et al, 2009; Bale et al, 2010; Heim et al, 2010; Brown, 2012; Davis and Pfaff, 2014; Goldstein et al, 2014). Further, mechanistic animal studies modeling endophenotypes of these disorders have demonstrated robust sex differences in the timing of susceptibility to insults to the developing brain where males appear more vulnerable prenatally and females postnatally (Mueller and Bale, 2006; Mueller and Bale, 2007; Ivy et al, 2008; Kapoor et al, 2008; Mueller and Bale, 2008; Kapoor et al, 2009; Ivy et al, 2010; Hsiao and Patterson, 2012). Therefore, although a male and a female may both be diagnosed with the same disease, for instance autism, the means by which that disease was programmed and presented may be sex-specific.
Male-biased disorders
Recent studies have identified gender-specific patterns and connectivity, suggesting that the brains of boys and girls begin to develop very differently at an early age, where the brains of boys are structured to increase the connectivity between perception and coordinated action, and that of girls to assist in connectivity between analytical and intuitive processing (Satterthwaite et al, 2014). These differences clearly begin during childhood and are further increased by the hormones and maturational processes occurring during adolescence, and as mentioned previously, modified with during periods of dynamic hormonal change such as those occurring during the menstrual cycle, childbearing, and the perimenopause in women.
Certainly, numerous neurodevelopmental disorders exhibit strong sex biases, including autism spectrum disorder with an overall sex ratio of 4 : 1 for boys:girls (as reviewed in Newschaffer et al (2007), Davis and Pfaff (2014), and Gore et al (2014)) as well as attention deficit hyperactivity disorder with a male to female sex ratio of 3.2 : 1 (as reviewed in Erskine et al (2013)). The age of onset of these disorders and their male preponderance, suggests that intra-uterine factors are involved in their pathophysiology. Although the onset of schizophrenia peaks in both males and females after puberty, males are more likely to be affected, to have earlier onset and a more protracted course (Bale and Epperson, 2015). A male, but not female, fetus exposed during the second trimester of gestation to the stress of the 1940 invasion of The Netherlands had increased risk of schizophrenia later in life (van Os and Selten, 1998). This relationship between prenatal exposure to maternal psychosocial stress and risk for schizophrenia in male, but not female, offspring has been replicated in another study, but with first trimester exposure (Khashan et al, 2008). Although there are likely multiple factors contributing to sex differences in disease, sex-specific responses to fetal antecedents occurring during gestational sensitive windows may promote differences in programming trajectories that underlie such disease biases.
Along these lines, functional magnetic resonance imaging studies in men and women diagnosed with schizophrenia confirmed that the expected sex differences in regional volumes were disrupted, including the ratio of orbitofrontal cortex:amygdala, where male schizophrenia patients have a phenotypically more female pattern in these brain regions (Cowell et al, 1996; Goldstein et al, 2002; Gur et al, 2004). Hence, without consideration of outcomes by sex, vital information regarding the origins of neuropsychiatric conditions would be missed. Moreover, identification of those at greatest risk of adverse consequences of maternal psychosocial stress may improve outcomes.
Female-biased disorders
To our knowledge, there are few studies examining the impact of maternal psychosocial stress during discrete gestational windows on risk for affective disorders, which occur more frequently in females. Perhaps, this is due to the challenge of following cohorts from gestation to post-puberty when the sex bias for affective disorders in females is revealed. The ALSPAC study, previously mentioned, did not address potential sex differences regarding gestational exposure to maternal anxiety and depression on risk for affective disorders at age 18 years (Capron et al, 2015), nor did an Australian longitudinal cohort study (n=3099) examine outcomes by sex of the offspring assessed for internalizing and externalizing behaviors at age 21 years (Betts et al, 2015). Given the expense and time associated with prospective cohort studies, we would suggest mining existing databases, which may have sufficient sample sizes to test targeted hypotheses about potential sex or gender differences on risk for affective disorders and other conditions that occur distal to in utero life. Future prospective studies should consider sex and gender in their study design to be compliant with new NIH policies and to reduce missed scientific opportunities.
The Myth of Increased Female Variability
Now that we appreciate the importance and value of including SABV in research studies, questions frequently arise as to how best to design studies that will detect sex differences. We have included several out-takes (Box 1; Figures 1 and 2) to provide an overview of the estrous and menstrual cycles, and how an investigator can focus on or control for particular hormonal and reproductive states in rodents and humans. Our goal is to eradicate the notion and unnecessary roadblock that has hindered many investigators, namely, that females are ‘messy and add variability to results due to their hormonal cycle’. Although there is an entire field devoted to the importance of the female estrous (rodents) or menstrual (primates) cycle on outcomes from dendritic spine dynamics to cognitive processing, most neurobiological measures where an actual sex difference is found are not driven by changes in female cyclicity, the best evidence for which comes from rodent models that we will focus on first.
Yes, estrogen and progesterone significantly change over the estrous and menstrual cycles (Box 1; Figure 1) and across the reproductive life span (Figure 2). And, yes, gonadal hormones can promote significant changes in important neurobiological measures when specifically examined. However, a comprehensive meta-analysis recently completed by Zucker et al examining the variability within sex in 293 publications that included male and female mice showed that, in fact, females were equally or even less variable in all reported molecular, physiological, and behavioral measures examined than were males (Prendergast et al, 2014). This variability was similar between males and females whether animals were single or group housed. This variability comparison has now similarly been completed in rats as well (Becker et al, 2016). In addition, many behavioral studies have similarly reported that when estrous cycle stage was included as a variable, no significant differences in outcome measures were found, including for the Barnes maze, tail suspension test, forced swim test, elevated plus maze, light–dark box, and open-field tests (Mueller and Bale, 2007; Goel and Bale, 2008; Goel and Bale, 2009; Goel and Bale, 2010; Goel et al, 2011). This is not to say that gonadal hormones are not important in behavioral responses, but rather that the variability within females when comparing their outcomes to males does not explain sex differences.
Therefore, although the NIH and other funding agencies in the United States, Canada, and the European Union have now pushed forth the mandate to include SABV in all grant proposal submissions, there remains confusion as to how to best design and interpret results in which males and females are both included. First, as discussed in the Circumspective by McCarthy and Joel in this issue, to include SABV does not suggest that the researchers are asking nor are they powered to ask, if sex differences are present (Joel and McCarthy, 2016). Including both sexes and examining outcomes for potential differences between sexes in the results should provide insight as to whether major differences would be present and if further studies are warranted. The NIH has made it very clear that they are not requiring that everyone study sex differences nor are they in a position to fund the expenses for doubling of experimental numbers. But including female comparisons in what has been for most fields largely male-centric can only be seen as a benefit, as we consider additional modes and mechanisms in disease risk and resilience across the life span.
So, how then does an experimenter design their studies so as to be inclusive of SABV without doubling their experimental numbers? To start, knowing the literature as to reported sex differences can be very helpful in how to best go about including both sexes in your study or the appropriate justification for focusing on one sex only. Similarly, if you are expecting sex differences, knowing what type of sex difference can make a big difference in your experimental numbers and planned comparisons. For instance, if you are running a Barnes maze behavioral test and knowing that males and females use different strategies to locate the hidden escape box, then you know that the latency for both groups may be different, but the interpretation of the difference is not that females have decreased spatial ability, but rather that their less risk-aversive serial search strategy requires additional travel time (Mueller and Bale, 2007). This is an example of a sexually dimorphic outcome where the measure exists in two forms, one more prevalent in one sex vs the other (ie, females using a serial search strategy, males using a spatial navigation strategy in this test; Joel and McCarthy, 2016). Knowing this, you might design your study to ask about differences within sex for a given manipulation rather than between sexes. As another example, in post-puberty rodents, the HPA stress axis has a significant sex difference in the amount of ACTH and corticosterone produced in response to a given acute stressor (Handa et al, 1994; Handa et al, 1994; Romeo et al, 2004; Romeo and McEwen, 2006; Goel and Bale, 2007; Goel and Bale, 2008; Goel and Bale, 2009; Handa et al, 2009; Weiser and Handa, 2009). This would be an example of a sex difference that is along a continuum, with females producing the same hormones and in the same direction as males (increased following stress), but just at higher levels (Joel and McCarthy, 2016). In this example, one should be aware that when designing studies comparing sexes, most biological responses have floor and ceiling effects. So, although one sex can increase (males) or decrease (females) their stress response more than the other following a given manipulation, this may not constitute an actual sex difference due to the limitations of different starting points for each sex. Last, if you detect high variability specifically in your female groups and want to determine the potential impact of cycle stage, we have included general information for a ‘how to’ in Box 1. Most rodents will move through four stages of the estrous cycle as follows: metestrus, diestrus, proestrus, and estrus. Rats are more predictable in this 4-day cycle than mice tend to be, although this can be strain-, age-, and environment-specific (Caligioni, 2009). Females co-housed together do not necessarily cycle together, but in mice, this group housing can induce a ‘persistent estrus’ state. Estradiol and progesterone levels are highest leading up to proestrus, which promotes reproductive behaviors and ovulation, and then remain relatively low across the remainder of the estrous cycle.
Similarly in humans, consideration of the menstrual cycle (Figure 1) and reproductive status (Figure 2) of the individual may reduce overall noise in the data and enhance the capacity to detect the outcomes between groups. As an example, pre-pulse inhibition (PPI) of the acoustic startle response, a measure of sensorimotor gating, is diminished among individuals with schizophrenia as well as in healthy women during late pregnancy and the luteal phase of the menstrual cycle (Braff et al, 2001). PPI response has historically been considered a potential endophenotype for schizophrenia, and a number of drug development studies have focused on the capacity of a given drug to modulate the PPI as a model for potential efficacy in the treatment of schizophrenia (Braff and Light, 2005; Javitt et al, 2008). Hence, investigations of PPI in the pathophysiology and treatment of schizophrenia should take into consideration the reproductive status of the individual as gonadal steroids can modify PPI in both men and women. This is but one example of an area of neuropsychiatric research for which an investigator should consider SABV or they risk obtaining a finding that is specific to reproductive aged males only (before the age-related decline in androgens; Figure 2).
How then do clinical and translational investigators know when and how to consider SABV and design their investigation in a manner to directly test for sex differences? We would argue that all research focusing on normal physiology and disease states or conditions which occur in both sexes should be powered to detect a potential sex difference in outcomes of interest or at the very least sex/gender should be included as a covariate. If both sexes will not be included in the investigation in question, the onus is upon the investigator to justify the exclusion of one sex or the other. This will be relatively simple when studying conditions such as breast cancer, which occur in both sexes, but 99% of cases are women, or pregnancy states for obvious reasons. In contrast, coronary heart disease (CHD) is roughly equal between men and women between the ages of 40 and 59 years (Mozaffarian et al, 2015). Therefore, it may be difficult to justify a male only study of CHD among younger adults. Further, estradiol has the protective effects against CHD among healthy young female adults, suggesting that reproductive status, as well as age, is crucial to consider when investigating CHD.
Figure 1 illustrates a typical menstrual cycle with respect to length and reproductive hormone levels among premenopausal women. If there is a reason to consider the potential effects of gonadal hormones on an outcome of interest such as PPI, it is most straightforward to study all female participants in the early to mid-follicular phase when the vast majority of women will have relatively low levels of estradiol and progesterone as well as the progesterone neurosteroid metabolite, allopregnanolone (ALLO). By day 8 of the menstrual cycle (with day 1 anchored to the first day of menstruation), estradiol begins to rise but does not peak until ovulation. Finally, the luteal phase of the menstrual cycle is characterized by a more complex hormonal milieu that is less predictable between cycles and between women. Young adolescent girls and women with disorders such as polycystic ovarian syndrome frequently have anovulatory cycles, characterized by low progesterone levels. Such cycles disrupt the normal hormonal milieu of the luteal phase as well as the length of the cycle, making timing of an investigation or procedure with respect to the desired phase more challenging.
For investigators who wish to isolate the impact of estradiol on outcomes of interest in naturally cycling women, test days should occur during the first week of the onset of menstruation and between days 12 and 15 of an idealized 28-day cycle. In this case, a within subject design is ideal. However, some investigators such as Mohammed Milad and his laboratory have been successful in examining sex, reproductive hormones, and oral contraceptive pill (OCP) effects on their outcomes of interest (primarily fear conditioning and extinction) by studying men and women without regard for the hormonal status of the female on a given test day (Hwang et al, 2015). They parse the women into groups based upon blood hormone levels or self-report of timing of last menstrual period and report of OCP use. This procedure is most effective when there are few constraints on access to study equipment or facilities, but may be less effective in costly neuroimaging studies if a specific hormonal milieu is the goal. The gold standard for defining menstrual cycle phase or effects of specific levels of hormones on outcomes is to obtain blood samples for hormonal staging on each test day.
For those who are interested in capturing the luteal phase of the cycle, it is best to require participants to track their menstrual pattern for at least one cycle and to determine the timing of ovulation using urine luteinizing hormone (LH) kits. These kits can be somewhat difficult to interpret, and women should follow the instructions for a specific kit closely. In our experience, women frequently question whether a LH detection line is dark enough to be positive and we now ask all women to take a cell phone picture of their results to forward to our investigators for confirmation.
CONCLUSIONS
In summary, the NIH policy to consider SABV is a mandate that impacts every investigator who plans to seek federal funding for their research. However, we contend that the most important reason to consider sex and gender in biomedical research is that it improves the quality of the science, and the safety and efficacy of treatments for human disorders. In addition, there is great potential to gain mechanistic insight from studies where sex differences are identified. The antiquated myth that females are ‘messy’ and make research more difficult is not supported by the evidence, and articles such as this one, and those from other investigators who have been considering sex and gender in their research for decades, will help promote the inclusion and importance of SABV in biomedical research (Bale and Epperson, 2015; Miller et al, 2015; Becker and Koob, 2016; Joel and McCarthy, 2016).
FUNDING AND DISCLOSURE
The work discussed in this review was funded in part by grants from the NIH MH073030 (Bale), MH091258 (Bale), MH087597 (Bale), MH104184 (Bale), MH108286 (Bale), MH099910 (Epperson and Bale), AG048839 (Epperson), and DA030301 (Epperson). Dr Epperson acknowledges the receipt of research grant support from Shire and Sage Therapeutics, stock investments in Eli Lilly, Pfizer, Abbott, Abbvie, Merck, and Johnson and 20 Johnson, as well as consulting to Sage Therapeutics, Forest Laboratories, and Asarina Pharmaceuticals. The authors declare no conflict of interest.
References
Final report on the aspirin component of the ongoing Physicians' Health Study (1989). Steering Committee of the Physicians' Health Study Research Group. N Engl J Med 321: 129–135.
Albert K, Pruessner J, Newhouse P (2015). Estradiol levels modulate brain activity and negative responses to psychosocial stress across the menstrual cycle. Psychoneuroendocrinology 59: 14–24.
Arnold AP (2009). The organizational-activational hypothesis as the foundation for a unified theory of sexual differentiation of all mammalian tissues. Horm Behav 55: 570–578.
Azak S (2012). Maternal depression and sex differences shape the infants' trajectories of cognitive development. Infant Behav Dev 35: 803–814.
Bachmann GA, Mussman B (2015). The aging population: imperative to uncouple sex and gender to establish gender equal health care. Maturitas 80: 421–425.
Bale TL (2006). Stress sensitivity and the development of affective disorders. Horm Behav 50: 529–533.
Bale TL (2009). Neuroendocrine and immune influences on the CNS: it's a matter of sex. Neuron 64: 13–16.
Bale TL, Baram TZ, Brown AS, Goldstein JM, Insel TR, McCarthy MM et al (2010). Early life programming and neurodevelopmental disorders. Biol Psychiatry 68: 314–319.
Bale TL, Epperson CN (2015). Sex differences and stress across the lifespan. Nat Neurosci 18: 1413–1420.
Barker JM, Torregrossa MM, Arnold AP, Taylor JR (2010). Dissociation of genetic and hormonal influences on sex differences in alcoholism-related behaviors. J Neurosci 30: 9140–9144.
Baron-Cohen S, Auyeung B, Norgaard-Pedersen B, Hougaard DM, Abdallah MW, Melgaard L et al (2015). Elevated fetal steroidogenic activity in autism. Mol Psychiatry 20: 369–376.
Becker JB, Arnold AP, Berkley KJ, Blaustein JD, Eckel LA, Hampson E et al (2005). Strategies and methods for research on sex differences in brain and behavior. Endocrinology 146: 1650–1673.
Becker JB, Koob GF (2016). Sex differences in animal models: focus on addiction. Pharmacol Rev 68: 242–263.
Becker JB, Prendergast BJ, Liang JW (2016). Female rats are not more variable than male rats: a meta-analysis of neuroscience studies. Biol Sex Differ 7: 34.
Betts KS, Williams GM, Najman JM, Alati R (2015). The relationship between maternal depressive, anxious, and stress symptoms during pregnancy and adult offspring behavioral and emotional problems. Depress Anxiety 32: 82–90.
Bingham B, Viau V (2008). Neonatal gonadectomy and adult testosterone replacement suggest an involvement of limbic arginine vasopressin and androgen receptors in the organization of the hypothalamic-pituitary-adrenal axis. Endocrinology 149: 3581–3591.
Borchers AT, Gershwin ME (2012). Sociological differences between women and men: implications for autoimmunity. Autoimmun Rev 11: A413–A421.
Braff DL, Geyer MA, Swerdlow NR (2001). Human studies of prepulse inhibition of startle: normal subjects, patient groups, and pharmacological studies. Psychopharmacology 156: 234–258.
Braff DL, Light GA (2005). The use of neurophysiological endophenotypes to understand the genetic basis of schizophrenia. Dialogues Clin Neurosci 7: 125–135.
Brown AS (2012). Epidemiologic studies of exposure to prenatal infection and risk of schizophrenia and autism. Dev Neurobiol 27: 1272–1276.
Brown AS, Susser ES (2008). Prenatal nutritional deficiency and risk of adult schizophrenia. Schizophr Bull 34: 1054–1063.
Brown AS, Vinogradov S, Kremen WS, Poole JH, Deicken RF, Penner JD et al (2009). Prenatal exposure to maternal infection and executive dysfunction in adult schizophrenia. Am J Psychiatry 166: 683–690.
Buss C, Davis EP, Shahbaba B, Pruessner JC, Head K, Sandman CA (2012). Maternal cortisol over the course of pregnancy and subsequent child amygdala and hippocampus volumes and affective problems. Proc Natl Acad Sci USA 109: E1312–E1319.
Cahill L (2014). Equal not equal the same: sex differences in the human brain. Cerebrum 2014: 5.
Caligioni CS (2009). Assessing reproductive status/stages in mice. Curr Protoc Neurosci 48: 4I:A.4I.1–A.4I.8.
Capel B (1998). Sex in the 90s: SRY and the switch to the male pathway. Annu Rev Physiol 60: 497–523.
Capron LE, Glover V, Pearson RM, Evans J, O'Connor TG, Stein A et al (2015). Associations of maternal and paternal antenatal mood with offspring anxiety disorder at age 18 years. J Affect Disord 187: 20–26.
Chura LR, Lombardo MV, Ashwin E, Auyeung B, Chakrabarti B, Bullmore ET et al (2010). Organizational effects of fetal testosterone on human corpus callosum size and asymmetry. Psychoneuroendocrinology 35: 122–132.
Comasco E, Hahn A, Ganger S, Gingnell M, Bannbers E, Oreland L et al (2014). Emotional fronto-cingulate cortex activation and brain derived neurotrophic factor polymorphism in premenstrual dysphoric disorder. Hum Brain Mapp 35: 4450–4458.
Cowell PE, Kostianovsky DJ, Gur RC, Turetsky BI, Gur RE (1996). Sex differences in neuroanatomical and clinical correlations in schizophrenia. Am J Psychiatry 153: 799–805.
Davis EP, Pfaff D (2014). Sexually dimorphic responses to early adversity: implications for affective problems and autism spectrum disorder. Psychoneuroendocrinology 49: 11–25.
Drevets WC, Price JL, Furey ML (2008). Brain structural and functional abnormalities in mood disorders: implications for neurocircuitry models of depression. Brain Struct Funct 213: 93–118.
Dumas JA, Albert KM, Naylor MR, Sites CK, Benkelfat C, Newhouse PA (2012). The effects of age and estrogen on stress responsivity in older women. Am J Geriatr Psychiatry 20: 734–743.
Epperson CN, Pittman B, Czarkowski KA, Stiklus S, Krystal JH, Grillon C (2007). Luteal-phase accentuation of acoustic startle response in women with premenstrual dysphoric disorder. Neuropsychopharmacology 32: 2190–2198.
Epperson CN, Steiner M, Hartlage SA, Eriksson E, Schmidt PJ, Jones I et al (2012). Premenstrual dysphoric disorder: evidence for a new category for DSM-5. Am J Psychiatry 169: 465–475.
Erskine HE, Ferrari AJ, Nelson P, Polanczyk GV, Flaxman AD, Vos T et al (2013). Epidemiological modelling of attention-deficit/hyperactivity disorder and conduct disorder for the Global Burden of Disease Study 2010. J Child Psychol Psychiatry 54: 1263–1274.
Felitti VJ, Anda RF, Nordenberg D, Williamson DF, Spitz AM, Edwards V et al (1998). Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults. The Adverse Childhood Experiences (ACE) Study. Am J Prev Med 14: 245–258.
Franconi F, Campesi I, Occhioni S, Antonini P, Murphy MF (2012). Sex and gender in adverse drug events, addiction, and placebo. Handb Exp Pharmacol 214: 107–126.
Goel N, Bale TL (2007). Identifying early behavioral and molecular markers of future stress sensitivity. Endocrinology 148: 4585–4591.
Goel N, Bale TL (2008). Organizational and activational effects of testosterone on masculinization of female physiological and behavioral stress responses. Endocrinology 149: 6399–6405.
Goel N, Bale TL (2009). Examining the intersection of sex and stress in modelling neuropsychiatric disorders. J Neuroendocrinol 21: 415–420.
Goel N, Bale TL (2010). Sex differences in the serotonergic influence on the hypothalamic-pituitary-adrenal stress axis. Endocrinology 151: 1784–1794.
Goel N, Plyler KS, Daniels D, Bale TL (2011). Androgenic influence on serotonergic activation of the HPA stress axis. Endocrinology 152: 2001–2010.
Goldstein JM, Handa RJ, Tobet SA (2014). Disruption of fetal hormonal programming (prenatal stress) implicates shared risk for sex differences in depression and cardiovascular disease. Front Neuroendocrinol 35: 140–158.
Goldstein JM, Seidman LJ, O'Brien LM, Horton NJ, Kennedy DN, Makris N et al (2002). Impact of normal sexual dimorphisms on sex differences in structural brain abnormalities in schizophrenia assessed by magnetic resonance imaging. Arch Gen Psychiatry 59: 154–164.
Gore AC, Martien KM, Gagnidze K, Pfaff D (2014). Implications of prenatal steroid perturbations for neurodevelopment, behavior, and autism. Endocr Rev 35: 961–991.
Gregg C, Zhang J, Weissbourd B, Luo S, Schroth GP, Haig D et al (2010). High-resolution analysis of parent-of-origin allelic expression in the mouse brain. Science 329: 643–648.
Grumbach MM, Auchus RJ (1999). Estrogen: consequences and implications of human mutations in synthesis and action. J Clin Endocrinol Metab 84: 4677–4694.
Guille C, Spencer S, Cavus I, Epperson CN (2008). The role of sex steroids in catamenial epilepsy and premenstrual dysphoric disorder: implications for diagnosis and treatment. Epilepsy Behav 13: 12–24.
Gur RE, Kohler C, Turetsky BI, Siegel SJ, Kanes SJ, Bilker WB et al (2004). A sexually dimorphic ratio of orbitofrontal to amygdala volume is altered in schizophrenia. Biol Psychiatry 55: 512–517.
Handa RJ, Burgess LH, Kerr JE, O'Keefe JA (1994). Gonadal steroid hormone receptors and sex differences in the hypothalamo-pituitary-adrenal axis. Horm Behav 28: 464–476.
Handa RJ, Nunley KM, Lorens SA, Louie JP, McGivern RF, Bollnow MR (1994). Androgen regulation of adrenocorticotropin and corticosterone secretion in the male rat following novelty and foot shock stressors. Physiol Behav 55: 117–124.
Handa RJ, Weiser MJ, Zuloaga DG (2009). A role for the androgen metabolite, 5alpha-androstane-3beta,17beta-diol, in modulating oestrogen receptor beta-mediated regulation of hormonal stress reactivity. J Neuroendocrinol 21: 351–358.
Hantsoo L, Epperson CN (2015). Premenstrual dysphoric disorder: epidemiology and treatment. Curr Psychiatry Rep 17: 87.
Heim C, Bradley B, Mletzko TC, Deveau TC, Musselman DL, Nemeroff CB et al (2009). Effect of childhood trauma on adult depression and neuroendocrine function: sex-specific moderation by CRH receptor 1 gene. Front Behav Neurosci 3: 41.
Heim C, Nemeroff CB (1999). The impact of early adverse experiences on brain systems involved in the pathophysiology of anxiety and affective disorders. Biol Psychiatry 46: 1509–1522.
Heim C, Nemeroff CB (2001). The role of childhood trauma in the neurobiology of mood and anxiety disorders: preclinical and clinical studies. Biol Psychiatry 49: 1023–1039.
Heim C, Plotsky PM, Nemeroff CB (2004). Importance of studying the contributions of early adverse experience to neurobiological findings in depression. Neuropsychopharmacology 29: 641–648.
Heim C, Shugart M, Craighead WE, Nemeroff CB (2010). Neurobiological and psychiatric consequences of child abuse and neglect. Dev Psychobiol 52: 671–690.
Hendi AS (2015). Trends in U.S. life expectancy gradients: the role of changing educational composition. Int J Epidemiol 44: 946–955.
Hines M Brain Gender. Oxford University Press: Oxford; (2005).
Hong DS, Hoeft F, Marzelli MJ, Lepage JF, Roeltgen D, Ross J et al (2014). Influence of the X-chromosome on neuroanatomy: evidence from Turner and Klinefelter syndromes. J Neurosci 34: 3509–3516.
Hong DS, Reiss AL (2014). Cognitive and neurological aspects of sex chromosome aneuploidies. Lancet Neurol 13: 306–318.
Hsiao EY, Patterson PH (2012). Placental regulation of maternal-fetal interactions and brain development. Dev Neurobiol 72: 1317–1326.
Hwang MJ, Zsido RG, Song H, Pace-Schott EF, Miller KK, Lebron-Milad K et al (2015). Contribution of estradiol levels and hormonal contraceptives to sex differences within the fear network during fear conditioning and extinction. BMC Psychiatry 15: 295.
Imperato-McGinley J, Peterson RE, Gautier T, Cooper G, Danner R, Arthur A et al (1982). Hormonal evaluation of a large kindred with complete androgen insensitivity: evidence for secondary 5 alpha-reductase deficiency. J Clin Endocrinol Metab 54: 931–941.
Ivy AS, Brunson KL, Sandman C, Baram TZ (2008). Dysfunctional nurturing behavior in rat dams with limited access to nesting material: a clinically relevant model for early-life stress. Neuroscience 154: 1132–1142.
Ivy AS, Rex CS, Chen Y, Dube C, Maras PM, Grigoriadis DE et al (2010). Hippocampal dysfunction and cognitive impairments provoked by chronic early-life stress involve excessive activation of CRH receptors. J Neurosci 30: 13005–13015.
Javitt DC, Spencer KM, Thaker GK, Winterer G, Hajos M (2008). Neurophysiological biomarkers for drug development in schizophrenia. Nat Rev Drug Discov 7: 68–83.
Joel D, McCarthy MM (2016). Incorporating sex as a biological variable in neuropsychiatric research: where are we now and where should we be? Neuropsychopharmacology (e-pub ahead of print; doi:10.1038/npp.2016.79).
Kapoor A, Kostaki A, Janus C, Matthews SG (2009). The effects of prenatal stress on learning in adult offspring is dependent on the timing of the stressor. Behav Brain Res 197: 144–149.
Kapoor A, Leen J, Matthews SG (2008). Molecular regulation of the hypothalamic-pituitary-adrenal axis in adult male guinea pigs after prenatal stress at different stages of gestation. J Physiol 586 (Pt 17): 4317–4326.
Karatsoreos IN, McEwen BS (2013). Annual research review: the neurobiology and physiology of resilience and adaptation across the life course. J Child Psychol Psychiatry 54: 337–347.
Karatsoreos IN, McEwen BS (2013). Resilience and vulnerability: a neurobiological perspective. F1000Prime Rep 5: 13.
Khashan AS, Abel KM, McNamee R, Pedersen MG, Webb RT, Baker PN et al (2008). Higher risk of offspring schizophrenia following antenatal maternal exposure to severe adverse life events. Arch Gen Psychiatry 65: 146–152.
King N (2014). Permanent post concussion symptoms after mild head injury: a systematic review of age and gender factors. NeuroRehabilitation 34: 741–748.
Kingston D, Tough S, Whitfield H (2012). Prenatal and postpartum maternal psychological distress and infant development: a systematic review. Child Psychiatry Hum Dev 43: 683–714.
Liu Z, Liu J, Shi X, Wang L, Yang Y, Tao M (2015). Dynamic alteration of serum testosterone with aging: a cross-sectional study from Shanghai, China. Reprod Biol Endocrinol 13: 111.
Lombardo MV, Ashwin E, Auyeung B, Chakrabarti B, Lai MC, Taylor K et al (2012). Fetal programming effects of testosterone on the reward system and behavioral approach tendencies in humans. Biol Psychiatry 72: 839–847.
Lombardo MV, Ashwin E, Auyeung B, Chakrabarti B, Taylor K, Hackett G et al (2012). Fetal testosterone influences sexually dimorphic gray matter in the human brain. J Neurosci 32: 674–680.
Manwani B, Bentivegna K, Benashski SE, Venna VR, Xu Y, Arnold AP et al (2015). Sex differences in ischemic stroke sensitivity are influenced by gonadal hormones, not by sex chromosome complement. J Cereb Blood Flow Metab 35: 221–229.
Marar M, McIlvain NM, Fields SK, Comstock RD (2012). Epidemiology of concussions among United States high school athletes in 20 sports. Am J Sports Med 40: 747–755.
Mazure CM, Jones DP (2015). Twenty years and still counting: including women as participants and studying sex and gender in biomedical research. BMC Womens Health 15: 94.
McCarthy MM (1994). Molecular aspects of sexual differentiation of the rodent brain. Psychoneuroendocrinology 19: 415–427.
McCarthy MM (2016). Multifaceted origins of sex differences in the brain. Philos Trans R Soc Lond B Biol Sci 371: 20150106.
McCarthy MM, Auger AP, Bale TL, De Vries GJ, Dunn GA, Forger NG et al (2009). The epigenetics of sex differences in the brain. J Neurosci 29: 12815–12823.
McEwen BS, Morrison JH (2013). The brain on stress: vulnerability and plasticity of the prefrontal cortex over the life course. Neuron 79: 16–29.
Miller VM, Rocca WA, Faubion SS (2015). Sex differences research, precision medicine, and the Future of Women's Health. J Womens Health (Larchmt) 24: 969–971.
Mincic AM (2015). Neuroanatomical correlates of negative emotionality-related traits: a systematic review and meta-analysis. Neuropsychologia 77: 97–118.
Moog NK, Buss C, Entringer S, Shahbaba B, Gillen DL, Hobel CJ et al (2016). Maternal exposure to childhood trauma is associated during pregnancy with placental-fetal stress physiology. Biol Psychiatry 79: 831–839.
Moroz EV, Verkhratsky NS (1985). Hypophyseal-gonadal system during male aging. Arch Gerontol Geriatr 4: 13–19.
Mozaffarian D, Benjamin EJ, Go AS, Arnett DK, Blaha MJ, Cushman M et al (2015). Heart disease and stroke statistics–-2015 update: a report from the American Heart Association. Circulation 131: e29–322.
Mueller BR, Bale TL (2006). Impact of prenatal stress on long term body weight is dependent on timing and maternal sensitivity. Physiol Behav 88: 605–614.
Mueller BR, Bale TL (2007). Early prenatal stress impact on coping strategies and learning performance is sex dependent. Physiol Behav 91: 55–65.
Mueller BR, Bale TL (2008). Sex-specific programming of offspring emotionality after stress early in pregnancy. J Neurosci 28: 9055–9065.
Nelson JF, Felicio LS, Randall PK, Sims C, Finch CE (1982). A longitudinal study of estrous cyclicity in aging C57BL/6J mice: I. Cycle frequency, length and vaginal cytology. Biol Reprod 27: 327–339.
Newschaffer CJ, Croen LA, Daniels J, Giarelli E, Grether JK, Levy SE et al (2007). The epidemiology of autism spectrum disorders. Annu Rev Public Health 28: 235–258.
Nugent BM, Wright CL, Shetty AC, Hodes GE, Lenz KM, Mahurkar A et al (2015). Brain feminization requires active repression of masculinization via DNA methylation. Nat Neurosci 18: 690–697.
O'Connor TG, Heron J, Golding J, Glover V, Team AS (2003). Maternal antenatal anxiety and behavioural/emotional problems in children: a test of a programming hypothesis. J Child Psychol Psychiatry 44: 1025–1036.
O'Donnell KJ, Glover V, Jenkins J, Browne D, Ben-Shlomo Y, Golding J et al (2013). Prenatal maternal mood is associated with altered diurnal cortisol in adolescence. Psychoneuroendocrinology 38: 1630–1638.
Parekh A, Fadiran EO, Uhl K, Throckmorton DC (2011). Adverse effects in women: implications for drug development and regulatory policies. Expert Rev Clin Pharmacol 4: 453–466.
Pechtel P, Lyons-Ruth K, Anderson CM, Teicher MH (2014). Sensitive periods of amygdala development: the role of maltreatment in preadolescence. Neuroimage 97: 236–244.
Pembrey M, Saffery R, Bygren LO., Network in Epigenetic Epidemiology (2014). Human transgenerational responses to early-life experience: potential impact on development, health and biomedical research. J Med Genet 51: 563–572.
Prendergast BJ, Onishi KG, Zucker I (2014). Female mice liberated for inclusion in neuroscience and biomedical research. Neurosci Biobehav Rev 40: 1–5.
Quinn JJ, Hitchcott PK, Umeda EA, Arnold AP, Taylor JR (2007). Sex chromosome complement regulates habit formation. Nat Neurosci 10: 1398–1400.
Ridker PM, Cook NR, Lee IM, Gordon D, Gaziano JM, Manson JE et al (2005). A randomized trial of low-dose aspirin in the primary prevention of cardiovascular disease in women. N Engl J Med 352: 1293–1304.
Rodgers AB, Bale TL (2015). Germ cell origins of posttraumatic stress disorder risk: the transgenerational impact of parental stress experience. Biol Psychiatry 78: 307–314.
Romeo RD, Lee SJ, Chhua N, McPherson CR, McEwen BS (2004). Testosterone cannot activate an adult-like stress response in prepubertal male rats. Neuroendocrinology 79: 125–132.
Romeo RD, McEwen BS (2006). Stress and the adolescent brain. Ann NY Acad Sci 1094: 202–214.
Rose AB, Merke DP, Clasen LS, Rosenthal MA, Wallace GL, Vaituzis AC et al (2004). Effects of hormones and sex chromosomes on stress-influenced regions of the developing pediatric brain. Ann NY Acad Sci 1032: 231–233.
Sanchez MM, Ladd CO, Plotsky PM (2001). Early adverse experience as a developmental risk factor for later psychopathology: evidence from rodent and primate models. Dev Psychopathol 13: 419–449.
Satterthwaite TD, Shinohara RT, Wolf DH, Hopson RD, Elliott MA, Vandekar SN et al (2014). Impact of puberty on the evolution of cerebral perfusion during adolescence. Proc Natl Acad Sci USA 111: 8643–8648.
Satterthwaite TD, Vandekar S, Wolf DH, Ruparel K, Roalf DR, Jackson C et al (2014). Sex differences in the effect of puberty on hippocampal morphology. J Am Acad Child Adolesc Psychiatry 53: 341–350 e341.
Shanmugan S, Epperson CN (2014). Estrogen and the prefrontal cortex: towards a new understanding of estrogen's effects on executive functions in the menopause transition. Hum Brain Mapp 35: 847–865.
Sorensen MB, Fritz-Hansen T, Jensen HH, Pedersen AT, Hojgaard L, Ottesen B (2001). Temporal changes in cardiac function and cerebral blood flow during sequential postmenopausal hormone replacement. Am J Obstet Gynecol 184: 41–47.
Spoletini I, Vitale C, Malorni W, Rosano GM (2012). Sex differences in drug effects: interaction with sex hormones in adult life. Handb Exp Pharmacol 214: 91–105.
Springer KW, Mager Stellman J, Jordan-Young RM (2012). Beyond a catalogue of differences: a theoretical frame and good practice guidelines for researching sex/gender in human health. Soc Sci Med 74: 1817–1824.
Timby E, Backstrom T, Nyberg S, Stenlund H, Wihlback AC, Bixo M (2016). Women with premenstrual dysphoric disorder have altered sensitivity to allopregnanolone over the menstrual cycle compared to controls-a pilot study. Psychopharmacology 233: 2109–2117.
van Os J, Selten JP (1998). Prenatal exposure to maternal stress and subsequent schizophrenia. The May 1940 invasion of The Netherlands. Br J Psychiatry 172: 324–326.
Weiser MJ, Handa RJ (2009). Estrogen impairs glucocorticoid dependent negative feedback on the hypothalamic-pituitary-adrenal axis via estrogen receptor alpha within the hypothalamus. Neuroscience 159: 883–895.
Whitley H, Lindsey W (2009). Sex-based differences in drug activity. Am Fam Physician 80: 1254–1258.
Zahn-Waxler C, Shirtcliff EA, Marceau K (2008). Disorders of childhood and adolescence: gender and psychopathology. Annu Rev Clin Psychol 4: 275–303.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Bale, T., Epperson, C. Sex as a Biological Variable: Who, What, When, Why, and How. Neuropsychopharmacol 42, 386–396 (2017). https://doi.org/10.1038/npp.2016.215
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/npp.2016.215
This article is cited by
-
A longitudinal cohort study on the use of health and care services by older adults living at home with/without dementia before and during the COVID-19 pandemic: the HUNT study
BMC Health Services Research (2024)
-
Sex differences in DNA methylation across gestation: a large scale, cross-cohort, multi-tissue analysis
Cellular and Molecular Life Sciences (2024)
-
Sex differences in distribution and identity of aromatase gene expressing cells in the young adult rat brain
Biology of Sex Differences (2023)
-
Structured tracking of alcohol reinforcement (STAR) for basic and translational alcohol research
Molecular Psychiatry (2023)
-
Early life stress in male mice blunts responsiveness in a translationally-relevant reward task
Neuropsychopharmacology (2023)