Abstract
Congenital deficiency of carnitine palmitoyltransferase (CPT) II has been known for at least 30 years now, and its phenotypic variability remains fascinating. Three distinct clinical entities have been described, the adult, the infantile, and the perinatal, all with an autosomal recessive inheritance pattern. The adult CPT II clinical phenotype is somewhat benign and requires additional external triggers such as high-intensity exercise before the predominantly myopathic symptoms are elicited. The perinatal and infantile forms involve multiple organ systems. The perinatal disease is the most severe form and is invariably fatal. The introduction of mass spectrometry to analyze blood acylcarnitine profiles has revolutionized the diagnosis of fatty acid oxidation disorders including CPT II deficiency. Its use in expanded neonatal screening programs has made presymptomatic diagnosis a reality. An increasing number of mutations are being identified in the CPT II gene with a distinct genotype-phenotype correlation in most cases. However, clinical variability in some patients suggests additional genetic or environmental modifiers. Herein, we present a new case of lethal perinatal CPT II deficiency with a rare missense mutation, R296Q (907G>A) associated with a previously described 25-bp deletion on the second allele. We review the clinical features, the diagnostic protocol including expanded neonatal screening, the treatment, and the biochemical and molecular basis of CPT II deficiency.
Similar content being viewed by others
Main
The carnitine palmitoyltransferase (CPT) enzyme system, in association with acyl-coenzyme A (CoA) synthetase and the carnitine-acylcarnitine translocase (CACT), plays an important role in the transfer of long chain fatty acids (LCFA) from the cytosolic compartment to the mitochondrial matrix, where β-oxidation occurs (Bieber, 1988). Two genetically distinct mitochondrial membrane-bound enzymes make up the CPT system. CPT I is located on the inner aspect of the outer mitochondrial membrane. This enzyme is physiologically inhibited by the high levels of malonyl-CoA that occur postprandially and thus regulates the entry of LCFA into the mitochondria (McGarry and Brown, 1997). CPT II, which is not inhibited by malonyl-CoA, is situated on the inner aspect of the inner mitochondrial membrane (Murthy and Pande, 1987).
CPT II deficiency was first reported by DiMauro and DiMauro (1973) in adults with exercise-induced rhabdomyolysis. It is an autosomal recessive disorder (Angelini et al, 1981; Meola et al, 1987) and is now regarded as one of the most common inherited disorders of lipid metabolism (Zierz, 1994). Isolated presentation in two successive generations has been reported, indicating a possible dominant inheritance (Mongini et al, 1991). Partial CPT II deficiency with an autosomal dominant inheritance pattern has also been reported (Ionasescu et al, 1980). The molecular basis for this presentation was not elucidated.
To date, three distinct CPT II-deficient phenotypes have been described in the literature, for which genotypic information is now available. The adult form, which was originally identified by DiMauro and DiMauro (1973), is the most common and usually presents in young adults with recurrent myoglobinuria. The symptoms are usually precipitated by heavy exercise, and to a lesser extent, by cold, infection, emotional distress, and/or fasting. Renal failure may be a complication in some cases (Demaugre et al, 1988). The infantile form, which usually presents in early childhood with fasting-induced hypoketotic hypoglycemia, liver failure, cardiomyopathy, and peripheral neuropathy, is potentially fatal, although treatable if diagnosed early (Hug et al, 1991; Taroni et al, 1992). The perinatal form is the least common clinical presentation of CPT II deficiency and is almost universally and rapidly fatal (Elpeleg et al, 2001; Gellera et al, 1992; North et al, 1995; Pierce et al, 1999; Taroni et al, 1994; Vladutiu et al, 2002b). The phenotypic variability of CPT II deficiency is fascinating. There is a significant degree of genotype-phenotype correlation at the severe and mild ends of the clinical spectrum. However, CPT II gene polymorphisms may modify the expression of the mutated genes, giving rise to varied clinical features in some cases.
We report a new case of perinatal CPT II deficiency with a rare missense mutation and we review the current and expanding literature on CPT II deficiency.
Biochemical Review of the Mitochondrial Carnitine System
The metabolic significance of the mitochondrial carnitine system in the pathway of β-oxidation of LCFA is well recognized. LCFA of chain lengths C14–C18 are activated at the outer mitochondrial membrane to acyl-CoA esters by long-chain acyl-CoA synthetase (Kerner and Hoppel, 2000; Rinaldo et al, 2002). However, the inner mitochondrial membrane is impermeable to the acyl-CoA esters (Fig. 1). The so-called “carnitine shuttle” regulates the flux of acyl-CoA esters into the mitochondria. The shuttle requires the use of three major proteins, namely, CPT I, CACT, and CPT II.
CPT I catalyzes the rate-limiting step in β-oxidation, which is the conversion of the acyl-CoAs and free carnitine to acylcarnitines and free CoAs. CPT I is up-regulated when intracellular levels of malonyl-CoA are low, as is seen with fasting. Its activity is physiologically inhibited by high levels of malonyl-CoA (Dai et al, 2000; Declercq et al, 1987; Rinaldo et al, 2002). CPT I is located in the outer mitochondrial membrane (Fig. 1). Both the catalytic and the malonyl-CoA binding sites are exposed to the cytosol, where acyl-CoA esters are initially formed. Alterations in the membrane lipid environment can change the conformation of the CPT I enzyme, exerting an effect on its long-chain acyl-CoA binding site (Fraser et al, 2001; Zammit et al, 1997).
Two isoforms of CPT I have been described, a liver isoform (CPT IA or L-CPT I) and a muscle isoform (CPT IB or M-CPT I). L-CPT I is also found in lung, pancreas, ovary, brain, spleen, intestine, kidney, and skin fibroblasts (McGarry and Brown, 1997). M-CPT I is found in tissues with high-energy utilization such as heart and skeletal muscle and is also present in adipose tissue. The liver isoform has a lower affinity for malonyl-CoA and a higher affinity for carnitine (Kerner and Hoppel, 2000). Full-length cDNA cloning of L-CPT I from rat liver has predicted a protein of 773 amino acids with a molecular mass of 88 kDa (Esser et al, 1993). There is 82% and 88% identity between the human and the rat L-CPT I nucleotide sequence and the predicted protein primary structure, respectively. The human M-CPT I gene has been mapped to chromosome 22q13.3, and the L-CPT I gene is located on chromosome 11q13 (Britton et al, 1995; 1997).
In the second step of the carnitine shuttle, acylcarnitines enter the mitochondrial matrix in exchange for free carnitine, using CACT, an integral inner mitochondrial membrane protein (Fig. 1). CACT differs from other mitochondrial metabolite transporters in that its action is bidirectional (Indiveri et al, 1994; Palmieri et al, 1996) (Fig. 1). In addition to its function in the mitochondrial fatty acid oxidation (FAO), this enzyme is also thought to be involved in the membrane transport of acyl groups of different chain lengths. This multifunctionality may be the reason why deficiency of this protein tends to be more severe than most other FAO disorders (Kerner and Hoppel, 1998). The human CACT gene has been mapped to chromosome 3p21.31. The protein is composed of 301 amino acids and has a molecular mass of 33 kDa (Huizing et al, 1997; Indiveri et al, 1997; Palmieri et al, 1996; Viggiano et al, 1997).
The last step of the carnitine system is catalyzed by CPT II, an enzyme located on the matrix side of the inner mitochondrial membrane (Hoppel and Tomec, 1972). This step involves reconverting the acylcarnitine esters to their respective acyl-CoAs, which are now primed substrates for the β-oxidation process (Kerner and Hoppel, 2000). The transcribed CPT II protein with a molecular mass of approximately 71 kDa is composed of 658 amino acids, which includes an N-terminal 25 amino acid mitochondrial targeting sequence that is cleaved upon import into the mitochondria (Brown et al, 1991; McGarry and Brown, 1997; Woeltje et al, 1990b). The CPT II gene is located on chromosome 1p32, and the enzyme is ubiquitously expressed in all tissues that require FAO as an energy-producing pathway (Gellera et al, 1994). No isoforms are known to exist.
Case Report
The proband, a male neonate, was delivered by Cesarean section at 35.5 weeks gestation. The indication for the Cesarean section was preterm labor with fetal hydrocephalus. The mother, a Caucasian primigravida, had an otherwise unremarkable medical and prenatal history.
The baby was in respiratory distress at birth and was intubated and admitted to the neonatal intensive care unit, where he received pulmonary surfactant that led to a temporary improvement in oxygenation. Echocardiography revealed normal heart anatomy with persistent pulmonary hypertension. Magnetic resonance imaging of the brain was consistent with Dandy-Walker Syndrome. A ventriculo-peritoneal shunt was inserted on the second day of his life.
The patient developed metabolic acidosis and hypotension on the third day of his life. Volume expanders and sodium bicarbonate were administered; however, the metabolic acidosis persisted. His hospital stay was further complicated by oliguria and hypocalcemia, which required intravenous calcium supplementation. On the fourth day of his life, the patient developed bradycardia, which was resistant to medical therapy. A pacemaker was inserted; however, his condition continued to deteriorate. He subsequently had a cardiac arrest and could not be resuscitated.
At autopsy, the baby weighed 3600 gm and his crown-heel length was 55.5 cm. Gross examination of the cardio-respiratory system revealed patent ductus arteriosus, mildly pale myocardium, and unremarkable lungs. Examination of the brain revealed marked hydrocephalus, polymicrogyria, and hypoplasia of the vermis. There were choroid plexus hemorrhages in the lateral and third ventricles. All of the ventricles were dilated. There were also subarachnoid and intraparenchymal hemorrhages. The other organ systems were unremarkable on macroscopic examination.
Microscopic examination of the heart showed numerous small fat vacuoles within the muscle fibers. A section of the liver showed extensive macrovesicular steatosis, centrilobular congestion, and extramedullary hematopoiesis. The hematoxylin and eosin–stained section of skeletal muscle was unremarkable; however, a subtle increase in the lipid content was evident on a frozen section stained with oil red O. The remaining organ systems revealed no histopathologic abnormalities. Electron microscopic examination of the liver, heart, and skeletal muscle demonstrated elevated lipid content and increased mitochondria.
Plasma amino acid quantification showed elevated phenylalanine, tyrosine, and methionine, consistent with hepatic dysfunction. A nonspecific elevation of many other amino acids was also seen. Urine organic acid analysis revealed elevated lactic acid and 4-hydroxyphenyllactic acids. Plasma carnitine analysis showed normal total carnitine with low free carnitine and an elevated acylcarnitine to free carnitine ratio (free carnitine was 7 μmol/L; expected 38 ± 21). The plasma acylcarnitine profile showed markedly elevated long-chain species, especially C16 and C18:1, in association with low acetyl signal (Table 1).
FAO studies performed on fibroblasts, using the method of Manning et al, (1990), revealed a profound defect in LCFA oxidation (Fig. 2). CPT II assay (Esser et al, 1993) revealed reduced enzyme activity, which was 7% of the activity in control fibroblast samples (Fig. 3).
After enzymatic confirmation of the defect, a prenatal investigation was performed on cultured amniotic fluid cells in a subsequent pregnancy. The CPT II activity was found to be 50% of that in non-CPT II–deficient control amniocytes, and a heterozygous fetus was predicted.
Mutational analysis in the proband revealed a rare R296Q mutation on one allele and a 534T insdel25, an insertion that results in a 25-bp deletion on the other allele. R296Q mutation was not seen in 100 alleles in our population, and previous association of the latter mutation with severe CPT II deficiency strongly suggests that these are the disease-causing mutations. The patient was also homozygous for the V368I polymorphism.
Clinical and Metabolic Features of CPT II Deficiency
As previously mentioned, three distinct clinical presentations of CPT II deficiency have been described. It seems that the amount of residual enzymatic activity dictates the different clinical phenotypes, although some authors disagree (Elpeleg et al, 2001; Martin et al, 1999).
The adult form typically presents in early adulthood with muscle pain and myoglobinuria, usually after physical exercise (Bank et al, 1975; Cumming et al, 1976; DiMauro and DiMauro, 1973; Faigel, 1995; Scholte et al, 1979; Villard et al, 1996). Other precipitants may include, but are not limited to, infection, fasting, cold, increased fat intake, emotional distress, and certain drugs (Kelly et al, 1989; Kottlors et al, 2001; Reza et al, 1978; Wallace et al, 2001). The clinical features of the adult form have occasionally been reported to occur in childhood, as in the case of a 6-year-old girl who presented with acute muscle weakness, pain, and inability to walk. She had been symptomatic since the age of 2 years and was homozygous for the S113L (338C>T) mutation that is commonly associated with the adult form of the disease (Gempel et al, 2001). A similar case presenting at 8 months of age was reported by Hurvitz et al (2000). Two cases of CPT II deficiency presenting in adolescence with migraine headache have been reported (Kabbouche et al, 2003). Rare manifestations include recurrent pancreatitis after prolonged episodes of physical exercise and increased fat intake, permanent muscle weakness, and convulsions including status epilepticus (Gieron and Korthals, 1987; Shintani et al, 1995; Tein et al, 1994). Cardiac arrest may occur after strenuous exercise (Ratliff et al, 2002). Patients are usually asymptomatic between attacks, which vary greatly in frequency. Marked elevation of creatine kinase level is seen in 86% of the patients (Martin et al, 1999). Chronic fatigue and persistently elevated serum creatine kinase levels were the predominant features in one case of combined CPT II deficiency and the mitochondrial complex I defect (Tsao and Mendell, 2002). However, in most cases, serum creatine kinase levels are normal during intercritical phases and this is an important clue to a metabolic myopathy. Metabolic studies of an adult patient, homozygous for the S113L mutation, showed severe insulin resistance (Haap et al, 2002). Residual metabolic flux, as measured by the rate of [9,10-3H]myristate oxidation in cultured fibroblasts from patients with adult-onset CPT II deficiency, is usually approximately 50% of that in fibroblasts from normal controls, whereas CPT II activity ranges from 15% to 26% of normal (Bonnefont et al, 1996). Recent evidence suggests that both residual flux and enzyme activity may be even lower when measured at 41° C than at 37° C (Olpin et al, 2002). The prognosis is generally favorable, although fatalities have been reported (Kelly et al, 1989).
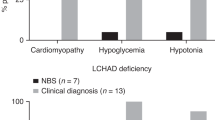
The infantile form of CPT II deficiency usually manifests between 6 months and 2 years of age with hypoketotic hypoglycemia, hepatomegaly, and raised plasma creatine kinase levels (Bonnefont et al, 1999; Demaugre et al, 1991). Cardiac manifestations include dilated hypertrophic cardiomyopathy and arrhythmias (Demaugre et al, 1991; Taroni et al, 1992; Vianey-Saban et al, 1995). Other clinical and laboratory features may include episodic weakness, encephalopathy, seizures, respiratory distress, metabolic acidosis, increased serum aminotransferase and ammonia, and decreased serum carnitine (Elpeleg et al, 1993; Ross et al, 1996; Taroni et al, 1992). In this group of patients, CPT II activity in fibroblasts ranges from 4% to 10% of the activity in control fibroblasts (Demaugre et al, 1991; Elpeleg et al, 1993). [9,10-3H]Myristate oxidation in fibroblasts is usually less than 10% of the control values (Bonnefont et al, 1996).
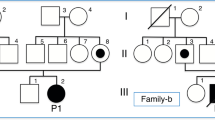
The perinatal form of CPT II deficiency has only been reported in a few cases. This presentation is fatal, leading to death in the neonatal period as was observed in our case (Albers et al, 2001a; Elpeleg et al, 2001; Gellera et al, 1992; Hug et al, 1991; Land et al, 1995; North et al, 1995; Pierce et al, 1999; Sharma et al, 2003; Smeets et al, 2003; Taroni et al, 1994; Vladutiu et al, 2002b; Witt et al, 1991; Zinn et al, 1991). Pregnancy may be complicated by oligohydramnios, and prenatal screening may show malformations including large ventricles, agenesis of the corpus callosum, intraventricular calcifications, and cystic dysplasia of the brain and the kidneys (Elpeleg et al, 2001; North et al, 1995). The patients are usually symptomatic at birth or within the first four days of life. In addition to dysmorphia, the clinical features include nonketotic hypoglycemia, metabolic acidosis, seizures, arrhythmias, nephromegaly, hepatomegaly, and cardiomegaly with cardiomyopathy (Elpeleg et al, 2001; North et al, 1995; Pierce et al, 1999). Central nervous system anomalies include ventriculomegaly, periventricular cysts, subarachnoid and subependymal hemorrhages, calcifications, and polymicrogyria, which is thought to result from abnormal neuronal migration. One patient of CPT II with perinatal myopathic illness without organomegaly or cardiovascular abnormalities has been reported, who died at approximately 34 days of life (Land et al, 1995). The residual LCFA oxidation in fibroblasts of patients with perinatal onset CPT II deficiency is less than 2%, and there is barely detectable CPT II activity in any of the tissues (Elpeleg et al, 2001).
Pathophysiology of CPT II Deficiency
Despite all of the studies done on CPT II deficiency, little is understood about the pathogenesis of the disorder. Suggestions have been made that certain stressors adversely impair energy metabolism in muscle in CPT II-deficient individuals (Wallace et al, 2001). Muscle fibers have been noted to have the highest amount of lipid during normal exercise in healthy individuals. Thus, it is conceivable that in CPT II-deficient patients, lipid will accumulate in stressed muscle (Nelson et al, 1990). There is evidence that the S113L mutation leads to a thermolabile CPT II protein whose activity is reduced when body temperature is high, as with exercise, febrile illness, or heat stress (Olpin et al, 2002). In later-onset disease, the skeletal muscle is primarily affected, whereas the other organ systems are spared. This is probably due to the fact that the residual enzymatic activity is able to maintain sufficient FAO for ketogenesis in the liver. In the infantile and perinatal forms, the residual activity of CPT II is low. This leads to decreased β-oxidation and consequent hypoketotic hypoglycemia and systemic lipid accumulation.
Diagnosis
Diagnosis of CPT II deficiency is first suspected by the alert clinician who recognizes the symptomatology and orders appropriate investigations. In the adult form, serum creatine kinase levels may be decreased, normal, or persistently elevated with further increase during periods of metabolic decompensation as an indicator of muscle involvement (Tsao and Mendell, 2002). The urine may be brown because of myoglobinuria. Serum myoglobin levels are elevated in some cases (Shintani et al, 1995). There may be elevated levels of serum creatinine and blood urea nitrogen, and acute renal failure may occur (Berkman et al, 1993; Demaugre et al, 1988; Kelly et al, 1989; Shintani et al, 1995; Villard et al, 1996). Hypocalcemia may occur because of muscle necrosis. Electromyography may demonstrate muscle injury; however, results can be normal in some cases (Kelly et al, 1989; Mongini et al, 1991). In the infantile form, marked hypoglycemia and hypoketonuria caused by deficient hepatic ketogenesis are common findings (Demaugre et al, 1988).
Hepatic steatosis is a common finding in both infantile and perinatal forms. Although increased lipid content may be seen in some cases on frozen sections of skeletal muscle stained with oil red O, it is not unusual to have normal skeletal muscle biopsy specimens (Cumming et al, 1976; Scholte et al, 1979). Electron microscopy, however, demonstrates increased skeletal muscle lipid in most cases (Elpeleg et al, 1993; Kelly et al, 1989; Mongini et al, 1991). The organic acid screen may show a nonspecific organic aciduria indicative of liver disease as seen in our patient or increased excretion of long-chain dicarboxylic acids (Fontaine et al, 1998). In the cases presenting earlier in life, the total blood carnitine levels are often decreased, with higher than normal levels of acylcarnitine, so that the acylcarnitine to free carnitine ratio is increased. In the adult CPT II deficiencies, carnitine levels are less predictable. Acylcarnitine analysis using tandem mass spectrometry may show elevated long chain (C16 and C18:1) acylcarnitines with low C2 signal (Gempel et al, 2001). LCFA oxidation studies can be performed on cultured fibroblasts, utilizing [9,10-3H]palmitate and [9,10-3H]myristate (Taroni et al, 1992). The residual flux through the FAO pathway correlates well with the severity of the disease. CPT II activity can be measured using 50- to 100-mg frozen skeletal muscle tissue (Hargreaves et al, 2000). Mutation analysis can be performed on skeletal muscle, blood, fibroblasts, and lymphoblasts. Dried whole blood on filter paper has been used successfully and is fast and economical (Smail et al, 1999).
Tandem mass spectrometry has emerged as a noninvasive and rapid method of detecting CPT II deficiency (Gempel et al, 1999; Videen et al, 1999). The first perinatal case of CPT II deficiency to be detected by tandem mass spectrometry through expanded newborn screening was reported in 2001 (Albers et al, 2001b). The use of tandem mass spectrometry in expanded newborn screening programs has positively impacted our diagnostic capability in the newborn period and has been successfully demonstrated for several metabolic disorders including some from the FAO pathway such as medium-chain acyl-CoA dehydrogenase deficiency (Naylor and Chace, 1999). Routine newborn screening has been adopted in several states in the United States and at the national level in several countries. There are also a number of private laboratories offering a fee-for-service program for this type of assay (Jones and Bennett, 2002; Levy and Albers, 2000). Within the United States, the New England consortium seems to provide an excellent working model, which addresses important aspects of management (Albers et al, 2001a; Gempel et al, 2002). The method is highly sensitive and specific (Wiley et al, 1999). Although perinatal CPT II deficiency is almost invariably fatal, early diagnosis is still useful. Presently, there is minimal data on the utility of newborn screening for nonperinatal CPT II deficiency. It seems likely that the infantile form of the disease should be detectable with good sensitivity. Late-onset CPT II deficiency may have much lower excretion of diagnostic acylcarnitines because of the high residual enzyme activity. We do not know how sensitive current screening assays are for this disease. Rettinger et al (2002) described a method using tandem mass spectrometry to determine the CPT II activity in muscle biopsy specimens.
Molecular Basis of CPT II Deficiency and Genotype-Phenotype Correlation
The CPT II gene has been cloned (Finocchiaro et al, 1991; Verderio et al, 1995) and assigned to chromosome 1p32 (Gellera et al, 1994). The gene contains five exons with a range of 81 to 1305 bp in length and spans 20 kilobases (Woeltje et al, 1990a). The unusually long exon 4 codes for more than half of all of the translated sequences of the gene (Verderio et al, 1995). More than 25 mutations have been described (Table 2). Most mutations are missense mutations and are found in exons 1, 3, 4, and 5.
The S113L is the most common mutation in the late adult form and is prevalent in populations of Southern European origin (Bonnefont et al, 1996; Handig et al, 1996; Taroni et al, 1993; Weiser et al, 2003; Yang et al, 1998b; Zierz et al, 1994). There are some case reports of children with this mutation who present with myopathic features of the adult form of the disease (Gempel et al, 2001). CPT II deficiency may manifest clinically even in a person heterozygous for the S113L mutation (Kaufmann et al, 1997; Taggart et al, 1999; Taroni et al, 1993). Compound heterozygosity may cause intermediate disease, as in the case of the S113L and the R631C (1897C>T) causing earlier presentation of the adult myopathic type. S113L in association with E487K (1459G>A) was reported in a 13 year old with the adult phenotype. The patient had been symptomatic since 8 years of age (Bruno et al, 2000; Taroni et al, 1993). The allelic frequency of the S113L mutation in European patients is 60% (Taroni et al, 1993).
The P50H (149C>A) causes a significant decrease in CPT II activity by altering the stability of the CPT II protein and is also associated with the adult form of disease (Verderio et al, 1995). The D553N (1657G>A) mutation, which is rare, involves substitution of an acidic amino acid (aspartic acid) with a neutral one (asparagine) and leads to an unstable protein. Heterozygous D553N, in association with the S113L mutation, has been reported in a patient with the adult phenotype (Verderio et al, 1995). The R503C (1507C>T), and G549D (1646G>A) substitutions are located in highly conserved regions of all CPT genes. The R503C mutation, which is lethal in the homozygous state, is known to cause clinical symptoms in the simple heterozygous form (Taggart et al, 1999; Vladutiu et al, 2000).
The Y628S (1883A>C) mutation results in severe impairment of the CPT II protein stability and is associated with the infantile type (Bonnefont et al, 1996). The R631C mutation also decreases the protein stability. This mutation is also associated with the infantile form of CPT II deficiency (Taroni et al, 1992); however, it has been associated with the adult phenotype in a separate report (Toscano et al, 1996). A combination of the E174K (520G>A) mutation, which extends the length of the α-helix, and the F383Y (1148T>A) mutation, which changes the direction of the turn, have so far only been associated with the Japanese population and result in infantile disease when homozygous (Akanuma et al, 1997; Wataya et al, 1998; Yamamoto et al, 1996).
The R124Stop (370C>T) mutation in exon 4 creates a stop codon at residue 124 of the protein leading to premature termination in translation (Yang et al, 1998a). In the L178F;N179_I186del (533_534insT;534_558del) mutation (seen on one allele of our patient), phenylalanine is substituted for leucine and this is followed by a 25-bp deletion (Yang et al, 1998b). The Q550R (1649A>G), R151Q (452G>A), P604S (1810C>T) substitutions (Yang et al, 1998b), the P227L (680C>T) mutation (Taroni et al, 1994; Yang et al, 1998b), the F448L (1342T>C) on exon 4, the Y479F (1436A>T), and the M214T (641T>C) substitutions (Weiser et al, 1997) are disease causing.
The Q413fs (1238_1239 delAG) mutation encodes an unstable truncated protein. The 413delAG-F448L haplotype is found predominantly in the Ashkenazi Jewish population and is associated with the antenatal presentation when homozygous (Elpeleg et al, 2001; Taggart et al, 1999). The fatal perinatal phenotype has been reported in five siblings in an isolated Moroccan family. Genomic studies showed compound heterozygosity for the 534T ins/del 25 mutation and a G>A splice mutation. This mutation, which is located in the intron 2 splice-acceptor site, was the first of its kind to be reported (Smeets et al, 2003). The L302fs (907_918ins) results in premature termination of the protein and truncation by about 350 amino acids and is also associated with the perinatal phenotype (Gellera et al, 1992).
Phenotypic variability has been known to occur in siblings with the same genotype (Handig et al, 1996; Vladutiu et al, 2002a), suggesting other environmental or genetic factors may play a role in the predisposition to disease severity. Although the genotype has clearly been associated with disease severity in many cases of CPT II deficiency, it is becoming accepted that the best predictive indicator may be the residual level of LCFA oxidation, typically performed in cultured cells (Thuillier et al, 2000).
Three polymorphisms have been described, the V368I (1203G>A), for which our patient was homozygous, the M647V (2040A>G) substitution (Taroni et al, 1992), and the F352C (1571T>G) substitution, which is predominantly found in the Japanese population (Wataya et al, 1998). In some cases the polymorphisms have been found to exacerbate the effect of some mutations (Taroni et al, 1992), whereas in other cases they seem to have no effect (Taroni et al, 1993). However, they are not pathologic by themselves. The V368I and the M647V polymorphisms are commonly associated with the S113L mutation. In Southern European populations, the allelic frequencies of V368I and M647V are V1 = 0.49 and V2 = 0.51 and M1 = 0.75 and M2 = 0.25, respectively (Verderio et al, 1993; 1995). The F352C polymorphism does not seem to have an effect on the CPT II activity (Wataya et al, 1998).
Treatment
Glucose remains the mainstay therapy in the management of CPT II deficiency. Intravenous glucose infusions have been shown to be beneficial in improving exercise tolerance, whereas oral glucose has not (Orngreen et al, 2002). The intravenous glucose is thought to spare glycogenolysis in muscle through supplementation of carbohydrate combustion during the early stages of exercise (Orngreen et al, 2002). A medium-chain triglyceride diet has been shown to lower the triglyceride storage in an isolated case of CPT II deficiency; however, the long-term effects were not elucidated (Scott et al, 1991). Other authors have recommended avoidance of C12-fatty acids in the medium-chain triglycerides preparations in addition to tightly regulated doses (Schaefer et al, 1997). In some situations, treatment with medium-chain triglycerides has not altered the symptomatology (Carroll et al, 1978). Prolonged episodes of fasting should be avoided in these patients (Bougneres et al, 1981). During labor, in an affected mother, adequate analgesia in addition to glucose infusions and close monitoring of serum creatine kinase level has been recommended (Moundras et al, 2000). In rats, theophylline has been shown to increase cardiac and renal CPT activity by an unknown mechanism (Alhomida, 2001). It is important to note that valproic acid, a drug commonly used in the treatment of pediatric convulsions, has been shown to trigger acute rhabdomyolysis in CPT II deficiency and is contraindicated (Kottlors et al, 2001). Thus it is imperative to rule out this disorder before therapy with this drug is initiated or to use an alternative drug if the situation permits.
References
Akanuma J, Wataya K, Matsubara Y, and Narisawa K (1997). Identification of missense mutations and haplotyping of carnitine palmitoyltransferase II gene. Nippon Rinsho 55: 3297–3301.
Albers S, Marsden D, Quackenbush E, Stark AR, Levy HL, and Irons M (2001b). Detection of neonatal carnitine palmitoyltransferase II deficiency by expanded newborn screening with tandem mass spectrometry. Pediatrics 107: E103.
Albers S, Waisbren SE, Ampola MG, Brewster TG, Burke LW, Demmer LA, Filiano J, Greenstein RM, Ingham CL, Korson MS, Marsden D, Schwartz RC, Seashore MR, Shih VE, and Levy HL (2001a). New England Consortium: A model for medical evaluation of expanded newborn screening with tandem mass spectrometry. J Inherit Metab Dis 24: 303–304.
Alhomida AS (2001). Oral theophylline changes renal carnitine palmitoyltransferase activity in rats. Arch Med Res 32: 394–399.
Angelini C, Freddo L, Battistella P, Bresolin N, Pierobon-Bormioli S, Armani M, and Vergani L (1981). Carnitine palmitoyltransferase deficiency: Clinical variability, carrier detection and autosomal recessive inheritance. Neurology 31: 883–886.
Bank WJ, DiMauro S, Bonilla E, Capuzzi DM, and Rowland LP (1975). A disorder of muscle lipid metabolism and myoglobinuria: Absence of carnitine palmitoyltransferase. N Engl J Med 292: 443–449.
Berkman N, Meirow D, Katzir Z, and Bar-On H (1993). Acute renal failure due to carnitine palmitoyltransferase deficiency. J Intern Med 233: 295–297.
Bieber LL (1988). Carnitine. Annu Rev Biochem 57: 261–283.
Bonnefont JP, Demaugre F, Prip-Buus C, Saudubray JM, Brivet M, Abadi N, and Thuillier L (1999). Carnitine palmitoyltransferase deficiencies. Mol Genet Metab 68: 424–440.
Bonnefont JP, Taroni F, Cavadini P, Cepanec C, Brivet M, Saudubray JM, Leroux JP, and Demaupsie F (1996). Molecular analysis of carnitine palmitoyltransferase II deficiency with hepatocardiomuscular expression. Am J Hum Genet 58: 971–978.
Bougneres PF, Saudubray JM, Marsac C, Bernard O, Odievre M, and Girard J (1981). Fasting hypoglycemia resulting from hepatic carnitine palmitoyltransferase deficiency. J Pediatr 98: 742–746.
Britton CH, Mackey DW, Esser V, Foster DW, Burns DK, Yarnall DP, Froguel P, and McGarry JD (1997). Fine chromosome mapping of the genes for human liver and muscle carnitine palmitoyltransferase I (CPT IA and CPT IB). Genomics 40: 209–211.
Britton CH, Schultz RA, Zhang B, Esser V, Foster DW, and McGarry JD (1995). Human liver mitochondrial carnitine palmitoyltransferase I: Characterization of its cDNA and chromosomal localization and partial analysis of the gene. Proc Natl Acad Sci USA 92: 1984–1988.
Brown NF, Esser V, Gonzalez AD, Evans CT, Slaughter CA, Foster DW, and McGarry JD (1991). Mitochondrial import and processing of rat liver carnitine palmitoyltransferase II defines the amino terminus of the mature protein: Possibility of differential modification of the rat and human isoforms. J Biol Chem 266: 15446–15449.
Bruno C, Bado M, Minetti C, Cordone G, and DiMauro S (2000). Novel mutation in the CPT II gene in a child with periodic febrile myalgia and myoglobinuria. J Child Neurol 15: 390–393.
Carroll JE, Brooke MH, DeVivo DC, Kaiser KK, and Hagberg JM (1978). Biochemical and physiologic consequences of carnitine palmitoyltransferase deficiency. Muscle Nerve 1: 103–110.
Cumming WJ, Hardy P, Hudgson P, and Walls J (1976). Carnitine-palmitoyl-transferase deficiency. J Neurol Sci 30: 247–258.
Dai J, Zhu H, Shi J, and Woldegiorgis G (2000). Identification by mutagenesis of conserved arginine and tryptophan residues in rat liver carnitine palmitoyltransferase I important for catalytic activity. J Biol Chem 275: 22020–22024.
Declercq PE, Falck JR, Kuwajima M, Tyminski H, Foster DW, and McGarry JD (1987). Characterization of the mitochondrial carnitine palmitoyltransferase enzyme system. I. Use of inhibitors. J Biol Chem 262: 9812–9821.
Demaugre F, Bonnefont JP, Colonna M, Cepanec C, Leroux JP, and Saudubray JM (1991). Infantile form of carnitine palmitoyltransferase II deficiency with hepatomuscular symptoms and sudden death: Physiopathological approach to carnitine palmitoyltransferase II deficiencies. J Clin Invest 87: 859–864.
Demaugre F, Bonnefont JP, Mitchell G, Nguyen-Hoang N, Pelet A, Rimoldi M, Di Donato S, and Saudubray JM (1988). Hepatic and muscular presentations of carnitine palmitoyltransferase deficiency: Two distinct entities. Pediatr Res 24: 308–311.
Deschauer M, Chrzanowska-Lightowlers ZM, Biekmann E, Pourfarzam M, Taylor RW, Turnbull DM, and Zierz S (2003). A splice mutation in muscle carnitine palmitoyltransferase II deficiency. Mol Genet Metab 79: 124–128.
Deschauer M, Wieser T, Schroder R, and Zierz S (2002). A novel nonsense mutation (515del4) in muscle carnitine palmitoyltransferase II deficiency. Mol Genet Metab 75: 181–185.
DiMauro S and DiMauro PMM (1973). Muscle carnitine palmitoyltransferase deficiency and myoglobinuria. Science 182: 929–931.
Elpeleg ON, Hammerman C, Saada A, Shaag A, Golzand E, Hochner-Celnikier D, Berger I, and Nadjari M (2001). Antenatal presentation of carnitine palmitoyltransferase II deficiency. Am J Med Genet 102: 183–187.
Elpeleg ON, Joseph A, Branski D, Christensen E, Holme E, Demaugre F, Saudubray JM, and Gutman A (1993). Recurrent metabolic decompensation in profound carnitine palmitoyltransferase II deficiency. J Pediatr 122: 917–919.
Esser V, Britton CH, Weis BC, Foster DW, and McGarry JD (1993). Cloning, sequencing, and expression of a cDNA encoding rat liver carnitine palmitoyltransferase I: Direct evidence that a single polypeptide is involved in inhibitor interaction and catalytic function. J Biol Chem 268: 5817–5822.
Faigel HC (1995). Carnitine palmitoyltransferase deficiency in a college athlete: A case report and literature review. J Am Coll Health 44: 51–54.
Finocchiaro G, Taroni F, Rocchi M, Martin AL, Colombo I, Tarelli GT, and DiDonato S (1991). cDNA cloning, sequence analysis, and chromosomal localization of the gene for human carnitine palmitoyltransferase. Proc Natl Acad Sci USA 88: 661–665.
Fontaine M, Briand G, Largilliere C, Degand P, Divry P, Vianey-Saban C, Mousson B, and Vamecq J (1998). Metabolic studies in a patient with severe carnitine palmitoyltransferase type II deficiency. Clin Chim Acta 273: 161–170.
Fraser F, Padovese R, and Zammit VA (2001). Distinct kinetics of carnitine palmitoyltransferase I in contact sites and outer membranes of rat liver mitochondria. J Biol Chem 276: 20182–20185.
Gellera C, Verderio E, Floridia G, Finocchiaro G, Montermini L, Cavadini P, Zuffardi O, and Taroni F (1994). Assignment of the human carnitine palmitoyltransferase II gene (CPT1) to chromosome 1p32. Genomics 24: 195–197.
Gellera C, Witt DR, Verderio E, Cavadini P, DiDonato S, and Taroni F (1992). Molecular study of lethal neonatal carnitine palmitoyltransferase II (CPT II) deficiency (Abstract). Am J Hum Genet 51: A168.
Gempel K, Kiechl S, Hofmann S, Lochmuller H, Kiechl-Kohlendorfer U, Willeit J, Sperl W, Rettinger A, Bieger I, Pongratz D, Gerbitz KD, and Bauer MF (2002). Screening for carnitine palmitoyltransferase II deficiency by tandem mass spectrometry. J Inherit Metab Dis 25: 17–27.
Gempel K, Kottlors M, Jaksch M, Gerbitz KD, and Bauer MF (1999). Adult carnitine palmitoyltransferase II deficiency: Detection of characteristic carnitine esters in serum by tandem mass spectrometry. J Inherit Metab Dis 22: 941–942.
Gempel K, von Praun C, Baumkotter J, Lehnert W, Ensenauer R, Gerbitz KD, and Bauer MF (2001). “Adult” form of muscular carnitine palmitoyltransferase II deficiency: Manifestation in a 2-year-old child. Eur J Pediatr 160: 548–551.
Gieron MA and Korthals JK (1987). Carnitine palmitoyltransferase deficiency with permanent weakness. Pediatr Neurol 3: 51–53.
Haap M, Thamer C, Machann J, Tschritter O, Loblein K, Kellerer M, Schick F, Jacob S, Haring HU, and Stumvoll M (2002). Metabolic characterization of a woman homozygous for the Ser113Leu missense mutation in carnitine palmitoyltransferase II. J Clin Endocrinol Metab 87: 2139–2143.
Handig I, Dams E, Taroni F, Van Laere S, de Barsy T, and Willems PJ (1996). Inheritance of the S113L mutation within an inbred family with carnitine palmitoyltransferase enzyme deficiency. Hum Genet 97: 291–293.
Hargreaves IP, Heales SJR, Olpin SE, Morgan-Hughes JA, and Land JM (2000). The diagnosis of carnitine palmitoyltransferase II deficiency is now possible in small skeletal muscle biopsies. J Inherit Metab Dis 23: 352–354.
Hoppel CL and Tomec RJ (1972). Carnitine palmitoyltransferase: Location of two enzymatic activities in rat liver mitochondria. J Biol Chem 247: 832–841.
Hug G, Bove KE, and Soukup S (1991). Lethal neonatal multiorgan deficiency of carnitine palmitoyltransferase II. N Engl J Med 325: 1862–1864.
Huizing M, Iacobazzi V, Ijlst L, Savelkoul P, Ruitenbeek W, van den Heuvel L, Indiveri C, Smeitink J, Trijbels FJ, Wanders RJ, and Palmieri F (1997). Cloning of the human carnitine-acylcarnitine translocase carrier cDNA and identification of the molecular defect in a patient. Am J Hum Genet 61: 1239–1245.
Hurvitz H, Klar A, Korn-Lubetzki I, Wanders RJ, and Elpeleg ON (2000). Muscular carnitine palmitoyltransferase II deficiency in infancy. Pediatr Neurol 22: 148–150.
Ijlst L, Hendriksen AG, Ruiter JPN, and Wanders RJ (1999). Molecular basis of CPTII deficiency: Identification of 9 novel mutations (Abstract). J Inherit Metab Dis 22 (Suppl 1): A53.
Indiveri C, Iacobazzi V, Giangregorio N, and Palmieri F (1997). The mitochondrial carnitine carrier protein: cDNA cloning, primary structure and comparison with other mitochondrial transport proteins. Biochem J 321: 713–719.
Indiveri C, Tonazzi A, and Palmieri F (1994). The reconstituted carnitine carrier from rat liver mitochondria: Evidence for a transport mechanism different from that of other mitochondrial translocators. Biochim Biophys Acta 1189: 65–73.
Ionasescu V, Hug G, and Hoppel C (1980). Combined partial deficiency of muscle carnitine palmitoyltransferase and carnitine with autosomal dominant inheritance. J Neurol Neurosurg Psychiatry 43: 679–682.
Jones PM and Bennett MJ (2002). The changing face of newborn screening: Diagnosis of inborn errors of metabolism by tandem mass spectrometry. Clin Chim Acta 324: 121–128.
Kabbouche MA, Powers SW, Vockell AL, LeCates SL, and Hershey AD (2003). Carnitine palmitoyltransferase II (CPT II) deficiency and migraine headache: Two case reports. Headache 43: 490–495.
Kaufmann P, el-Schahawi M, and DiMauro S (1997). Carnitine palmitoyltransferase II deficiency: Diagnosis by molecular analysis of blood. Mol Cell Biochem 174: 237–239.
Kelly KJ, Garland JS, Tang TT, Shug AL, and Chusid MJ (1989). Fatal rhabdomyolysis following influenza infection in a girl with familial carnitine palmitoyltransferase deficiency. Pediatrics 84: 312–316.
Kerner J and Hoppel C (1998). Genetic disorders of carnitine metabolism and their nutritional management. Annu Rev Nutr 18: 179–206.
Kerner J and Hoppel C (2000). Fatty acid import into the mitochondria. Biochim Biophys Acta 1486: 1–17.
Kottlors M, Jaksch M, Ketelsen UP, Weiner S, Glocker FX, and Lucking CH (2001). Valproic acid triggers acute rhabdomyolysis in a patient with carnitine palmitoyltransferase type II deficiency. Neuromuscul Disord 11: 757–759.
Land JM, Mistry S, Squier M, Hope P, Ghadiminejad I, Orford M, and Saggerson D (1995). Neonatal carnitine palmitoyltransferase-2 deficiency: A case presenting with myopathy. Neuromuscul Disord 5: 129–137.
Levy HL and Albers S (2000). Genetic screening of newborns. Hum Genet 1: 139–177.
Manning NJ, Olpin SE, Pollitt RJ, and Webley J (1990). A comparison of [9,10-3H]palmitic and [9,10-3H]myristic acids for the detection of defects of fatty acid oxidation in intact cultured fibroblasts. J Inherit Metab Dis 13: 58–68.
Martin MA, Rubio JC, De Bustos F, del Hoyo P, Campos Y, Garcia A, Bornstein B, Cabello A, and Arenas J (1999). Molecular analysis in Spanish patients with muscle carnitine palmitoyltransferase deficiency. Muscle Nerve 22: 941–943.
Martin MA, Rubio JC, del Hoyo P, Garcia A, Bustos F, Campos Y, Cabello A, Culebras JM, and Arenas J (2000). Identification of novel mutations in Spanish patients with muscle carnitine palmitoyltransferase II deficiency. Hum Mutat 15: 579–580.
McGarry JD and Brown NF (1997). The mitochondrial carnitine palmitoyltransferase system: From concept to molecular analysis. Eur J Biochem 244: 1–14.
Meola G, Bresolin N, Rimoldi M, Velicogna M, Fortunato F, and Scarlato G (1987). Recessive carnitine palmitoyltransferase deficiency: Biochemical studies in tissue cultures and platelets. J Neurol 235: 74–79.
Mongini T, Doriguzzi C, Palmucci L, Chiado-Piat L, Maniscalco M, and Schiffer D (1991). Myoglobinuria and carnitine palmitoyltransferase deficiency in father and son. J Neurol 238: 323–324.
Moundras JM, Wattrisse G, Leroy B, Decocq J, and Krivosic-Horber R (2000). Anesthetic management of obstetrical labor in a parturient with muscular carnitine palmitoyltransferase deficiency. Ann Fr Anesth Reanim 19: 611–616.
Murthy MS and Pande SV (1987). Malonyl-CoA binding site and the overt carnitine palmitoyltransferase activity reside on the opposite sides of the outer membrane. Proc Natl Acad Sci USA 84: 378–382.
Naylor EW and Chace DH (1999). Automated tandem mass spectroscopy for mass newborn screening for disorders in fatty acid organic acid, and amino acid metabolism. J Child Neurol 14 (Suppl 1): S4–S8.
Nelson KR, Ray JM, Wilson D, and Davis DG (1990). Motor unit potential analysis in carnitine palmitoyltransferase deficiency. J Child Neurol 5: 350–351.
North KN, Hoppel CL, De Girolami U, Kozakewich HP, and Korson MS (1995). Lethal neonatal deficiency of carnitine palmitoyltransferase II associated with dysgenesis of the brain and kidneys. J Pediatr 127: 414–420.
Olpin SE, Afifi A, Clark S, Bonham JR, Dalton A, Leonard JV, Land J, Rahman S, Morriss AA, Turnbull D, and Pourfarzam M (2002). Mutation and biochemical analysis in carnitine palmitoyltransferase type II deficiency suggests complex genotype/phenotype interactions (Abstract). J Inherit Metab Dis 25 (Suppl 1): 78.
Orngreen MC, Olsen DB, and Vissing J (2002). Exercise tolerance in carnitine palmitoyltransferase II deficiency with IV and oral glucose. Neurology 59: 1046–1051.
Palmieri F, Bisaccia F, Capobianco L, Dolce V, Fiermonte G, Iacobazzi V, Indiveri C, and Palmieri L (1996). Mitochondrial metabolite transporters. Biochim Biophys Acta 1275: 127–132.
Pierce MR, Pridjian G, Morrison S, and Pickoff AS (1999). Fatal carnitine palmitoyltransferase II deficiency in a newborn: New phenotypic features. Clin Pediatr 38: 13–20.
Ratliff NB, Harris KM, Smith SA, Tankh-Johnson M, Gornick CC, and Maron BJ (2002). Cardiac arrest in a young marathon runner. Lancet 360: 542.
Rettinger A, Gempel K, Hofmann S, Gerbitz KD, and Bauer MF (2002). Tandem mass spectrometric assay for the determination of carnitine palmitoyltransferase II activity in muscle tissue. Anal Biochem 302: 246–251.
Reza MJ, Kar NC, Pearson CM, and Kark RA (1978). Recurrent myoglobinuria due to muscle carnitine palmitoyltransferase deficiency. Ann Intern Med 88: 610–615.
Rinaldo P, Matern D, and Bennett MJ (2002). Fatty acid oxidation disorders. Annu Rev Physiol 64: 477–502.
Ross B, Zucherberg AL, and Geraghty MT (1996). Carnitine palmitoyltransferase II (CPT II) deficiency presenting with hyperammonemia in an infant (Abstract). Am J Hum Genet Suppl 59: A379.
Schaefer J, Jackson S, Taroni F, Swift P, and Turnbull DM (1997). Characterization of carnitine palmitoyltransferases in patients with carnitine palmitoyltransferase deficiency: Implications for diagnosis and therapy. J Neurol Neurosurg Psychiatry 62: 169–176.
Scholte HR, Jennekens FG, and Bouvy JJ (1979). Carnitine palmitoyltransferase II deficiency with normal carnitine palmitoyltransferase I in skeletal muscle and leucocytes. J Neurol Sci 40: 39–51.
Scott TF, Virella-Lopes M, and Malone MJ (1991). Hypertriglyceridemia in carnitine palmitoyltransferase deficiency: Lipid profile and treatment with medium chain triglycerides. Muscle Nerve 14: 676–677.
Sharma R, Perszyk AA, Marangi D, Monteiro C, and Raja S (2003). Lethal neonatal carnitine palmitoyltransferase II deficiency: An unusual presentation of a rare disorder. Am J Perinatol 20: 25–32.
Shintani S, Shiigai T, and Sugiyama N (1995). Atypical presentation of carnitine palmitoyltransferase (CPT) deficiency as status epilepticus. J Neurol Sci 129: 69–73.
Smail D, Gambino L, Boles C, and Vladutiu GD (1999). Rapid, cost-effective gene mutation screening for carnitine palmitoyltransferase II deficiency using whole blood on filter paper. Clin Chem 45: 2035–2038.
Smeets RJ, Smeitink JA, Semmekrot BA, Scholte HR, Wanders RJ, and van Den Heuvel LP (2003). A novel splice site mutation in neonatal carnitine palmitoyltransferase II deficiency. J Hum Genet 48: 8–13.
Taggart RT, Smail D, Apolito C, and Vladutiu GD (1999). Novel mutations associated with carnitine palmitoyltransferase II deficiency. Hum Mut 13: 210–220.
Taroni F, Gellera C, Cavadini P, Baratta S, Lamantea E, Dethlefs S, DiDonato S, Reik RA, and Benke PJ (1994). Lethal carnitine palmitoyltransferase (CPT) II deficiency in newborns: A molecular genetic study (Abstract). Am J Hum Genet 55: A245.
Taroni F, Verderio E, Dworzak F, Willems PJ, Cavadini P, and DiDonato S (1993). Identification of a common mutation in the carnitine palmitoyltransferase II gene in familial recurrent myoglobinuria patients. Nat Genet 4: 314–320.
Taroni F, Verderio E, Fiorucci S, Cavadini P, Finocchiaro G, Uziel G, Lamantea E, Gellera C, and DiDonato S (1992). Molecular characterization of inherited carnitine palmitoyltransferase II deficiency. Proc Natl Acad Sci USA 89: 8429–8433.
Tein I, Christodoulou J, Donner E, and McInnes RR (1994). Carnitine palmitoyltransferase II deficiency: A new cause of recurrent pancreatitis. J Pediatr 124: 938–940.
Thuillier L, Rostane H, Droin V, Demaugre F, Brivet M, Kadhom N, Prip-Buus C, Gobin S, Saudubray JM, and Bonnefont JP (2003). Correlation between genotype, metabolic data, and clinical presentation in carnitine palmitoyltransferase 2 (CPT2) deficiency. Hum Mutat 21: 493–501.
Thuillier L, Sevin C, Demaugre F, Brivet M, Rabier D, Droin V, Aupetit J, Abadi N, Kamoun P, Saudubray JM, and Bonnefont JP (2000). Genotype/phenotype correlation in carnitine palmitoyltransferase II deficiency: Lessons from a compound heterozygous patient. Neuromuscul Disord 10: 200–205.
Toscano A, Baratta S, Rodolico C, Aguennouz M, Autunno M, Vita G, Messina C, Invernizzi F, and Taroni F (1996). Carnitine palmitoyltransferase II (CPT II) deficiency: Occurrence of the adult-onset muscular phenotype in a family with the infant-type Arg-631-Cys CPT II mutation (Abstract). J Neurol 243 (Suppl 2): A159.
Tsao CY and Mendell JR (2002). Combined partial deficiencies of carnitine palmitoyltransferase II and mitochondrial complex I presenting as increased serum creatine kinase level. J Child Neurol 17: 304–306.
Verderio E, Cavadini P, Montermini L, Wang H, Lamantea E, Finocchiaro G, DiDonato S, Gellera C, and Taroni F (1995). Carnitine palmitoyltransferase II deficiency: Structure of the gene and characterization of two novel disease-causing mutations. Hum Mol Genet 4: 19–29.
Verderio E, Cavadini P, Pandolfo M, DiDonato S, and Taroni F (1993). Two novel sequence polymorphisms of the human carnitine palmitoyltransferase II (CPT 1) gene. Hum Mol Genet 2: 334–335.
Vianey-Saban C, Stremler N, Paut O, Buttin T, Divry P, Zabot MT, Camboulives J, Mathieu M, and Mousson B (1995). Infantile form of carnitine palmitoyltransferase II deficiency in a girl with rapid fatal onset. J Inherit Metab Dis 18: 362–363.
Videen JS, Haseler LJ, Karpinski NC, and Terkeltaub RA (1999). Noninvasive evaluation of adult onset myopathy from carnitine palmitoyltransferase II deficiency using proton magnetic resonance spectroscopy. J Rheumatol 26: 1757–1763.
Viggiano L, Iacobazzi V, Marzella R, Cassano C, Rocchi M, and Palmieri F (1997). Assignment of the carnitine/acylcarnitine translocase gene (CACT) to human chromosome band 3p21.31 by in situ hybridization. Cytogenet Cell Genet 79: 62–63.
Villard J, Fischer A, Mandon G, Collombet JM, Taroni F, and Mousson B (1996). Recurrent myoglobinuria due to carnitine palmitoyltransferase II deficiency: Expression of the molecular phenotype in cultured muscle cells. J Neurol Sci 136: 178–181.
Vladutiu GD, Bennett MJ, Fisher NM, Smail D, Boriack R, Leddy J, and Pendergast DR (2002a). Phenotypic variability among first-degree relatives with carnitine palmitoyltransferase II deficiency. Muscle Nerve 26: 492–498.
Vladutiu GD, Bennett MJ, Smail D, Wong LJ, Taggart RT, and Lindsey HB (2000). A variable myopathy associated with heterozygosity for the R503C mutation in the carnitine palmitoyltransferase II gene. Mol Genet Metab 70: 134–141.
Vladutiu GD, Quackenbush EJ, Hainline BE, Albers S, Smail DS, and Bennett MJ (2002b). Lethal neonatal and severe late infantile forms of carnitine palmitoyltransferase II deficiency associated with compound heterozygosity for different protein truncation mutations. J Pediatr 141: 734–736.
Wallace RA, Klestov AC, and Kubler PA (2001). Emotional distress induced rhabdomyolysis in an individual with carnitine palmitoyltransferase deficiency. Clin Exp Rheumatol 19: 583–586.
Wataya K, Akanuma J, Cavadini P, Aoki Y, Kure S, Invernizzi F, Yoshida I, Kira J, Taroni F, Matsubara Y, and Narisawa K (1998). Two CPT2 mutations in three Japanese patients with carnitine palmitoyltransferase II deficiency: Functional analysis and association with polymorphic haplotypes and two clinical phenotypes. Hum Mutat 11: 377–386.
Weiser T, Deschauer M, Olek K, Hermann T, and Zierz S (2003). Carnitine palmitoyltransferase II deficiency: Molecular and biochemical analysis of 32 patients. Neurology 60: 1351–1353.
Weiser T, Deschauer M, and Zierz S (1997). Carnitine palmitoyltransferase II deficiency: Three novel mutations. Ann Neurol 42: 414.
Wiley V, Carpenter K, and Wilcken B (1999). Newborn screening with tandem mass spectrometry: 12 months experience in NSW Australia. Acta Pediatr 432 (Suppl): 48–51.
Witt DR, Theobald M, Santa-Maria M, Packman S, Townsend S, Sweetman L, Goodman S, Rhead W, and Hoppel C (1991). Carnitine palmitoyltransferase-type 2 deficiency: Two new cases and successful prenatal diagnosis. Am J Hum Genet 49: 109.
Woeltje KF, Esser V, Weis BC, Cox WF, Schroeder JG, Liao ST, Foster DW, and McGarry JD (1990b). Inter-tissue and inter-species characteristics of the mitochondrial carnitine palmitoyltransferase enzyme system. J Biol Chem 265: 10714–10719.
Woeltje KF, Esser V, Weis BC, Sen A, Cox WF, McPhaul MJ, Slaughter CA, Foster DW, and McGarry JD (1990a). Cloning, sequencing, and expression of a cDNA encoding rat liver mitochondrial carnitine palmitoyltransferase II. J Biol Chem 265: 10720–10725.
Yamamoto S, Abe H, Kohgo T, Ogawa A, Ohtake A, Hayashibe H, Sakuraba H, Suzuki Y, Aramaki S, Takayanagi M, Hasegawa S, and Niimi H (1996). Two novel mutations (Glu174 → Lys, Phe383 → Tyr) causing the “hepatic” form of carnitine palmitoyltransferase II deficiency. Hum Genet 98: 116–118.
Yang BZ, Ding JH, Dewese T, Roe D, He G, Wilkinson J, Day DW, Demaugre F, Rabier D, Brivet M, and Roe CR (1998b). Identification of four novel mutations in patients with carnitine palmitoyltransferase II deficiency. Mol Genet Metab 64: 229–236.
Yang BZ, Ding JH, Roe D, Demaugre F, Brivet M, and Roe CR (1997). Carnitine palmitoyltransferase II deficiency: Clinical forms and mutations. Proceeding, Seventh International Congress of Inborn Errors of Metabolism, Vienna, Austria, May 21 to 25, 1997, P202 (Abstract).
Yang BZ, Ding JH, Roe D, Dewese T, Day DW, and Roe CR (1998a). A novel mutation identified in carnitine palmitoyltransferase II deficiency. Mol Genet Metab 63: 110–115.
Zammit VA, Fraser F, and Corstorphine CG (1997). Regulation of mitochondrial outer-membrane carnitine palmitoyltransferase (CPT I): Role of membrane topology. Adv Enzyme Regul 37: 295–317.
Zierz S (1994). Carnitine palmitoyltransferase deficiency. In: Engel AG and Franzini-Armstrong C, editors. Mycology. New York: McGraw-Hill, 1577–1586.
Zierz S, Engel AG, and Olek K (1994). The Ser 113 Leu mutation in the carnitine palmitoyltransferase II gene in patients with muscle carnitine palmitoyltransferase deficiency. Muscle Nerve Suppl 1: S129.
Zinn AB, Zurcher VL, Kraus F, Strohl C, Walsh-Sukys MC, and Hoppel CL (1991). Carnitine palmitoyltransferase B (CPT B) deficiency: A heritable cause of neonatal cardiomyopathy and dysgenesis of the kidney. Pediatr Res 29: 73A.
Acknowledgements
Acknowledgements
We thank Drs. Jonathan Cohen and Sijing Niu of the Department of Internal Medicine and McDermott Center of the University of Texas Southwestern Medical Center for sequencing the CPT II gene, and Mr. Richard L. Boriack for enzyme analysis.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Sigauke, E., Rakheja, D., Kitson, K. et al. Carnitine Palmitoyltransferase II Deficiency: A Clinical, Biochemical, and Molecular Review. Lab Invest 83, 1543–1554 (2003). https://doi.org/10.1097/01.LAB.0000098428.51765.83
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1097/01.LAB.0000098428.51765.83
This article is cited by
-
Metabolomics Adaptation of Juvenile Pacific Abalone Haliotis discus hannai to Heat Stress
Scientific Reports (2020)
-
Mitochondrial membrane transporters and metabolic switch in heart failure
Heart Failure Reviews (2019)
-
Heat stroke with bimodal rhabdomyolysis: a case report and review of the literature
Journal of Intensive Care (2016)
-
Metabotypes with properly functioning mitochondria and anti-inflammation predict extended productive life span in dairy cows
Scientific Reports (2016)
-
Rhabdomyolysis and acute kidney injury in two children: Answers
Pediatric Nephrology (2013)