Abstract
Mitochondria are involved in the development of organ failure in critical care diseases. However, the mechanisms underlying mitochondrial dysfunction are not clear yet. Inducible hemoxygenase (HO-1), a member of the heat shock protein family, is upregulated in critical care diseases and considered to confer cytoprotection against oxidative stress. However, one of the products of HO-1 is Fe2+ which multiplies the damaging potential of reactive oxygen species catalyzing Fenton reaction. The aim of this study was to clarify the relevance of free iron metabolism to the oxidative damage of the liver in endotoxic shock and its impact on mitochondrial function. Endotoxic shock in rats was induced by injection of lipopolysaccharide (LPS) at a dose of 8 mg/kg (i.v.). We observed that the pro-inflammatory cytokine TNF-α and the liver necrosis marker aspartate aminotransferase were increased in blood, confirming inflammatory response to LPS and damage to liver tissue, respectively. The levels of free iron in the liver were significantly increased at 4 and 8 h after onset of endotoxic shock, which did not coincide with the decrease of transferrin iron levels in the blood, but rather with expression of the inducible form of heme oxygenase (HO-1). The proteins important for sequestering free iron (ferritin) and the export of iron out of the cells (ferroportin) were downregulated facilitating the accumulation of free iron in cells. The temporarily increased concentration of free iron in the liver correlated with the temporary impairment of both mitochondrial function and tissue ATP levels. Addition of exogenous iron ions to mitochondria isolated from control animals resulted in an impairment of mitochondrial respiration similar to that observed in endotoxic shock in vivo. Our data suggest that free iron released by HO-1 causes mitochondrial dysfunction in pathological situations accompanied by endotoxic shock.
Similar content being viewed by others
Introduction
Sepsis is the leading cause of death in adult intensive care units.1 The reason for death in sepsis is multiple organ failure (MOF). The mechanisms causing MOF are not yet clear. However, oxidative stress and mitochondrial dysfunction appear to be the most common candidates. Among articles considering oxidative stress as a mechanism leading to organ dysfunction, there are a number of authors reporting beneficial effects of iron chelators.2, 3, 4, 5, 6 On the other hand, it is a known fact that iron levels in the blood are decreased under inflammatory conditions.7, 8 This evidence suggests underlying changes of iron metabolism and especially of free iron, which is particularly potent in inducing oxidative stress.
Iron in low-molecular-weight forms may play a catalytic role in the initiation of free radical reactions.9, 10 The resulting oxyradicals have the potential to damage cellular lipids, nucleic acids, proteins, and carbohydrates; the consequence is wide-ranging impairment in cellular function and integrity.11 One of the targets of iron-mediated oxidative stress is mitochondria.12 In sepsis, the level of circulating iron in the plasma is decreased due to retention of iron within the cells. This phenomenon is considered to be a defense reaction depriving bacteria of iron.13
Though mitochondrial function during sepsis and endotoxic shock has been studied extensively, results are contradictory. Mitochondrial function during septic/endotoxic shock depends on: (i) the source of mitochondria, (ii) the experimental induction of septic/endotoxic shock, and (iii) the phase of illness. Mitochondria obtained from different organs show different susceptibility to septic/endotoxic shock (reviewed by Taylor and Piantadosi14). In acute bacteremia induced by E. coli, for example, mitochondria isolated from kidney before death have normal state 3 respiration, whereas mitochondria from brain have significantly reduced state 3 activity.14 Septic/endotoxic shock induced intraperitoneally/subcutaneously either has no effect on mitochondrial function or increases state 3 respiration, consequently improving respiratory control values.15, 16, 17, 18 In contrast, intravenous injection/infusion of endotoxin mostly affects mitochondrial function by decreasing state 3 respiration and ATP synthesis at least in the late phase of endotoxic shock.19, 20, 21, 22 However, intravenous infusion of E. coli has been shown both to improve and to decrease respiration in state 3.23 Another important observation was that mitochondrial respiration often increases in the early phase of acute critical illness, including septic/endotoxic shock, but consistently falls during the late phase of illness.19, 24, 25 Thus it appears to be important to follow the time course of mitochondrial function under septic conditions, but this was not yet been systematically studied.
The aim of this study was to clarify the contribution of free iron metabolism to liver damage and mitochondrial dysfunction in rats subjected to endotoxic shock at different time points after onset of shock.
MATERIALS AND METHODS
Endotoxic Shock
Rats were injected with lipopolysaccharide (LPS) at a dose of 8 mg/kg (i.v.). Adult male Sprague–Dawley rats weighing 280±21 g (Animal Research Laboratories, Himberg, Austria) were divided into two groups: a control group receiving saline i.v. and a group receiving 8 mg lipopolysaccharide/kg i.v. (LPS; E. coli 026:B6, Difco, Detroit, MI, USA). This dosage of LPS was used in our previous studies26 and by others.27, 28 At different time points (0, 2, 4, 8, and 12 h (n=7)), the animals were killed; blood and liver tissue were taken for analytical examination. All animals received humane care according to the criteria outlined in the ‘Guide for the Care and Use of Laboratory Animals’ prepared by the National Academy of Sciences and published by the National Institutes of Health (NIH publication 86-23 revised 1985).
Preparation of Mitochondria
Rat liver mitochondria (RLM) were prepared as described previously29 and stored at 0°C for 4–5 h in a buffer containing 0.25 M sucrose, 10 mM TRIS-HCl, 0.5 mM EDTA (pH 7.2), and 0.5 g/l essentially fatty-acid-free bovine serum albumin.
Mitochondrial Function and ROS Generation
Respiratory parameters of mitochondria isolated from control and LPS-treated rats were determined with a Clark-type oxygen electrode (OROBOROS Ltd, Innsbruck, Austria). Rat liver mitochondria (0.5 mg/ml) were incubated in a buffer consisting of 105 mM KCl, 20 mM TRIS-HCl, 1 mM diethylenetriaminepentaacetic acid, 5 mM KH2PO4, and 1 mg/ml fatty acid-free bovine serum albumin (pH 7.4, 25°C). State 4 respiration was stimulated either by the addition of 5 mM glutamate plus 5 mM malate or 10 mM succinate in the presence of rotenone (1 μg/ml). The transition to state 3 respiration was induced by addition of 200 μM ADP. State 4 respiration was defined as oxygen consumption by isolated mitochondria on a particular substrate, in the absence of ADP, reflecting the integrity of the inner mitochondrial membrane. State 3 respiration was defined as ADP-stimulated respiration, reflecting ATP synthesis.
Gene Expression
RNA was extracted from corresponding liver specimens using TriReagent (Molecular Research Centre, USA). From total RNA, 1 μg was used for subsequent reverse transcription with Superscript (Invitrogen) and anchored oligo-dT-primers (3.5 μM final concentration). To check the generation of amplifiable cDNA in the reverse transcription, a conventional PCR step was performed using GAPDH-specific primers, as described elsewhere.30 Analysis of gene expression was performed by means of real-time PCR using specific primer pairs as described previously31 on an iCycler iQ™ (Bio-Rad, Hercules, CA, USA). PCR was carried out using iTaq™ polymerase™ (0.625 U/reaction; BioRad) with a final concentration of 200 μmol/l dNTP (each) and 3 mmol/l MgCl2 with the provided reaction buffer (1 × ) in a final volume of 25 μl. Each reaction well was loaded with primers (500 nmol/l each) and SYBR® GREEN I ( × 0.5, Sigma). All sequences of interest were amplified in parallel from one aliquot of cDNA on the same plate using the following PCR protocol: an initial Taq polymerase activating step at 95°C for 3 min followed by 40 cycles with a 20 s denaturation step at 92°C, a 30 s annealing step at 62°C, a 40 s extension step at 72°C and a 15 s step at 85°C during which data were collected. Quantification of the template concentration was achieved using standard curves and the built-in iCycler iQ Detection System Software, Version v3.1. To generate the standard, equal aliquots of the cDNA of all samples were pooled. For normalization, the values for the target sequence were averaged and calculated in relation to the arithmetic mean of the values obtained from four housekeeping genes (beta-actin, HPRT, GAPDH, and cyclophilin A).
ATP Determination
For the ATP assay, livers from control animals and rats treated with LPS were immediately excised after killing the animals, instantly frozen in liquid nitrogen, and stored at −80°C until measurement. In order to release cellular ATP, frozen liver tissue (40 mg) from rats treated with or without LPS was boiled for 2 min after the addition of 300 μl boiling buffer (100 mM TRIS-Cl (pH 7.75), 4 mM EDTA). Samples were put on ice and homogenized by sonication (micro tip, 1 × 10 s pulse). ATP concentrations were determined using the ATP bioluminescence assay kit HS II (Roche) according to the manufacturer's protocol. Data were standardized to the protein concentration, which was determined with the DC protein assay kit (Bio-Rad).
Iron Determination
Free iron concentration in liver tissue was measured by EPR spectroscopy as described in our previous publication32 using a nitrite assay: sodium nitrite (0.05 ml, 8.7 M) was added to 0.4–0.5 g of liver tissue and incubated at 20°C for 20 min. Nitric oxide (NO) produced from the reduction of sodium nitrite gives rise to a dinitrosyl iron complex with endogenous free iron characterized by an EPR absorption at g=2.04.33 Free iron concentration was calculated on a calibration plot obtained by adding incremental volumes of FeSO4*7H2O to tissue homogenate.
EPR Measurements
Plasma and red blood cells (RBC) were separated by centrifugation, placed in 1 ml syringes and frozen in liquid nitrogen. Low-temperature EPR spectra were recorded at liquid nitrogen temperature with a Bruker EMX EPR spectrometer (the general settings were: microwave frequency 9.431 GHz, modulation frequency 100 kHz, microwave power 20 mW, modulation amplitude 4 G; gain 105). In plasma, we determined the signal of transferrin at g=4.3. The intensity was determined as the peak-to-peak magnitude of the signal. In RBC, we determined NO–Hb complexes. The double integrals of NO–Hb signals were calculated and compared with those obtained from nitroso–heme complex standards. The preparation of nitroso–heme complex standards was performed as described earlier.34
Determination of Protein Levels of Transferrin and Hepcidin
All procedures were performed at room temperature under agitation. Two μl of plasma were spotted on nitrocellulose membranes (Trans-Blot Transfer Medium, Bio-Rad) and membranes were blocked overnight with 2% BSA in PBS. For detection of total transferrin, goat anti-rat transferrin antiserum (Alpha Diagnostic, USA) was diluted 1:2000 in PBST-BSA (PBS, 0.2% Tween 20, 0.2% BSA). For detection of total hepcidin, rabbit anti-mouse HEPC IgG (aff pure, Alpha Diagnostic) was used at a final concentration of 1 μg/ml. This antibody is highly (92%) conserved35 and suitable for studies on rats.31 Membranes were incubated with primary antibodies for 1 h in a total volume of 10 ml. After washing (3 × 5 min with PBST), the membranes were incubated with the appropriate secondary antibodies (anti-goat and anti-rabbit (Acvis Antibodies, Germany), respectively, both peroxidase conjugates, 1:5000 each in PBST-BSA) for 1 h. After final washing, membranes were incubated for 2 min with Lumi-Light Western-Blotting Substrate (Roche Diagnostics, Germany) and signals were detected with a CCD camera (Alpha Innotech Corporation, USA). Spots were quantified by densitometric measurement and expressed as integrated density value (IDV=AU).
Statistics
All data are presented as means±s.e.m. Statistical analysis was performed by one-way ANOVA test followed by post hoc test for least significant difference (LSD). Significance was based on a value of P<0.05. The calculations were made with the software SPSS 11.5 for Windows (SPSS Inc.) and MS Excel (Microsoft Corp.).
RESULTS
LPS-Mediated Body Response
The most important marker of sepsis, TNF-α, was already drastically increased at the mRNA level at 2 h after LPS challenge, and then gradually decreased (Figure 1a). Aspartate amino transferase (AST), a marker of liver mitochondrial damage, gradually increased, reaching maximum at 8 h (Figure 1b).
Effect of endotoxin on TNF-α and AST levels. Expression of TNF-α, an important marker of endotoxic shock, reached its highest level at 2 h. Plasma levels of the necrosis marker AST reached its highest level at 8 h. *Significant differences (P<0.05) between LPS treated groups and the control (0 h) are indicated.
Iron Content in Blood Plasma
The concentration of transferrin iron in plasma was unchanged during the first 4 h and significantly dropped down at 8 h and even more at 12 h (Figure 2a). The decrease of transferrin iron was not due to a decrease of protein, since the latter did not change within 12 h (Figure 2b), but was due to a decrease of iron content, and consequently a decrease of transferrin saturation. The levels of hepcidin mRNA were increased (see Figure 6) however hepcidin protein levels in blood were even decreased, suggesting that the observed changes in iron metabolism are not related to a hepcidin-mediated pathway (Figure 2c). Transferrin receptor mRNA levels were significantly increased 2 h after LPS challenge, but later they dropped below control values (Figure 2d).
Time course of proteins involved in iron transport in blood. The levels of transferrin-bound iron did not change in the first 4 h but were drastically decreased at 8 and 12 h (a), while the plasma concentration of transferrin protein was unchanged (b). Protein levels of hepicin in plasma showed a decrease at 2 h after LPS challenge (c). Expression of transferrin receptor temporarily increased at 2 h, was unchanged at 4 and 8 h, and was downregulated at 12 h (d). *Significant differences (P<0.05) between LPS treated groups and the control (0 h) are indicated.
Free Iron Levels in Liver and Expression of Inducible Heme Oxygenase
In contrast to our expectations, free iron levels in liver (Figure 3a) did not change during the first 2 h but increased at 4 and 8 h, followed by a decrease at 12 h (Figure 3b). Therefore, the kinetics of transferrin iron in plasma did not show a temporal relationship with free iron concentration in liver. In contrast a high correlation (Figure 3d) was found between the expression of inducible heme oxygenase (HO-1) (Figure 3c) and levels of free iron. At the same time, mRNA levels of ferritin and ferroportin, both responsible for decreasing the intracellular free iron pool either by sequestration or by elimination of iron out of the cell, were decreased (Figure 4a and b). These findings suggest that HO-1 could at least partly contribute to the increase of free iron.
Relationship between HO-1 expression and free iron levels in liver. Free iron signal (a) in liver increased reaching its highest (more than two-fold) levels at 4 and 8 h (b). Expression of HO-1 also reached its highest level at 4 and 8 h (c), demonstrating a good correlation with free iron levels (d). *Significant differences (P<0.05) between LPS treated groups and the control (0 h) are indicated.
Time course of proteins involved in free iron sequestration in liver. Expression of both proteins responsible for decreasing the levels of free iron, ferritin (a), and ferroportin (FPN, b) were downregulated after LPS challenge. *Significant differences (P<0.05) between LPS treated groups and the control (0 h) are indicated.
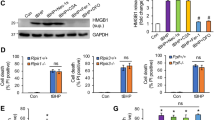
Mitochondrial Function
Respiratory control (RC) of mitochondria was elevated at 2 and 12 h and decreased between 4 and 8 h (Figure 5a). This was well correlated with the levels of ATP in liver tissue (Figure 5b). Addition of ferrous iron ions to isolated mitochondria from control liver tissue decreased RC value significantly (Figure 5c).
Effect of endotoxin in vivo and free iron in vitro on the function of liver mitochondria. Mitochondrial function (a) and ATP levels (b) as a function of time in livers of rats subjected to LPS challenge. Cellular energy in the form of ATP is 70% reduced 8 h later. Exogenously added iron ion reduces mitochondrial function about 50% (c). *Significant differences (P<0.05) between LPS treated groups and the control (0 h) are indicated.
DISCUSSION
TNF-α, a marker for inflammatory response to endotoxic shock, was already significantly upregulated at mRNA levels after 2 h, confirming a strong inflammatory reaction. Endotoxic inflammation was accompanied by increasing AST levels, suggesting damage to the liver. The AST levels reached maximum levels at 8 h. It is of note that at this time point, the mortality was approximately 30% and the observed decrease in AST levels at 12 h could be due to the fact that the surviving animals were less responsive to LPS. On average, the maximal response was observed at 8 h, indicating maximal tissue damage.
We observed a decrease in plasma levels of transferrin-bound iron, which have previously been reported in similar models.2, 7 This decrease was exclusively due to the iron saturation of transferrin, because the protein levels of transferrin were not changed (Figure 2). Infusion with LPS or the inflammatory cytokine IL-6 were shown to induce hepcidin mRNA in liver and to decrease the levels of circulating iron.36 However, since hepcidin protein was found to increase in urine, but not in plasma of subjects treated with LPS,37 a direct hormone-like action of hepcidin on distant tissues, like intestinal mucosa, could not yet be proven. Our own findings confirm the findings of the previous studies: determination of hepcidin mRNA in the liver from LPS-treated rats revealed moderately increased levels (Figure 6); however, hepcidin protein levels were not increased in the plasma at the indicated time points, but were even decreased. But probably, besides its indirect and delayed effects on the endocrine system and intestinal mucosa, hepcidin exerts predominantly local effects. Recently, it was reported that hepcidin acts by binding to ferroportin and causing its relocalization and loss of function.38 Therefore, we think that iron is retained within the cells due to a decreased availability of the iron exporter ferroportin.
We have found significantly decreased mRNA levels of ferroportin, the only protein exporting iron from the cell, in the livers of endotoxin-treated rats. A previous study has shown that ferroportin is downregulated at mRNA and protein levels in splenic macrophages after LPS administration in a mouse model.39 Therefore, we questioned whether this condition would have an impact on the levels of free iron in livers of LPS-treated rats.
We have found significantly increased levels of catalytically active, ‘free,’ iron at 4 and 8 h. They coincide with the increased levels of markers for tissue damage at this time point. These data provide a mechanistic rationale for previously published articles40, 41, 42, 43 reporting beneficial effects of the iron chelator desferioxamine in sepsis models. Notably, the increase in hepatic intracellular iron levels was not due to decreased levels of transferrin-bound iron in blood. At 4 h after LPS administration, iron levels were already significantly increased, but levels of circulating iron (transferring-bound iron) still remained unchanged. These findings suggest that the transient increase of free iron in livers of LPS-treated rats reported in our study is not mediated by hepcidin. Although a partial contribution to increased hepatic iron levels, due to a decreased export via ferroportin, cannot be excluded.
Recently, we have reported that in a similar rat model for endotoxic shock the levels of cytochrome p450 and its activity are drastically decreased.26 It was shown that inducible heme oxygenase (HO-1) is responsible for the degradation of p450 in stressful conditions.44 One of the products of this reaction is ferrous iron.
It is known that iron metabolism is regulated by IRP (iron responsive proteins) affecting among others ferritin and transferrin receptor at the mRNA level. Inflammation dramatically affects the iron metabolism and many inflammatory mediators act via the IRPs.45, 46 Thus, iron metabolism is expected to be modulated in our model, since cytokines and NO are produced upon LPS stimulation (increase of expression of TNF-α and inducible NO-synthase (iNOS) (data not shown)). In order to understand the source of the increased amount of free iron detected at 4 and 8 h after LPS challenge, we analyzed the pattern of iron metabolism associated gene expression, the overall result of upstream operating stimuli.
Our data show that there is a significant expression of HO-1, which correlates with increased free iron levels. Additionally, the mechanisms which prevent accumulation of free iron inside the cells, namely its elimination via ferroportin or an increased sequestration into ferritin, are apparently not operating in the liver at the early phase of endotoxic shock, since expression of both proteins is decreased.
Many studies show that induction of HO-1 confers cell protection in several pathologic conditions, including nitrosative stress.47, 48 Decomposition of heme by HO-1 is believed to downmodulate excess production of NO, since iNOS is a heme protein.36 However, heme degradation liberates ferrous iron. Therefore, HO-1 plays a pivotal role, and beneficial effects depend on the appropriate cellular control of the free iron pool.
Induction of HO-1 by extracellular heme was shown to increase the free iron pool relevant for its subsequent sequestration into ferritin.37 In endothelial cells, increased expression of HO-1 exerted an increased cytotoxicity due to elevated levels of catalytically active intracellular iron.39 This indicates that endotoxic shock temporarily creates a situation where more free iron might accumulate from increased HO-1 activity, which is not accordingly sequestered into ferritin or eliminated via ferroportin at this time. Irrespective of the source of these increased free iron levels, it was important to determine whether these increased iron levels can exert deleterious effects on cellular function. As mitochondria are considered an important target for pathological effects of LPS,20, 21, 24, 25, 38 we investigated mitochondrial function.
We observed that one of the most important markers of mitochondrial function, so-called respiratory control, is increased at 2 h after LPS challenge, probably reflecting an adaptive reaction which has been described previously.24, 40, 41 However at 4 and particularly at 8 h, RC was significantly decreased, recovering at 12 h. This is in line with reports showing impaired mitochondrial function at 4 h after LPS challenge in feline,20 and improved mitochondrial function at 16 h in rats.17, 40 We show that both a decrease in RC at 4 h and an increase later on is also valid for rats. However, the impairment of mitochondrial function at 4 h is only temporary. It is known that iron overload can impair mitochondrial function.42, 43 To investigate whether the levels of free iron we have detected at 4 and 8 h post LPS-challenge in liver tissue are sufficient to decrease mitochondrial function, we added to control mitochondria a corresponding amount of exogenous ferrous iron. We observed a significant decrease in RC, confirming previous studies that excessive levels of free iron impair mitochondrial function. Therefore, we here present a novel mechanism possibly involved in endotoxin-induced tissue damage mediated by increased levels of intracellular iron.
We have observed that the most dramatic changes were observed at 8 h after LPS challenge, namely the highest levels of AST, coinciding with highest levels of intracellular free iron and impaired mitochondrial function.
Our findings suggest that the increase of free iron in liver mediated by endotoxin might be a result of increased HO-1 activity and that released iron likely impairs mitochondrial respiration and might further contribute to tissue damage and organ failure. Thus, this study provides a rationale for the use of iron chelators as a treatment of sepsis.
References
Schoenberg MH, Weiss M, Radermacher P . Outcome of patients with sepsis and septic shock after ICU treatment. Langenbecks Arch Surg 1998;383:44–48.
Liu P, McGuire GM, Fisher MA, et al. Activation of Kupffer cells and neutrophils for reactive oxygen formation is responsible for endotoxin-enhanced liver injury after hepatic ischemia. Shock 1995;3:56–62.
Messaris E, Antonakis PT, Memos N, et al. Deferoxamine administration in septic animals: improved survival and altered apoptotic gene expression. Int Immunopharmacol 2004;4:455–459.
Ritter C, Andrades ME, Reinke A, et al. Treatment with N-acetylcysteine plus deferoxamine protects rats against oxidative stress and improves survival in sepsis. Crit Care Med 2004;32:342–349.
Ritter C, da Cunha AA, Echer IC, et al. Effects of N-acetylcysteine plus deferoxamine in lipopolysaccharide-induced acute lung injury in the rat. Crit Care Med 2006;34:471–477.
Vulcano M, Meiss RP, Isturiz MA . Deferoxamine reduces tissue injury and lethality in LPS-treated mice. Int J Immunopharmacol 2000;22:635–644.
Kemna E, Pickkers P, Nemeth E, et al. Time-course analysis of hepcidin, serum iron, and plasma cytokine levels in humans injected with LPS. Blood 2005;106:1864–1866.
Weiss G . Modification of iron regulation by the inflammatory response. Best Pract Res Clin Haematol 2005;18:183–201.
Britton RS, Leicester KL, Bacon BR . Iron toxicity and chelation therapy. Int J Hematol 2002;76:219–228.
Pietrangelo A . Mechanism of iron toxicity. Adv Exp Med Biol 2002;509:19–43.
Aust SD, Morehouse LA, Thomas CE . Role of metals in oxygen radical reactions. J Free Radic Biol Med 1985;1:3–25.
Vladimirov YA, Olenev VI, Suslova TB, et al. Lipid peroxidation in mitochondrial membrane. Adv Lipid Res 1980;17:173–249.
Bullen JJ, Rogers HJ, Spalding PB, et al. Iron and infection: the heart of the matter. FEMS Immunol Med Microbiol 2005;43:325–330.
Taylor DE, Piantadosi CA . Oxidative metabolism in sepsis and sepsis syndrome. J Crit Care 1995;10:122–135.
Geller ER, Jankauskas S, Kirkpatrick J . Mitochondrial death in sepsis: a failed concept. J Surg Res 1986;40:514–517.
Taylor DE, Ghio AJ, Piantadosi CA . Reactive oxygen species produced by liver mitochondria of rats in sepsis. Arch Biochem Biophys 1995;316:70–76.
Taylor DE, Kantrow SP, Piantadosi CA . Mitochondrial respiration after sepsis and prolonged hypoxia. Am J Physiol 1998;275:L139–L144.
Mela-Riker L, Bartos D, Vlessis AA, et al. Chronic hyperdynamic sepsis in the rat. II. Characterization of liver and muscle energy metabolism. Circ Shock 1992;36:83–92.
Lu SM, Song SM, Liu JC, et al. Changes of proton transportation across the inner mitochondrial membrane and H+-ATPase in endotoxic shock rats. Chin J Traumatol 2003;6:292–296.
Crouser ED, Julian MW, Blaho DV, et al. Endotoxin-induced mitochondrial damage correlates with impaired respiratory activity. Crit Care Med 2002;30:276–284.
Crouser ED, Julian MW, Huff JE, et al. Abnormal permeability of inner and outer mitochondrial membranes contributes independently to mitochondrial dysfunction in the liver during acute endotoxemia. Crit Care Med 2004;32:478–488.
Kantrow SP, Taylor DE, Carraway MS, et al. Oxidative metabolism in rat hepatocytes and mitochondria during sepsis. Arch Biochem Biophys 1997;345:278–288.
Tanaka J, Kono Y, Shimahara Y, et al. A study of oxidative phosphorylative activity and calcium-induced respiration of rat liver mitochondria following living Escherichia coli injection. Adv Shock Res 1982;7:77–90.
Singer M, De Santis V, Vitale D, et al. Multiorgan failure is an adaptive, endocrine-mediated, metabolic response to overwhelming systemic inflammation. Lancet 2004;364:545–548.
Singer M, Brealey D . Mitochondrial dysfunction in sepsis. Biochem Soc Symp 1999;66:149–166.
Kozlov AV, Gille L, Miller I, et al. Opposite effects of endotoxin on mitochondrial and endoplasmic reticulum functions. Biochem Biophys Res Commun 2007;352:91–96.
Takemura S, Minamiyama Y, Toyokuni S, et al. Overexpression of CYP3A aggravates endotoxin-induced liver injury in hypophysectomized female rats. Hepatol Res 2007 (e-pub ahead of print).
Gao J, Zeng BX, Zhou LJ, et al. Protective effects of early treatment with propofol on endotoxin-induced acute lung injury in rats. Br J Anaesth 2004;92:277–279.
Staniek K, Nohl H . H2O2 detection from intact mitochondria as a measure for one-electron reduction of dioxygen requires a non-invasive assay system. Biochim Biophys Acta 1999;1413:70–80.
Duvigneau JC, Hartl RT, Teinfalt M, et al. Delay in processing porcine whole blood affects cytokine expression. J Immunol Methods 2003;272:11–21.
Goss JA, Seu P, Gao FQ, et al. Ischemia–reperfusion of rat liver modulates hepcidin in vivo expression. Liver Transpl 2005;11:800–806.
Kozlov AV, Yegorov DY, Vladimirov YA, et al. Intracellular free iron in liver tissue and liver homogenate: studies with electron paramagnetic resonance on the formation of paramagnetic complexes with desferal and nitric oxide. Free Radic Biol Med 1992;13:9–16.
Vanin AF, Chetverikov AG . Paramagnetic nitrosyl complexes of heme and nonheme iron. Biofizika 1968;13:608–615.
Kozlov AV, Bini A, Iannone A, et al. Electron paramagnetic resonance characterization of rat neuronal nitric oxide production ex vivo. Methods Enzymol 1996;268:229–236.
Pigeon C, Ilyin G, Courselaud B, et al. A new mouse liver-specific gene, encoding a protein homologous to human antimicrobial peptide hepcidin, is overexpressed during iron overload. J Biol Chem 2001;276:7811–7819.
Srisook K, Cha YN . Super-induction of HO-1 in macrophages stimulated with lipopolysaccharide by prior depletion of glutathione decreases iNOS expression and NO production. Nitric Oxide 2005;12:70–79.
Sheftel AD, Kim SF, Ponka P . Non-heme induction of heme oxygenase-1 does not alter cellular iron metabolism. J Biol Chem 2007;282:10480–10486.
Simonson SG, Welty-Wolf K, Huang YT, et al. Altered mitochondrial redox responses in gram negative septic shock in primates. Circ Shock 1994;43:34–43.
Suttner DM, Dennery PA . Reversal of HO-1 related cytoprotection with increased expression is due to reactive iron. FASEB J 1999;13:1800–1809.
Kozlov AV, Staniek K, Haindl S, et al. Different effects of endotoxic shock on the respiratory function of liver and heart mitochondria in rats. Am J Physiol 2006;290:G543–G549.
Suliman HB, Carraway MS, Welty-Wolf KE, et al. Lipopolysaccharide stimulates mitochondrial biogenesis via activation of nuclear respiratory factor-1. J Biol Chem 2003;278:41510–41518.
Britton RS, Ramm GA, Olynyk J, et al. Pathophysiology of iron toxicity. Adv Exp Med Biol 1994;356:239–253.
Ceccarelli D, Kozlov AV, Gallesi D, et al. The role of desferrioxamine chelatable iron in rat liver mitochondrial dysfunction in chronic dietary iron overload. Bioelectrochem Bioenerg 1997;42:169–174.
Schwartzman ML, Abraham NG, Carroll MA, et al. Regulation of arachidonic acid metabolism by cytochrome P-450 in rabbit kidney. Biochem J 1986;238:283–290.
Cairo G, Pietrangelo A . Nitric-oxide-mediated activation of iron-regulatory protein controls hepatic iron metabolism during acute inflammation. Eur J Biochem 1995;232:358–363.
Phillips JD, Kinikini DV, Yu Y, et al. Differential regulation of IRP1 and IRP2 by nitric oxide in rat hepatoma cells. Blood 1996;87:2983–2992.
Zhao S, Zhang Y, Gu Y, et al. Heme oxygenase-1 mediates up-regulation of adhesion molecule expression induced by peroxynitrite in endothelial cells. J Soc Gynecol Investig 2004;11:465–471.
Li MH, Cha YN, Surh YJ . Carbon monoxide protects PC12 cells from peroxynitrite-induced apoptotic death by preventing the depolarization of mitochondrial transmembrane potential. Biochem Biophys Res Commun 2006;342:984–990.
Acknowledgements
We thank Jeffrey Doan for comments on the manuscript. This study was partially supported by the Shock Society/Novo Nordisk Research Grant for Hemorrhagic Shock and Hemostasis 2006.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Duvigneau, J., Piskernik, C., Haindl, S. et al. A novel endotoxin-induced pathway: upregulation of heme oxygenase 1, accumulation of free iron, and free iron-mediated mitochondrial dysfunction. Lab Invest 88, 70–77 (2008). https://doi.org/10.1038/labinvest.3700691
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/labinvest.3700691
Keywords
This article is cited by
-
Heme oxygenase-1 inhibition promotes IFNγ- and NOS2-mediated control of Mycobacterium tuberculosis infection
Mucosal Immunology (2021)
-
Is Iron Accumulation a Possible Risk Factor for Sarcopenia?
Biological Trace Element Research (2018)
-
Differences in vulnerability of neurons and astrocytes to heme oxygenase-1 modulation: Implications for mitochondrial ferritin
Scientific Reports (2016)
-
Asthma as a disruption in iron homeostasis
BioMetals (2016)
-
Magnetite- and maghemite-induced different toxicity in murine alveolar macrophage cells
Archives of Toxicology (2014)