Abstract
Objective:
To describe conservative management of spontaneous intestinal perforation (SIP) in preterm infants using peritoneal needle aspiration (PNA).
Study design:
Monocentric retrospective review of SIP cases treated primarily by PNA between 1999 and 2015 (n=31).
Results:
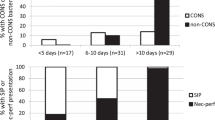
Mean gestational age was 29.2±2.4 weeks and birthweight 1149±428 g. SIP occurred at 3.7±2.2 days of life. PNA achieved definitive treatment in 18 patients (60%) with a mean of 1.8 (±0.8) procedures. All patients requiring more than three PNAs had secondary laparotomy. Two patients died and five presented severe cerebral lesions. Full enteral feeding was achieved 42±18 days after SIP. Intestinal morbidity included cholestasis (n=6), intestinal stricture (n=1) and growth restriction (n=22). On follow-up (n=25, median=4 years), no severe impairment was noted. Seventeen children (68%) had a normal development.
Conclusion:
PNA as primary therapy for SIP is a viable option, resulting in definitive treatment in 60% of cases, with limited mortality and morbidity.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
References
Wadhawan R, Oh W, Hintz SR, Blakely ML, Das A, Bell EF et al. Neurodevelopmental outcomes of extremely low birth weight infants with spontaneous intestinal perforation or surgical necrotizing enterocolitis. J Perinatol 2014; 34 (1): 64–70.
Pumberger W, Mayr M, Kohlhauser C, Weninger M . Spontaneous localized intestinal perforation in very-low-birth-weight infants: a distinct clinical entity different from necrotizing enterocolitis. J Am Coll Surg 2002; 195 (6): 796–803.
Attridge JT, Clark R, Walker MW, Gordon PV . New insights into spontaneous intestinal perforation using a national data set: (1) SIP is associated with early indomethacin exposure. J Perinatol 2006; 26 (2): 93–99.
Eicher C, Seitz G, Bevot A, Moll M, Goelz R, Arand J et al. Surgical management of extremely low birth weight infants with neonatal bowel perforation: a single-center experience and a review of the literature. Neonatology 2012; 101 (4): 285–292.
Emil S, Davis K, Ahmad I, Strauss A . Factors associated with definitive peritoneal drainage for spontaneous intestinal perforation in extremely low birth weight neonates. Eur J Pediatr Surg 2008; 18 (2): 80–85.
Ragouilliaux CJ, Keeney SE, Hawkins HK, Rowen JL . Maternal factors in extremely low birth weight infants who develop spontaneous intestinal perforation. Pediatrics 2007; 120 (6): e1458–e1464.
Buchheit JQ, Stewart DL . Clinical comparison of localized intestinal perforation and necrotizing enterocolitis in neonates. Pediatrics 1994; 93 (1): 32–36.
Fisher JG, Jones BA, Gutierrez IM, Hull MA, Kang KH, Kenny M et al. Mortality associated with laparotomy-confirmed neonatal spontaneous intestinal perforation: a prospective 5-year multicenter analysis. J Pediatr Surg 2014; 49 (8): 1215–1219.
Shah J, Singhal N, da Silva O, Rouvinez-Bouali N, Seshia M, Lee SK et al. Intestinal perforation in very preterm neonates: risk factors and outcomes. J Perinatol 2015; 35 (8): 595–600.
Wadhawan R, Oh W, Vohr BR, Saha S, Das A, Bell EF et al. Spontaneous intestinal perforation in extremely low birth weight infants: association with indometacin therapy and effects on neurodevelopmental outcomes at 18-22 months corrected age. Arch Dis Child Fetal Neonatal Ed 2013; 98 (2): F127–F132.
Blakely ML, Tyson JE, Lally KP, McDonald S, Stoll BJ, Stevenson DK et al. Laparotomy versus peritoneal drainage for necrotizing enterocolitis or isolated intestinal perforation in extremely low birth weight infants: outcomes through 18 months adjusted age. Pediatrics 2006; 117 (4): e680–e687.
Shah TA, Meinzen-Derr J, Gratton T, Steichen J, Donovan EF, Yolton K et al. Hospital and neurodevelopmental outcomes of extremely low-birth-weight infants with necrotizing enterocolitis and spontaneous intestinal perforation. J Perinatol 2012; 32 (7): 552–558.
Gordon PV . Understanding intestinal vulnerability to perforation in the extremely low birth weight infant. Pediatr Res 2009; 65 (2): 138–144.
Stark AR, Carlo WA, Tyson JE, Papile LA, Wright LL, Shankaran S et al. Adverse effects of early dexamethasone in extremely-low-birth-weight infants. National Institute of Child Health and Human Development Neonatal Research Network. N Engl J Med 2001; 344 (2): 95–101.
Kelleher J, Salas AA, Bhat R, Ambalavanan N, Saha S, Stoll BJ et al. Prophylactic indomethacin and intestinal perforation in extremely low birth weight infants. Pediatrics 2014; 134 (5): e1369–e1377.
Holland AJA, Shun A, Martin HCO, Cooke-Yarborough C, Holland J . Small bowel perforation in the premature neonate: congenital or acquired? Pediatr Surg Int 2003; 19 (6): 489–494.
Uceda JE, Laos CA, Kolni HW, Klein AM . Intestinal perforations in infants with a very low birth weight: a disease of increasing survival? J Pediatr Surg 1995; 30 (9): 1314–1316.
Blakely ML, Lally KP, McDonald S, Brown RL, Barnhart DC, Ricketts RR et al. Postoperative outcomes of extremely low birth-weight infants with necrotizing enterocolitis or isolated intestinal perforation: a prospective cohort study by the NICHD Neonatal Research Network. Ann Surg 2005; 241 (6): 984–989-994.
Cass DL, Brandt ML, Patel DL, Nuchtern JG, Minifee PK, Wesson DE . Peritoneal drainage as definitive treatment for neonates with isolated intestinal perforation. J Pediatr Surg 2000; 35 (11): 1531–1536.
Jakaitis BM, Bhatia AM . Definitive peritoneal drainage in the extremely low birth weight infant with spontaneous intestinal perforation: predictors and hospital outcomes. J Perinatol 2015; 35 (8): 607–611.
Sharma R, Tepas JJ, Mollitt DL, Pieper P, Wludyka P . Surgical management of bowel perforations and outcome in very low-birth-weight infants (< or =1,200 g). J Pediatr Surg 2004; 39 (2): 190–194.
Tepas JJ, Sharma R, Hudak ML, Garrison RD, Pieper P . Coming full circle: an evidence-based definition of the timing and type of surgical management of very low-birth-weight (<1000 g) infants with signs of acute intestinal perforation. J Pediatr Surg 2006; 41 (2): 418–422.
Stokes SM, Iocono JA, Draus JM . Peritoneal drainage as the initial management of intestinal perforation in premature infants. Am Surg 2014; 80 (9): 851–854.
Moss RL, Dimmitt RA, Barnhart DC, Sylvester KG, Brown RL, Powell DM et al. Laparotomy versus peritoneal drainage for necrotizing enterocolitis and perforation. N Engl J Med 2006; 354 (21): 2225–2234.
Rao SC, Basani L, Simmer K, Samnakay N, Deshpande G . Peritoneal drainage versus laparotomy as initial surgical treatment for perforated necrotizing enterocolitis or spontaneous intestinal perforation in preterm low birth weight infants. Cochrane Database Syst Rev 2011; 15 (6): CD006182.
Hunter CJ, Chokshi N, Ford HR . Evidence vs experience in the surgical management of necrotizing enterocolitis and focal intestinal perforation. J Perinatol 2008; 28 (Suppl 1): S14–S17.
Michel JL, Harper L, Alessandri JL, Jacquemot L, De Napoli-Cocci S, Pilorget H et al. Peritoneal needle suction for intestinal perforation in the preterm neonate. Eur J Pediatr Surg 2004; 14 (2): 85–88.
Khan RA, Narasimhan KL . Spontaneous intestinal perforation. Ann Ital Chir 2012; 83 (5): 437–439-440.
Chioukh F-Z, Ben Ameur K, Laamiri R, Ben Hmida H, Nouri A, Monastiri K . Spontaneous intestinal perforation in a very low birth weight infant: successful management by peritoneal needle suction. J Neonatal Surg 2016; 5 (3): 39.
Parry G, Tucker J, Tarnow-Mordi W, UK Neonatal Staffing Study Collaborative Group. CRIB II: an update of the clinical risk index for babies score. Lancet 2003; 361 (9371):1789–1791.
Mamelle N, Munoz F, Grandjean H . [Fetal growth from the AUDIPOG study. I. Establishment of reference curves]. J Gynecol Obstet Biol Reprod 1996; 25 (1): 61–70.
Jobe AH, Bancalari E . Bronchopulmonary dysplasia. Am J Respir Crit Care Med 2001; 163 (7): 1723–1729.
Papile LA, Burstein J, Burstein R, Koffler H . Incidence and evolution of subependymal and intraventricular hemorrhage: a study of infants with birth weights less than 1,500 gm. J Pediatr 1978; 92 (4): 529–534.
He T-Z, Xu C, Ji Y, Sun X-Y, Liu M . Idiopathic neonatal pneumoperitoneum with favorable outcome: a case report and review. World J Gastroenterol 2015; 21 (20): 6417–6421.
Khan RA, Mahajan JK, Rao KLN . Spontaneous intestinal perforation in neonates: is surgery always indicated? Afr J Paediatr Surg 2011; 8 (2): 249–251.
Rovin JD, Rodgers BM, Burns RC, McGahren ED . The role of peritoneal drainage for intestinal perforation in infants with and without necrotizing enterocolitis. J Pediatr Surg 1999; 34 (1): 143–147.
Rees CM, Eaton S, Kiely EM, Wade AM, McHugh K, Pierro A . Peritoneal drainage or laparotomy for neonatal bowel perforation? A randomized controlled trial. Ann Surg 2008; 248 (1): 44–51.
Bartoli F, Vasseur Maurer S, Giannoni E, Osterheld M-C, Laubscher B . [Focal spontaneous colic perforation in term or near-term neonates: rare and potentially insidious]. Arch Pediatr 2011; 18 (4): 408–412.
Tiwari C, Sandlas G, Jayaswal S, Shah H . Spontaneous intestinal perforation in neonates. J Neonatal Surg 2015; 4 (2): 14.
Naji A, Elkarout Y, Benajiba N . [Neonatal spontaneous gastric perforation: about a case]. Pan Afr Med J 2015; 21: 61.
Adesanya OA, O’Shea TM, Turner CS, Amoroso RM, Morgan TM, Aschner JL . Intestinal perforation in very low birth weight infants: growth and neurodevelopment at 1 year of age. J Perinatol 2005; 25 (9): 583–589.
Acknowledgements
Author contributions
All authors contributed to: conception and design of the study, analysis and interpretation of the data, drafting and revision of the article. All of them approved the final manuscript as submitted.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Gébus, M., Michel, JL., Samperiz, S. et al. Management of neonatal spontaneous intestinal perforation by peritoneal needle aspiration. J Perinatol 38, 159–163 (2018). https://doi.org/10.1038/jp.2017.170
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/jp.2017.170